Ann Surg Treat Res.
2018 Oct;95(4):213-221. 10.4174/astr.2018.95.4.213.
Intraoperative abortion of adult living donor liver transplantation: 15 cases from 1,179 cases in 20 years of experience in a single center
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. gskim@skku.edu
- 2Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2421199
- DOI: http://doi.org/10.4174/astr.2018.95.4.213
Abstract
- PURPOSE
This study aimed to report intraoperative abortion of adult living donor liver transplantation (LDLT).
METHODS
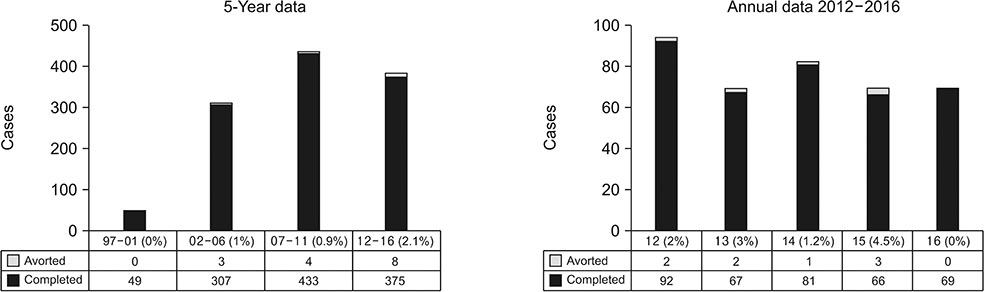
From June 1997 to December 2016, 1,179 adult LDLT cases were performed. 15 cases (1.3%) of intraoperative abortions in LDLT were described.
RESULTS
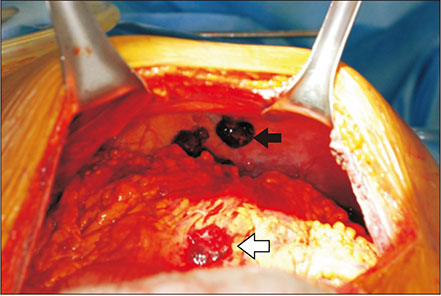
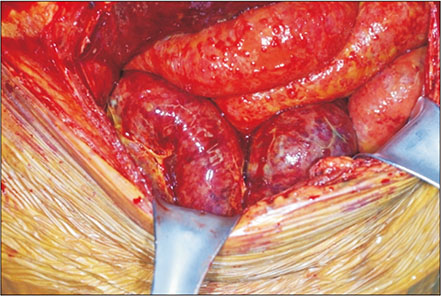
Among 15 cases, 5 intraoperative abortions were donor-related, and remaining 10 cases were recipient-related. All donor-related abortions were due to unexpected steatohepatitis. Among remaining 10 recipient-related intraoperative abortions, unexpected extension of hepatocellular carcinoma was related in 5 cases. Two cases of intraoperative abortions were related to bowel inflammation, and 2 cases were associated with severe adhesion related to previous treatment. One recipient with severe pulmonary hypertension was also aborted.
CONCLUSION
Complete prevention of aborted LDLT is still not feasible. In this regard, further efforts to minimize intraoperative abortion are required.
MeSH Terms
Figure
Reference
-
1. Kawasaki S, Makuuchi M, Matsunami H, Hashikura Y, Ikegami T, Nakazawa Y, et al. Living related liver transplantation in adults. Ann Surg. 1998; 227:269–274.
Article2. Shah SA, Levy GA, Greig PD, Smith R, McGilvray ID, Lilly LB, et al. Reduced mortality with right-lobe living donor compared to deceased-donor liver transplantation when analyzed from the time of listing. Am J Transplant. 2007; 7:998–1002.
Article3. Guba M, Adcock L, MacLeod C, Cattral M, Greig P, Levy G, et al. Intraoperative ‘no go’ donor hepatectomies in living donor liver transplantation. Am J Transplant. 2010; 10:612–618.
Article4. Kwon CH, Kim DJ, Han YS, Park JB, Choi GS, Kim SJ, et al. HCC in living donor liver transplantation: can we expand the Milan criteria. Dig Dis. 2007; 25:313–319.
Article5. Shin M, Song S, Kim JM, Kwon CH, Kim SJ, Lee SK, et al. Donor morbidity including biliary complications in living-donor liver transplantation: single-center analysis of 827 cases. Transplantation. 2012; 93:942–948.6. Taourel P, Bret PM, Reinhold C, Barkun AN, Atri M. Anatomic variants of the biliary tree: diagnosis with MR cholangiopancreatography. Radiology. 1996; 199:521–527.
Article7. Nakamura T, Tanaka K, Kiuchi T, Kasahara M, Oike F, Ueda M, et al. Anatomical variations and surgical strategies in right lobe living donor liver transplantation: lessons from 120 cases. Transplantation. 2002; 73:1896–1903.8. Basaran C, Agildere AM, Donmez FY, Sevmis S, Budakoglu I, Karakayali H, et al. MR cholangiopancreatography with T2-weighted prospective acquisition correction turbo spin-echo sequence of the biliary anatomy of potential living liver transplant donors. AJR Am J Roentgenol. 2008; 190:1527–1533.
Article9. Song GW, Lee SG, Hwang S, Sung GB, Park KM, Kim KH, et al. Preoperative evaluation of biliary anatomy of donor in living donor liver transplantation by conventional nonenhanced magnetic resonance cholangiography. Transpl Int. 2007; 20:167–173.
Article10. McCormack L, Petrowsky H, Jochum W, Mullhaupt B, Weber M, Clavien PA. Use of severely steatotic grafts in liver transplantation: a matched case-control study. Ann Surg. 2007; 246:940–946.11. Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant. 2005; 5:2605–2610.
Article12. Sasso M, Miette V, Sandrin L, Beaugrand M. The controlled attenuation parameter (CAP): a novel tool for the non-invasive evaluation of steatosis using Fibroscan. Clin Res Hepatol Gastroenterol. 2012; 36:13–20.
Article13. Gondolesi GE, Roayaie S, Muñoz L, Kim-Schluger L, Schiano T, Fishbein TM, et al. Adult living donor liver transplantation for patients with hepatocellular carcinoma: extending UNOS priority criteria. Ann Surg. 2004; 239:142–149.14. Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001; 33:1394–1403.
Article15. Soejima Y, Taketomi A, Yoshizumi T, Uchiyama H, Aishima S, Terashi T, et al. Extended indication for living donor liver transplantation in patients with hepatocellular carcinoma. Transplantation. 2007; 83:893–899.
Article16. Kaihara S, Kiuchi T, Ueda M, Oike F, Fujimoto Y, Ogawa K, et al. Living-donor liver transplantation for hepatocellular carcinoma. Transplantation. 2003; 75:3 Suppl. S37–S40.
Article17. Jonas S, Bechstein WO, Steinmüller T, Herrmann M, Radke C, Berg T, et al. Vascular invasion and histopathologic grading determine outcome after liver transplantation for hepatocellular carcinoma in cirrhosis. Hepatology. 2001; 33:1080–1086.
Article18. Ravaioli M, Ercolani G, Cescon M, Vetrone G, Voci C, Grigioni WF, et al. Liver transplantation for hepatocellular carcinoma: further considerations on selection criteria. Liver Transpl. 2004; 10:1195–1202.
Article19. Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996; 334:693–699.
Article20. Cillo U, Vitale A, Bassanello M, Boccagni P, Brolese A, Zanus G, et al. Liver transplantation for the treatment of moderately or well-differentiated hepatocellular carcinoma. Ann Surg. 2004; 239:150–159.
Article21. Kim AY, Sinn DH, Jeong WK, Kim YK, Kang TW, Ha SY, et al. Hepatobiliary MRI as novel selection criteria in liver transplantation for hepatocellular carcinoma. J Hepatol. 2018; 68:1144–1152.
Article22. Ramsay MA, Simpson BR, Nguyen AT, Ramsay KJ, East C, Klintmalm GB. Severe pulmonary hypertension in liver transplant candidates. Liver Transpl Surg. 1997; 3:494–500.
Article23. Colle IO, Moreau R, Godinho E, Belghiti J, Ettori F, Cohen-Solal A, et al. Diagnosis of portopulmonary hypertension in candidates for liver transplantation: a prospective study. Hepatology. 2003; 37:401–409.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Split liver transplantation for two adult recipients: A collective review of Korean experience
- Liver retransplantation for adult recipients
- Complete transition from open to laparoscopic living donor hepatectomy: 8-year experience with more than 500 laparoscopy cases
- Split liver transplantation for one adult and one pediatric recipient: A collective review of Korean experience