J Korean Acad Prosthodont.
2018 Oct;56(4):278-286. 10.4047/jkap.2018.56.4.278.
Differences in percussion-type measurements of implant stability according to height of healing abutments and measurement angle
- Affiliations
-
- 1Department of Biomaterials and Prosthodontics, Kyung Hee University Dental School Hospital at Gangdong, Seoul, Republic of Korea. sbykmw@yahoo.co.kr
- 2Department of Prosthodontics, School of Dentistry, Kyung Hee University, Seoul, Republic of Korea.
- 3Department of Prosthodontics, Institute for Clinical Dental Research, Korea University Medical Center, Korea University, Seoul, Republic of Korea.
- KMID: 2424027
- DOI: http://doi.org/10.4047/jkap.2018.56.4.278
Abstract
- PURPOSE
The purpose of this study was to evaluate the effect of healing abutment height and measurement angle on implant stability when using Periotest and AnyCheck.
MATERIALS AND METHODS
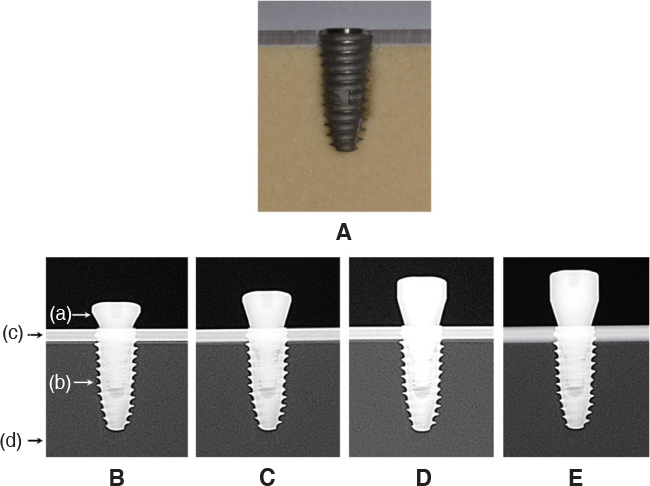
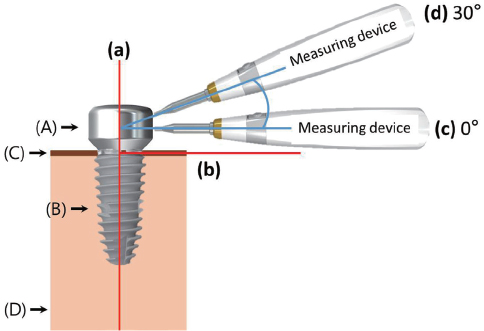
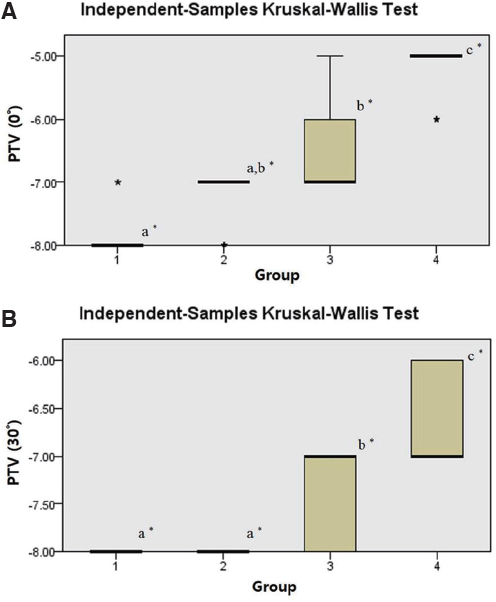
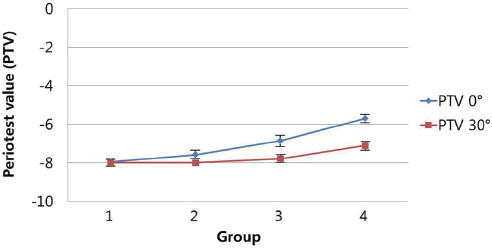
60 implants were placed into artificial bone blocks. After implant insertion, 2, 3, 4 and 5 mm healing abutments were installed on 15 specimens, respectively. Insertion torque value, implant stability test, Periotest value were measured. Insertion torque value was controlled between 45 - 55 Ncm. AnyCheck was used for measuring implant stability test and Periotest M was used for measuring Periotest value. Implant stability test and Periotest value were measured at the angles of 0 and 30 degrees to the horizontal plane. Measured values were analyzed statistically.
RESULTS
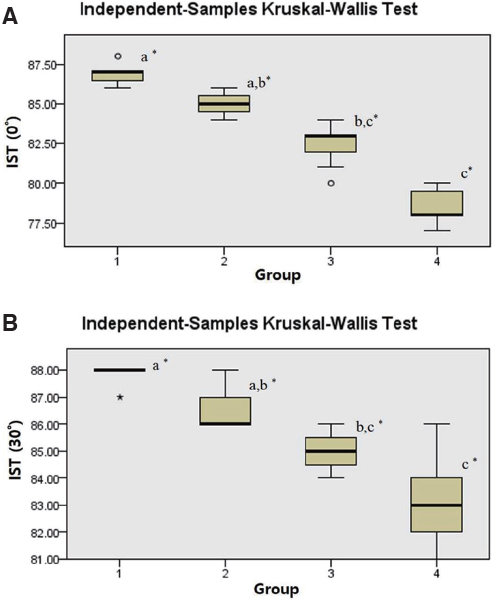
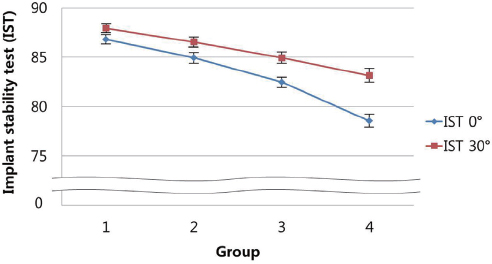
Insertion torque value had no significant difference among groups. When healing abutment height was higher, implant stability test and Periotest value showed lower stability. Also when measurement angle was decreased, implant stability test and Periotest value showed lower stability.
CONCLUSION
When measuring stability of implants with percussion type devices, measured values should be evaluated considering height of healing abutments and measurement angle.
Keyword
MeSH Terms
Figure
Reference
-
1. Raghavendra S, Wood MC, Taylor TD. Early wound healing around endosseous implants: a review of the literature. Int J Oral Maxillofac Implants. 2005; 20:425–431.2. Meredith N. Assessment of implant stability as a prognostic determinant. Int J Prosthodont. 1998; 11:491–501.3. Javed F, Romanos GE. The role of primary stability for successful immediate loading of dental implants. A literature review. J Dent. 2010; 38:612–620.
Article4. Elias CN, Rocha FA, Nascimento AL, Coelho PG. Influence of implant shape, surface morphology, surgical technique and bone quality on the primary stability of dental implants. J Mech Behav Biomed Mater. 2012; 16:169–180.
Article5. O'Sullivan D, Sennerby L, Meredith N. Measurements comparing the initial stability of five designs of dental implants: a human cadaver study. Clin Implant Dent Relat Res. 2000; 2:85–92.6. Ericsson I, Johansson CB, Bystedt H, Norton MR. A histomorphometric evaluation of bone-to-implant contact on machine-prepared and roughened titanium dental implants. A pilot study in the dog. Clin Oral Implants Res. 1994; 5:202–206.
Article7. Johansson CB, Sennerby L, Albrektsson T. A removal torque and histomorphometric study of bone tissue reactions to commercially pure titanium and Vitallium implants. Int J Oral Maxillofac Implants. 1991; 6:437–441.8. Wennerberg A, Albrektsson T, Andersson B, Krol JJ. A histomorphometric and removal torque study of screw-shaped titanium implants with three different surface topographies. Clin Oral Implants Res. 1995; 6:24–30.
Article9. Swami V, Vijayaraghavan V, Swami V. Current trends to measure implant stability. J Indian Prosthodont Soc. 2016; 16:124–130.
Article10. Huang HM, Chiu CL, Yeh CY, Lin CT, Lin LH, Lee SY. Early detection of implant healing process using resonance frequency analysis. Clin Oral Implants Res. 2003; 14:437–443.
Article11. Sennerby L, Meredith N. Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2000. 2008; 47:51–66.
Article12. Oh JS, Kim SG. Clinical study of the relationship between implant stability measurements using Periotest and Osstell mentor and bone quality assessment. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012; 113:e35–e40.
Article13. Atsumi M, Park SH, Wang HL. Methods used to assess implant stability: current status. Int J Oral Maxillofac Implants. 2007; 22:743–754.14. Faulkner MG, Giannitsios D, Lipsett AW, Wolfaardt JF. The use and abuse of the Periotest for 2-piece implant/abutment systems. Int J Oral Maxillofac Implants. 2001; 16:486–494.15. Faulkner MG, Wolfaardt JF, Chan A. Measuring abutment/implant joint integrity with the Periotest instrument. Int J Oral Maxillofac Implants. 1999; 14:681–688.16. Aparicio C. The use of the Periotest value as the initial success criteria of an implant: 8-year report. Int J Periodontic Restor Dent. 1997; 17:150–161.17. Aparicio C, Lang NP, Rangert B. Validity and clinical significance of biomechanical testing of implant/bone interface. Clin Oral Implants Res. 2006; 17:2–7.
Article18. Teerlinck J, Quirynen M, Darius P, van Steenberghe D. Periotest: an objective clinical diagnosis of bone apposition toward implants. Int J Oral Maxillofac Implants. 1991; 6:55–61.19. Devlin H, Horner K, Ledgerton D. A comparison of maxillary and mandibular bone mineral densities. J Prosthet Dent. 1998; 79:323–327.
Article20. Choi HH, Chung CH, Kim SG, Son MK. Reliability of 2 implant stability measuring methods in assessment of various periimplant bone loss: an in vitro study with the Periotest and Osstell Mentor. Implant Dent. 2014; 23:51–56.
Article21. Olivé J, Aparicio C. Periotest method as a measure of osseointegrated oral implant stability. Int J Oral Maxillofac Implants. 1990; 5:390–400.22. Kim SJ, Han DH. Periotest assessment of dental implant mobility: a clinical study. J Korean Acad Prosthodont. 1998; 36:758–771.23. Herrmann I, Lekholm U, Holm S, Kultje C. Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failures. Int J Oral Maxillofac Implants. 2005; 20:220–230.24. Jaffin RA, Berman CL. The excessive loss of Brånemark fixtures in type IV bone: a 5-year analysis. J Periodontol. 1991; 62:2–4.
Article25. Friberg B, Ekestubbe A, Sennerby L. Clinical outcome of Brånemark System implants of various diameters: a retrospective study. Int J Oral Maxillofac Implants. 2002; 17:671–677.26. Jun SH, Chang BM, Weber HP, Kwon JJ. Comparison of initial stability parameters and histomorphometric analysis of implants inserted into extraction sockets: human fresh cadaver study. Int J Oral Maxillofac Implants. 2010; 25:985–990.27. Levin BP. The correlation between immediate implant insertion torque and implant stability quotient. Int J Periodontics Restorative Dent. 2016; 36:833–840.
Article28. Gomez-Roman G, Lukas D. Influence of the implant abutment on the Periotest value: an in vivo study. Quintessence Int. 2001; 32:797–799.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The reliability of Anycheck device related to healing abutment diameter
- Effects of grooved abutment on stability of implant abutment screw
- IN VITRO COMPARATIVE STUDY BETWEEN ISQ AND PERIOTEST? VALUES ON THE IMPLANT STABILITY MEASUREMENTS ACCORDING TO THE INCREASED EFFECTIVE IMPLANT LENGTH
- Non-submerged type implant stability analysis during initial healing period by resonance frequency analysis
- Comparison of initial implant stability measured by Resonance Frequency Analysis between different implant systems