J Cerebrovasc Endovasc Neurosurg.
2018 Jun;20(2):96-105. 10.7461/jcen.2018.20.2.96.
Optimal Surgical Timing of Aspiration for Spontaneous Supratentorial Intracerebral Hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Soonchunhyang University Seoul Hospital, Seoul, Korea. c99867@schmc.ac.kr
- KMID: 2422603
- DOI: http://doi.org/10.7461/jcen.2018.20.2.96
Abstract
OBJECTIVE
Minimally invasive techniques such as stereotactic aspiration have been regarded as promising alternative methods to replace craniotomy in the treatment of intracerebral hemorrhage (ICH). The aim of this study was to identify the optimal timing of stereotactic aspiration and analyze the factors affecting the clinical outcome.
MATERIALS AND METHODS
This retrospective study included 81 patients who underwent stereotactic aspiration for spontaneous supratentorial ICH at single institution. Volume of hematoma was calculated based on computed tomography scan at admission, just before aspiration, immediately after aspiration, and after continuous drainage. The neurologic outcome was compared with Glasgow outcome scale (GOS) score.
RESULTS
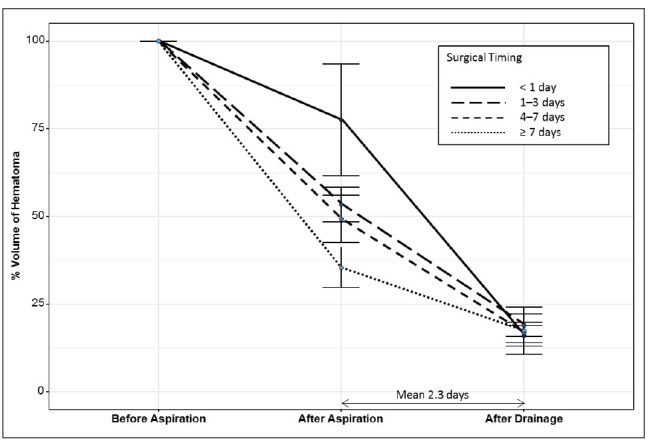
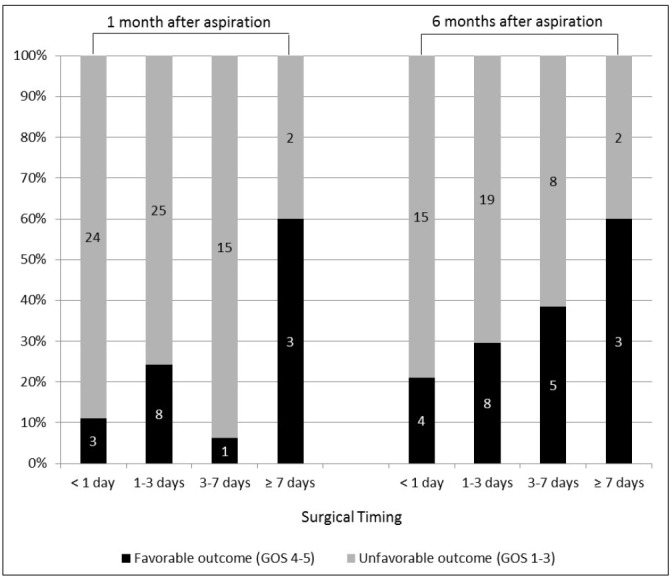
The mean volume ratio of residual hematoma was 59.5% and 17.6% immediately after aspiration and after continuous drainage for an average of 2.3 days, respectively. Delayed aspiration group showed significantly lower residual volume ratio immediately after aspiration. However, there was no significant difference in the residual volume ratio after continuous drainage. The favorable outcome of 1-month GOS 4 or 5 was significantly better in the group with delayed aspiration after more than 7 days (p = 0.029), despite no significant difference in postoperative 6-months GOS score. A factor which has significant correlation with postoperative 6-months favorable outcome was the final hematoma volume ratio after drainage (p = 0.028).
CONCLUSION
There is no difference in final residual volume of hematoma or 6-months neurologic outcome according to the surgical timing of hematoma aspiration. The only factor affecting the postoperative 6-months
MeSH Terms
Figure
Cited by 1 articles
-
Surgical strategy for patients with supratentorial spontaneous intracerebral hemorrhage: minimally invasive surgery and conventional surgery
Je Hun Jang, Won-Sang Cho, Noah Hong, Chang Hwan Pang, Sung Ho Lee, Hyun-Seung Kang, Jeong Eun Kim
J Cerebrovasc Endovasc Neurosurg. 2020;22(3):156-164. doi: 10.7461/jcen.2020.22.3.156.
Reference
-
1. Auer LM, Deinsberger W, Niederkorn K, Gell G, Kleinert R, Schneider G, et al. Endoscopic surgery versus medical treatment for spontaneous intracerebral hematoma: a randomized study. J Neurosurg. 1989; 4. 70(4):530–535. PMID: 2926492.
Article2. Beneš V, Vladyka V, Zvěřina E. Stereotaxic evacuation of typical brain haemorrhage. Acta Neurochir (Wien). 1965; 13(3):419–426. PMID: 5327121.
Article3. Bernays RL, Kollias SS, Romanowski B, Valavanis A, Yonekawa Y. Near-real-time guidance using intraoperative magnetic resonance imaging for radical evacuation of hypertensive hematomas in the basal ganglia. Neurosurgery. 2000; 11. 47(5):1081–1089. discussion 1089-90. PMID: 11063100.
Article4. Carhuapoma JR, Barrett RJ, Keyl PM, Hanley DF, Johnson RR. Stereotactic aspiration-thrombolysis of intracerebral hemorrhage and its impact on perihematoma brain edema. Neurocrit Care. 2008; 8(3):322–329. PMID: 18327659.
Article5. Fayad PB, Awad IA. Surgery for intracerebral hemorrhage. Neurology. 1998; 51(3 Suppl 3):S69–S73. PMID: 9744840.
Article6. Gaab MR. Intracerebral hemorrhage (ICH) and intraventricular hemorrhage (IVH): improvement of bad prognosis by minimally invasive neurosurgery. World Neurosurg. 2011; 2. 75(2):206–208. PMID: 21492714.
Article7. Hazell AS. Excitotoxic mechanisms in stroke: an update of concepts and treatment strategies. Neurochem Int. 2007; 6. 50(7-8):941–953. PMID: 17576023.
Article8. Hondo H, Uno M, Sasaki K, Ebisudani D, Shichijo F, Tóth Z, et al. Computed tomography controlled aspiration surgery for hypertensive intracerebral hemorrhage. Experience of more than 400 cases. Stereotact Funct Neurosurg. 1990; 54-55:432–437. PMID: 2080361.9. Hsieh CT, Chen CY, Chiang YH, Chang CH, Chang CF. Role of diffusion tensor imaging in a patient with spontaneous intracerebral hematoma treated by stereotactic evacuation. Surg Neurol. 2008; 7. 70(1):75–78. PMID: 17707485.
Article10. Huttner HB, Steiner T, Hartmann M, Köhrmann M, Juettler E, Mueller S, et al. Comparison of ABC/2 estimation technique to computer-assisted planimetric analysis in warfarin-related intracerebral parenchymal hemorrhage. Stroke. 2006; 2. 37(2):404–408. PMID: 16373654.
Article11. Jaffe J, AlKhawam L, Du H, Tobin K, O'leary J, Pollock G, et al. Outcome predictors and spectrum of treatment eligibility with prospective protocolized management of intracerebral hemorrhage. Neurosurgery. 2009; 3. 64(3):436–445. PMID: 19240605.
Article12. Keep R, Xiang J, Ennis S, Andjelkovic A, Hua Y, Xi G, et al. Blood-brain barrier function in intracerebral hemorrhage. Cerebral Hemorrhage. Vienna: Springer;2008. p. 73–77.13. Kothari RU, Brott T, Broderick JP, Barsan WG, Sauerbeck LR, Zuccarello M, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996; 8. 27(8):1304–1305. PMID: 8711791.
Article14. Lee JI, Nam DH, Kim JS, Hong SC, Shin HJ, Park K, et al. Stereotactic aspiration of intracerebral haematoma: significance of surgical timing and haematoma volume reduction. J Clin Neurosci. 2003; 7. 10(4):439–443. PMID: 12852882.
Article15. Lippitz BE, Mayfrank L, Spetzger U, Warnke JP, Bertalanffy H, Gilsbach JM. Lysis of basal ganglia haematoma with recombinant tissue plasminogen activator (rtPA) after stereotactic aspiration: initial results. Acta Neurochir (Wien). 1994; 127(3-4):157–160. PMID: 7942196.
Article16. Marquardt G, Wolff R, Sager A, Janzen RW, Seifert V. Subacute stereotactic aspiration of haematomas within the basal ganglia reduces occurrence of complications in the course of haemorrhagic stroke in non-comatose patients. Cerebrovasc Dis. 2003; 15(4):252–257. PMID: 12686788.
Article17. Marquardt G, Wolff R, Sager A, Hartung A, Lorenz R. Manual stereotactic aspiration of spontaneous deep-seated intracerebral haematomas in non-comatose patients. Br J Neurosurg. 2001; 4. 15(2):126–131. PMID: 11360375.18. Matsumoto K, Hondo H. CT-guided stereotaxic evacuation of hypertensive intracerebral hematomas. J Neurosurg. 1984; 9. 61(3):440–448. PMID: 6379125.
Article19. Mendelow AD, Gregson BA, Fernandes HM, Murray GD, Teasdale GM, Hope DT, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial intracerebral haematomas in the International Surgical Trial in Intracerebral Haemorrhage (STICH): a randomised trial. Lancet. 2005; 1. 29. 2. 04. 365(9457):387–397. PMID: 15680453.
Article20. Mendelow AD, Gregson BA, Rowan EN, Murray GD, Gholkar A, Mitchell PM, et al. Early surgery versus initial conservative treatment in patients with spontaneous supratentorial lobar intracerebral haematomas (STICH II): a randomised trial. Lancet. 2013; 8. 382(9890):397–408. PMID: 23726393.
Article21. Montes JM, Wong JH, Fayad PB, Awad IA. Stereotactic computed tomographic–guided aspiration and thrombolysis of intracerebral hematoma : protocol and preliminary experience. Stroke. 2000; 4. 31(4):834–840. PMID: 10753984.22. Morgenstern LB, Demchuk AM, Kim DH, Frankowski RF, Grotta JC. Rebleeding leads to poor outcome in ultra-early craniotomy for intracerebral hemorrhage. Neurology. 2001; 5. 56(10):1294–1299. PMID: 11376176.
Article23. Niizuma H, Otsuki T, Johkura H, Nakazato N, Suzuki J. CT-guided stereotactic aspiration of intracerebral hematoma– result of a hematoma-lysis method using urokinase. Appl Neurophysiol. 1985; 48(1-6):427–430. PMID: 3915660.24. Niizuma H, Shimizu Y, Yonemitsu T, Nakasato N, Suzuki J. Results of stereotactic aspiration in 175 cases of putaminal hemorrhage. Neurosurgery. 1989; 6. 24(6):814–819. PMID: 2664544.
Article25. Prasad K, Mendelow AD, Gregson B. Surgery for primary supratentorial intracerebral haemorrhage. Cochrane Database Syst Rev. 2008; 10. 08. (4):CD000200. PMID: 18843607.
Article26. Ramanan M, Shankar A. Minimally invasive surgery for primary supratentorial intracerebral haemorrhage. J Clin Neurosci. 2013; 12. 20(12):1650–1658. PMID: 24161339.
Article27. Schaller C, Rohde V, Meyer B, Hassler W. Stereotactic puncture and lysis of spontaneous intracerebral hemorrhage using recombinant tissue-plasminogen activator. Neurosurgery. 1995; 2. 36(2):328–333. discussion 333-5. PMID: 7731513.
Article28. Siddique SM, Mendelow AD. Surgical treatment of intracerebral haemorrhage. Br Med Bull. 2000; 1. 56(2):444–456. PMID: 11092093.
Article29. Staykov D, Huttner HB, Köhrmann M, Bardutzky J, Schellinger PD. Novel approaches to the treatment of intracerebral haemorrhage. Int J Stroke. 2010; 12. 5(6):457–465. PMID: 21050402.
Article30. Umebayashi D, Mandai A, Osaka Y, Nakahara Y, Tenjin H. Effects and complications of stereotactic aspiration for spontaneous intracerebral hemorrhage. Neurol Med Chir (Tokyo). 2010; 50(7):538–544. PMID: 20671378.
Article31. Wang JW, Li JP, Song YL, Tan K, Wang Y, Li T, et al. Stereotactic aspiration versus craniotomy for primary intracerebral hemorrhage: a meta-analysis of randomized controlled trials. PLoS One. 2014; 9. 9(9):e107614. PMID: 25237813.
Article32. Wu G, Sheng F, Wang L, Wang F, et al. The pathophysiological time window study of performing minimally invasive procedures for the intracerebral hematoma evacuation in rabbit. Brain Res. 2012; 7. 17. 1465:57–65. PMID: 22658751.
Article33. Yoshioka H, Horikoshi T, Aoki S, Hori M, Ishigame K, Uchida M, et al. Diffusion tensor tractography predicts motor functional outcome in patients with spontaneous intracerebral hemorrhage. Neurosurgery. 2008; 1. 62(1):97–103. discussion 103. PMID: 18300896.
Article34. Zuccarello M, Brott T, Derex L, Kothari R, Sauerbeck L, Tew J, et al. Early surgical treatment for supratentorial intracerebral hemorrhage: a randomized feasibility study. Stroke. 1999; 9. 30(9):1833–1839. PMID: 10471432.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Percutaneous Needle Aspiration for Evacuation of Intracerebral Hemorrhage: A Volumetric and Clincal Outcone Study
- Clinical Analysis for Stereotatic Aspiration and Thrombolysis of Spontaneous Intracerebral Hemorrhage
- The Management of Spontaneous Intracerebral Hemorrhage: Medical Versus Surgical Therapy for Spontaneous Intracerebral Hemorrhage
- Clinical Analysis of Stereotactic aspiration in the Management of Spontaneous Intracerebral Hemorrhage
- Brain Abscess Associated with Primary Intracerebral Hemorrhage: Case Report