Yonsei Med J.
2018 Nov;59(9):1107-1114. 10.3349/ymj.2018.59.9.1107.
Preliminary Findings on the Effectiveness of Meaning-Centered Psychotherapy in Patients with Pancreatobiliary Cancer
- Affiliations
-
- 1Department of Psychiatry , Yonsei University College of Medicine, Seoul, Korea. johnstein@yuhs.ac
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea.
- 3Department of Psychiatry, Yeungnam University College of Medicine, Daegu, Korea.
- 4Department of Surgery, Konyang University College of Medicine, Daejeon, Korea.
- 5Department of Psychiatry, Konyang University College of Medicine, Daejeon, Korea.
- 6Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. yds6110@yuhs.ac
- KMID: 2422496
- DOI: http://doi.org/10.3349/ymj.2018.59.9.1107
Abstract
- PURPOSE
This study investigated the effectiveness of meaning-centered psychotherapy (MCP), which is known to be a helpful psychotherapeutic intervention in distressing conditions, for patients with pancreatobiliary cancer.
MATERIALS AND METHODS
We recruited 37 patients with pancreatobiliary cancer from three university general hospitals and assessed their psychological characteristics. Patients who reported clinically significant emotional distress were recommended to undergo MCP. Patients who consented to MCP were provided four sessions of the therapy. Patient psychological characteristics were assessed again 2 months after MCP. For statistical comparison, outcome variables included anxiety, depression, mental adjustment to cancer, and quality of life (QoL), as well as the degree of stress and physical symptoms.
RESULTS
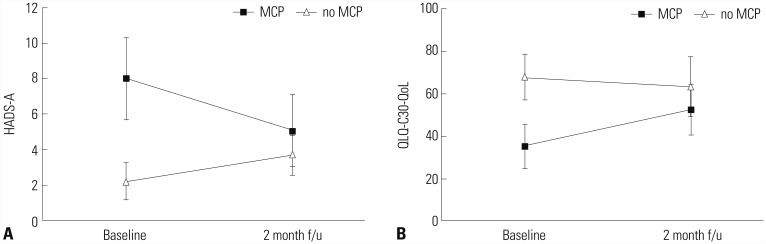
Sixteen patients completed the MCP and the final assessment 2 months later. In the initial assessment, the patients receiving MCP showed higher levels of anxiety and depression than those not receiving MCP, and QoL was also lower in terms of role function, emotional function, social function, and global QoL. At the 2-month follow-up, the MCP group showed a significant improvement in anxiety (p=0.007), depression (p=0.010), and anxious preoccupation (p < 0.001). In addition, QoL significantly improved in the MCP group, while there was no significant change in the non-MCP group.
CONCLUSION
In this study, MCP showed potential therapeutic benefits against emotional distress in patients with pancreatobiliary cancer, improving their QoL.
Figure
Reference
-
1. Statistics Korea. Death rates (2016) in Korea. Accessed 2017 December 3. Available at: http://kostat.go.kr/portal/korea/kor_nw/2/6/2/index.board?bmode=read&bSeq=&aSeq=363268&pageNo=1&rowNum=10&navCount=10&currPg=&sTarget=title&sTxt=.2. Korea Central Cancer Registry. Annual report of cancer statistics in Korea in 2014. Accessed 2017 December 3. Available at: http://ncc.re.kr/cancerStatsView.ncc?bbsnum=417&searchKey=total&searchValue=&pageNum=1.3. Jia L, Jiang SM, Shang YY, Huang YX, Li YJ, Xie DR, et al. Investigation of the incidence of pancreatic cancer-related depression and its relationship with the quality of life of patients. Digestion. 2010; 82:4–9. PMID: 20145402.
Article4. Tavoli A, Mohagheghi MA, Montazeri A, Roshan R, Tavoli Z, Omidvari S. Anxiety and depression in patients with gastrointestinal cancer: does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007; 7:28. PMID: 17629928.
Article5. Song SY. Recent trends in pancreatic cancer chemotherapy. Korean J Pancreas Biliary Tract. 2004; 9:92–101.6. Sinclair S, Pereira J, Raffin S. A thematic review of the spirituality literature within palliative care. J Palliat Med. 2006; 9:464–479. PMID: 16629575.
Article7. Chochinov HM, Cann BJ. Interventions to enhance the spiritual aspects of dying. J Palliat Med. 2005; 8(Suppl 1):S103–S115. PMID: 16499458.
Article8. Kelly B, Burnett P, Pelusi D, Badger S, Varghese F, Robertson M. Factors associated with the wish to hasten death: a study of patients with terminal illness. Psychol Med. 2003; 33:75–81. PMID: 12537038.
Article9. Ransom S, Sacco WP, Weitzner MA, Azzarello LM, McMillan SC. Interpersonal factors predict increased desire for hastened death in late-stage cancer patients. Ann Behav Med. 2006; 31:63–69. PMID: 16472040.
Article10. Breitbart W. Reframing hope: meaning-centered care for patients near the end of life. Interview by Karen S. Heller. J Palliat Med. 2003; 6:979–988. PMID: 14733692.11. Frankl VE. Man's search for meaning. New York (NY): Simon & Schuster, Inc.;1985.12. Breitbart W, Poppito S, Rosenfeld B, Vickers AJ, Li Y, Abbey J, et al. Pilot randomized controlled trial of individual meaning-centered psychotherapy for patients with advanced cancer. J Clin Oncol. 2012; 30:1304–1309. PMID: 22370330.
Article13. Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Nelson C, et al. Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psychooncology. 2010; 19:21–28. PMID: 19274623.
Article14. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67:361–370. PMID: 6880820.
Article15. Greer S, Watson M. Mental adjustment to cancer: its measurement and prognostic importance. Cancer Surv. 1987; 6:439–453. PMID: 3326657.16. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. 1993; 85:365–376. PMID: 8433390.
Article17. Fitzsimmons D, Johnson CD, George S, Payne S, Sandberg AA, Bassi C, et al. Development of a disease specific quality of life (QoL) questionnaire module to supplement the EORTC core cancer QoL questionnaire, the QLQ-C30 in patients with pancreatic cancer. EORTC Study Group on Quality of Life. Eur J Cancer. 1999; 35:939–941. PMID: 10533475.18. Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967; 11:213–218. PMID: 6059863.
Article19. National Comprehensive Cancer Network. Distress management. Clinical practice guidelines. J Natl Compr Canc Netw. 2003; 1:344–374. PMID: 19761069.20. Fayers PM, Aaronson NK, Bjordal K, Groenvold M, Curran D, Bottomley A. the EORTC Quality of Life Group. The EORTC QLQ-C30 Scoring Manual. 3rd ed. Brussels: European Organisation for Research and Treatment of Cancer;European Organisation for Research and Treatment of Cancer.21. Kim SY, Kim JM, Kim SW, Shin IS, Yoon JS, Shim HJ. Management of depression in terminally ill cancer patients. Korean J Psychopharmacol. 2010; 21:51–61.22. Frankl VE. Man's search for ultimate meaning. Cambridge (MA): Perseus Publishing;2000.23. Frankl VE. The will to meaning: foundations and applications of logotherapy. New York: Penguin Books;1988.24. Kang JI, Chung HC, Kim SJ, Choi HJ, Ahn JB, Jeung HC, et al. Standardization of the Korean version of Mini-Mental Adjustment to Cancer (K-Mini-MAC) scale: factor structure, reliability and validity. Psychooncology. 2008; 17:592–597. PMID: 17957732.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics and Effectiveness of Individual Psychotherapy for Palliative and End-of-Life Care: A Literature Review for Randomized Controlled Trials
- Effects of Meaning-Centered Therapy on Depressive Symptoms in Adults and Older Adults: A Systematic Review
- Can the Effectiveness of the Psychoanalytic Therapies Truly Be Proven?: The Effectiveness of the Psychoanalysis and Psychoanalytic Psychotherapy
- Systematic Review of Meaning-centered Interventions for Adolescents
- Communication at the End of Life