Korean J Women Health Nurs.
2018 Sep;24(3):310-321. 10.4069/kjwhn.2018.24.3.310.
Effects of Menstrual Self-management Education Program on Knowledge and Behavior of Menstrual Self-management in High School Girls
- Affiliations
-
- 1Health Teacher, Gowoon High School, Sejong, Korea.
- 2Professor, College of Nursing, Chungnam National University, Daejeon, Korea. sukheeahn@cnu.ac.kr
- KMID: 2420852
- DOI: http://doi.org/10.4069/kjwhn.2018.24.3.310
Abstract
- PURPOSE
To examine the effect of menstrual self-management education program on knowledge and behavior of menstrual self-management in high school girls.
METHODS
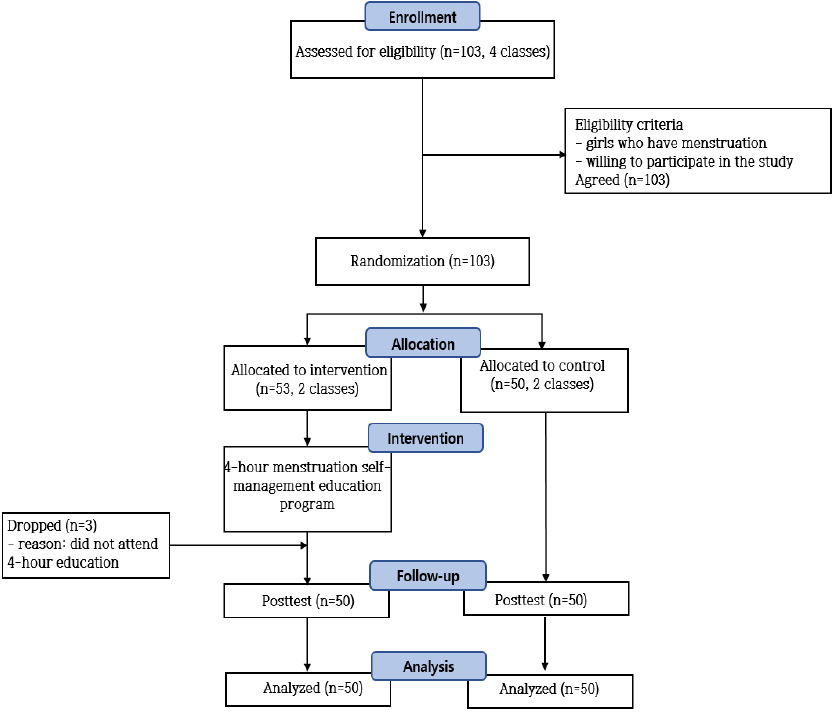
With a randomized controlled trial, 100 high school girl students were randomly assigned into experimental group and control group. Menstruation self-management program was consisted of a total of four sessions of education program (1 hour of education per session). Control group only received the first class of education. Measurement tools were 20-item menstrual knowledge scale and 12-item women's genito-urinary hygiene scale. Pretest and post-test questionnaires were administered.
RESULTS
There were significant differences in menstrual knowledge as well as menstrual self-management behavior between the two groups. The experimental group showed significant improvement in both menstrual knowledge score (t=13.37, p < .001) and menstrual self-management behavior score (t=8.38, p < .001) than the control group.
CONCLUSION
Results of this study suggest that the monthly self-management education program is effective in increasing the knowledge of menstruation of female high school students and enhancing their performance. This program needs to be implemented as a part of high school's standard sex education. Further study is needed to analyze follow-up effects of the program on self-management behavior of students after at least one menstrual cycle.
MeSH Terms
Figure
Reference
-
1. Min S, Ki J, Kim J, Kim H, Kim H, Park S, et al. Sex education for teenagers with parents and teachers. Seoul: Korean Sexology Research Association;2016. p. 344.2. Jogdand K, Yerpude P. A community based study on menstrual hygiene among adolescent girls. Indian J Matern Child Health. 2011; 13(3):1–6.3. Adinma ED, Adinma JI. Perceptions and practices on menstruation amongst Nigerian secondary school girls. Afr J Reprod Health. 2008; 12(1):74–83.4. Berhe H, Bayray A, Ukbayohannes R, Getachew G. Menstrual hygiene practice and associated factors among adolescent high school girls. J Bio-Innov. 2016; 5(1):1–15.5. Santina T, Wehbe N, Ziade F, Nehme M. Assessment of beliefs and practices relating to menstrual hygiene of adolescent girls in Lebanon. Int J Health Sci Res. 2013; 3(12):75–88.6. Kapoor G, Kumar D. Menstrual hygiene: Knowledge and practice among adolescent school girls in rural settings. Int J Reprod Contracept Obstet Gynecol. 2017; 6(3):959–962. DOI: 10.18203/2320-1770.ijrcog20170564.
Article7. Ahn S, Cho K. Personal hygiene practices related to genitourinary tract and menstrual hygiene management in female adolescents. Korean J Women Health Nurs. 2014; 20(3):215–224. DOI: 10.4069/kjwhn.2014.20.3.215.
Article8. Anand E, Singh J, Unisa S. Menstrual hygiene practices and its association with reproductive tract infections and abnormal vaginal discharge among women in India. Sex Reprod Healthc. 2015; 6(4):249–254. DOI: 10.1016/j.srhc.2015.06.001.
Article9. Kansal S, Singh S, Kumar A. Menstrual hygiene practices in context of schooling: A community study among rural adolescent girls in Varanasi. Indian J Community Med. 2016; 41(1):39–44. DOI: 10.4103/0970-0218.170964.
Article10. Low N, Chersich MF, Schmidlin K, Egger M, Francis SC, van de, et al. Intravaginal practices, bacterial vaginosis, and HIV infection in women: individual participant data metaanalysis. PLoS Med. 2011; 8(2):e1000416. DOI: 10.1371/journal.pmed.1000416.
Article11. Bui TC, Thai TN, Tran LT, Shete SS, Ramondetta LM, Basen-Engquist KM. Association between vaginal douching and genital human papillomavirus infection among women in the United States. J Infect Dis. 2016; 214(9):1370–1375. DOI: 10.1093/infdis/jiw388.
Article12. Na J, Kim Y, Kim H. The effects of systematic health education on health knowledge and health promotion behavior in elementary school students. J Korean Soc Sch Health. 2011; 24(2):173–180.13. The Education Ministry. School sex education standard for teachers' guide (elementary, middle, and high school). Sejong: Author;2015. p. 1096.14. Choo Y, Ko H, Kwon H, Kim B, Kim J, Noh Y, et al. Science of sex. 4th ed. Seoul: World Science;2015. p. 361.15. Kim J. Comparison and analysis on national health education standards for high school in South Korea. J Korean Soc Sch Health. 2016; 2(1):25–40.16. El-Mowafy RI, Mohamed Moussa MM, El-Ezaby HH. Effect of health education program on knowledge and practices about menstrual hygiene among adolescents girls at orphanage home. IOSR J Nurs Health Sci. 2014; 3(6):48–55.
Article17. Haque SE, Rahman M, Itsuko K, Mutahara M, Sakisaka K. The effect of a school-based educational intervention on menstrual health: An intervention study among adolescent girls in Bangladesh. BMJ Open. 2014; 4(7):e004607. DOI: 10.1136/bmjopen-2013-004607.
Article18. Nemade D, Seema A, Gujar R. Impact of health education on knowledge and practices about menstruation among adolescent school girls of Kalamboli, Navi-Mumbai. Health Popul: Perspect Popul. 2009; 32(4):167–175.19. Su JJ, Lindell D. Promoting the menstrual health of adolescent girls in China. Nurs Health Sci. 2016; 18:481–487.
Article20. Jun J. Effects of experience based menstrual education program on menstrual attitude and menstrual discomfort among female elementary students [master's thesis]. Busan: Pusan National University;2007. 75.21. Oh S. The comparison of sex-related knowledge and attitude of 6th-grade elementary school students between the field based learning and the cooperative learning method [master's thesis]. Daejeon: Chungnam National University;2010. 59.22. Lee Y. Development and effects of nocturnal emission and menstruation education program using CAI for Korean elementary school children [dissertation]. Seoul: Ewha Womans University;2010. 130.23. Kim J. Effect of heated red bean pillow application for college women with dysmenorrhea. Korean J Women Health Nurs. 2013; 19(2):67–74. DOI: 10.4069/kjwhn.2013.19.2.67.
Article24. Potur DC, Komurcu N. The effects of local how-dose heat application on dysmenorrhea. J Pediatr Adolesc Gynecol. 2014; 27(4):216–221. DOI: 10.1016/j.jpag.2013.11.003.25. Park K, Hwang EH, Shin MS, Sul JU. An effect of yoga therapy on relieving dysmenorrhea: RCTs (randomized controlled trials) review. Korean J Orient Prev Med. 2011; 15(2):39–49.26. Czerwinski BS. Variation in feminine hygiene practices as afunction of age. J Obstet Gynecol Neonatal Nurs. 2000; 29(6):625–633.27. Ahn S. Feminine hygiene and vaginal douche practices in middle-aged women. Korean J Women Health Nurs. 2013; 19(4):285–294. DOI: 10.4069/kjwhn.2013.19.4.285.
Article28. Rothman KJ, Funch DP, Alfredson T, Brady J, Dreyer NA. Randomized field trial of vaginal douching, pelvic inflammatory disease and pregnancy. Epidemiology. 2003; 14(3):340–348.
Article29. Kim Y, Park U. The effects of health education on health knowledge and health promoting behaviors in elementary school students. J Korean Soc Sch Health. 2013; 26(2):55–61.30. Kim K. Amos 18.0, analysis structural equation modeling. Seoul: Hannarae Academy;2010. p. 600.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Perfectionism and Testing Anxiety on the Menstrual Cycle during Test Evaluations among High School Girls
- Relationships among Attitudes toward Menstruation, Peri-menstrual Symptoms, and Coping in Adolescent Girls
- Intervention to Improve Menstrual Health Among Adolescent Girls Based on the Theory of Planned Behavior in Iran: A Cluster-randomized Controlled Trial
- Menstrual hygiene management and its determinants among adolescent girls in low-income urban areas of Delhi, India: a community-based study
- Status of Use of Menstrual Hygiene Products and Genital Organ Hygiene Management in Unmarried Women