Ann Lab Med.
2019 Jan;39(1):23-30. 10.3343/alm.2019.39.1.23.
Effectiveness of Platelet Function Analyzer-100 for Laboratory Detection of Anti-Platelet Drug-Induced Platelet Dysfunction
- Affiliations
-
- 1Department of Laboratory Medicine, Aerospace Medical Center, Republic of Korea Air Force, Cheongju, Korea.
- 2Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea. hyekim@cau.ac.kr
- 3Department of Laboratory Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- KMID: 2420267
- DOI: http://doi.org/10.3343/alm.2019.39.1.23
Abstract
- BACKGROUND
High on-treatment platelet reactivity (HTPR) is the phenomenon wherein patients exhibit normal platelet activity in laboratory testing despite adequate adherence to anti-platelet treatment. We investigated the detection rates of Platelet Function Analyzer (PFA)-100 (Dade Behring AG, Düdingen, Switzerland) for drug-induced platelet dysfunction and analyzed potential contributors to HTPR with practical PFA-100 data over six years.
METHODS
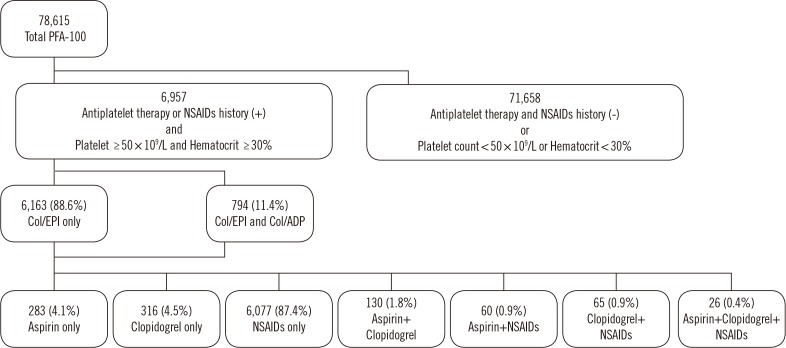
We used data from 6,957 patients who underwent PFA-100 testing after receiving aspirin, clopidogrel, or non-steroidal anti-inflammatory drugs (NSAIDs). Of these, 6,163 patients were tested with only the collagen/epinephrine cartridge (Col/EPI) of PFA-100; 794 were tested with both Col/EPI and the collagen/ADP cartridge (Col/ADP). We calculated PFA-100 closure time (CT) for each drug and compared the clinical and laboratory characteristics of the patients with prolonged CTs and normal CTs (i.e., HTPR).
RESULTS
In Col/EPI, 73.2% (365/499), 72.6% (390/537), and 55.3% (3,442/6,228) patients showed prolonged CTs for aspirin, clopidogrel, and NSAIDs, respectively. In Col/ADP, prolonged CTs were observed in 37.4% (34/91), 43.2% (35/81), and 29.6% (200/676) of patients receiving aspirin, clopidogrel, and NSAIDs, respectively. Of the patients tested with both cartridges, 88.9% (48/54), 95.3% (41/43), and 89.0% (577/648) of the patients receiving aspirin, clopidogrel, and NSAIDs had prolonged CTs, and 10.0% (79/794) showed normal CTs regardless of drugs. For clopidogrel users (both cartridges), there were more patients with malignancies in the normal CT than prolonged CT group.
CONCLUSIONS
PFA-100 is not sufficiently effective for laboratory screening of drug-induced platelet dysfunction. Malignancy may contribute to clopidogrel-related HTPR in PFA-100.
Keyword
MeSH Terms
Figure
Reference
-
1. Mammen EF, Comp PC, Gosselin R, Greenberg C, Hoots WK, Kessler CM, et al. PFA-100 system: a new method for assessment of platelet dysfunction. Semin Thromb Hemost. 1998; 24:195–202. PMID: 9579642.2. Fintel DJ. Oral antiplatelet therapy for atherothrombotic disease: overview of current and emerging treatment options. Vasc Health Risk Manag. 2012; 8:77–89. PMID: 22393298.3. Stegnar M. Platelet function tests and resistance to antiplatelet therapy. Srp Arh Celok Lek. 2010; 138:59–63. PMID: 20229685.4. Lordkipanidzé M, Pharand C, Nguyen TA, Schampaert E, Palisaitis DA, Diodati JG. Comparison of four tests to assess inhibition of platelet function by clopidogrel in stable coronary artery disease patients. Eur Heart J. 2008; 29:2877–2885. PMID: 18826988.5. Cattaneo M. Resistance to antiplatelet drugs: molecular mechanisms and laboratory detection. J Thromb Haemost. 2007; 5:230–237. PMID: 17635731.6. Agarwal S, Coakley M, Reddy K, Riddell A, Mallett S. Quantifying the effect of antiplatelet therapy: a comparison of the Platelet Function Analyzer (PFA-100®) and modified thromboelastography (mTEG®) with light transmission platelet aggregometry. Anesthesiology. 2006; 105:676–683. PMID: 17006064.7. Bartels A, Sarpong Y, Coberly J, Hughes N, Litt J, Quick J, et al. Failure of the platelet function assay (PFA)-100 to detect antiplatelet agents. Surgery. 2015; 158:1012–1018. Discussion 1018-9. PMID: 26299285.8. Baigent C, Patrono C. Selective cyclooxygenase 2 inhibitors, aspirin, and cardiovascular disease: a reappraisal. Arthritis Rheum. 2003; 48:12–20. PMID: 12528099.9. Bozimowski G. A review of nonsteroidal anti-inflammatory drugs. AANA J. 2015; 83:425–433. PMID: 26742337.10. Goldenberg NA, Jacobson L, Manco-Johnson MJ. Brief communication: duration of platelet dysfunction after a 7-day course of ibuprofen. Ann Intern Med. 2005; 142:506–509. PMID: 15809462.11. van Kraaij DJ, Hovestad-Witterland AH, de Metz M, Vollaard EJ. A comparison of the effects of nabumetone vs meloxicam on serum thromboxane B2 and platelet function in healthy volunteers. Br J Clin Pharmacol. 2002; 53:644–647. PMID: 12047490.12. Kearney PM, Baigent C, Godwin J, Halls H, Emberson JR, Patrono C. Do selective cyclo-oxygenase-2 inhibitors and traditional non-steroidal anti-inflammatory drugs increase the risk of atherothrombosis? Meta-analysis of randomised trials. BMJ. 2006; 332:1302–1308. PMID: 16740558.13. Kim JA, Kim JE, Song SH, Kim HK. Influence of blood lipids on global coagulation test results. Ann Lab Med. 2015; 35:15–21. PMID: 25553275.14. Catena C, Zingaro L, Casaccio D, Sechi LA. Abnormalities of coagulation in hypertensive patients with reduced creatinine clearance. Am J Med. 2000; 109:556–561. PMID: 11063957.15. Jakl M, Sevcik R, Fatorova I, Horacek JM, Pudil R. High on-treatment platelet reactivity: risk factors and 5-year outcomes in patients with acute myocardial infarction. Anatol J Cardiol. 2017; 17:113–118. PMID: 27721320.16. Park KW, Park JJ, Jeon KH, Kang SH, Oh IY, Yang HM, et al. Clinical predictors of high posttreatment platelet reactivity to clopidogrel in Koreans. Cardiovasc Ther. 2012; 30:5–11. PMID: 21129165.17. Maree AO, Curtin RJ, Dooley M, Conroy RM, Crean P, Cox D, et al. Platelet response to low-dose enteric-coated aspirin in patients with stable cardiovascular disease. J Am Coll Cardiol. 2005; 46:1258–1263. PMID: 16198840.18. Kundu SK, Heilmann EJ, Sio R, Garcia C, Davidson RM, Ostgaard RA. Description of an in vitro platelet function analyzer--PFA-100. Semin Thromb Hemost. 1995; 21(Suppl 2):106–112.19. Harrison P, Robinson MS, Mackie IJ, Joseph J, McDonald SJ, Liesner R, et al. Performance of the platelet function analyser PFA-100 in testing abnormalities of primary haemostasis. Blood Coagul Fibrinolysis. 1999; 10:25–31. PMID: 10070832.20. Warner TD, Nylander S, Whatling C. Anti-platelet therapy: cyclo-oxygenase inhibition and the use of aspirin with particular regard to dual anti-platelet therapy. Br J Clin Pharmacol. 2011; 72:619–633. PMID: 21320154.21. Cho YU, Chi HS, Jang S, Park CJ. Reconfirmation of preanalytical variables and establishment of reference intervals of platelet function analyzer-100 closure times in Korean adults. Korean J Lab Med. 2007; 27:318–323. PMID: 18094595.22. Paniccia R, Antonucci E, Gori AM, Marcucci R, Giglioli C, Antoniucci D, et al. Different methodologies for evaluating the effect of clopidogrel on platelet function in high-risk coronary artery disease patients. J Thromb Haemost. 2007; 5:1839–1847. PMID: 17723123.23. Patrono C, Rocca B. Drug insight: aspirin resistance--fact or fashion? Nat Clin Pract Cardiovasc Med. 2007; 4:42–50. PMID: 17180149.24. Harrison P, Segal H, Blasbery K, Furtado C, Silver L, Rothwell PM. Screening for aspirin responsiveness after transient ischemic attack and stroke: comparison of 2 point-of-care platelet function tests with optical aggregometry. Stroke. 2005; 36:1001–1005. PMID: 15817896.25. Cattaneo M. Aspirin and clopidogrel: efficacy, safety, and the issue of drug resistance. Arterioscler Thromb Vasc Biol. 2004; 24:1980–1987. PMID: 15388526.26. Peters BJ, Harmsze AM, ten Berg JM, Maitland-van der Zee AH, Tjoeng MM, de Boer A, et al. CYP2C19 and ABCB1 genes and individualized treatment with clopidogrel. Pharmacogenomics. 2011; 12:141–144. PMID: 21332306.27. Xie HG, Zou JJ, Hu ZY, Zhang JJ, Ye F, Chen SL. Individual variability in the disposition of and response to clopidogrel: pharmacogenomics and beyond. Pharmacol Ther. 2011; 129:267–289. PMID: 20965214.28. Bouman HJ, Schömig E, van Werkum JW, Velder J, Hackeng CM, Hirschhäuser C, et al. Paraoxonase-1 is a major determinant of clopidogrel efficacy. Nat Med. 2011; 17:110–116. PMID: 21170047.29. Arméro S, Camoin Jau L, Omar Aït Mokhtar O, Mancini J, Burignat-Bonello C, Tahirou I, et al. Intra-individual variability in clopidogrel responsiveness in coronary artery disease patients under long term therapy. Platelets. 2010; 21:503–507. PMID: 20670107.30. Wijeyeratne YD, Heptinstall S. Anti-platelet therapy: ADP receptor antagonists. Br J Clin Pharmacol. 2011; 72:647–657. PMID: 21518389.31. Blaicher AM, Landsteiner HT, Zwerina J, Leitgeb U, Volf I, Hoerauf K. Effect of non-selective, non-steroidal anti-inflammatory drugs and cyclo-oxygenase-2 selective inhibitors on the PFA-100 closure time. Anaesthesia. 2004; 59:1100–1103. PMID: 15479319.32. Favaloro EJ. Clinical utility of the PFA-100. Semin Thromb Hemost. 2008; 34:709–733. PMID: 19214910.33. Angchaisuksiri P. Cancer-associated thrombosis in Asia. Thromb J. 2016; 14(Suppl 1):26. PMID: 27766052.34. Mahé I, Chidiac J, Helfer H, Noble S. Factors influencing adherence to clinical guidelines in the management of cancer-associated thrombosis. J Thromb Haemost. 2016; 14:2107–2113. PMID: 27566698.35. Caine GJ, Stonelake PS, Lip GY, Kehoe ST. The hypercoagulable state of malignancy: pathogenesis and current debate. Neoplasia. 2002; 4:465–473. PMID: 12407439.36. Falanga A, Marchetti M, Vignoli A. Coagulation and cancer: biological and clinical aspects. J Thromb Haemost. 2013; 11:223–233. PMID: 23279708.37. Nierodzik ML, Klepfish A, Karpatkin S. Role of platelets, thrombin, integrin IIb-IIIa, fibronectin and von Willebrand factor on tumor adhesion in vitro and metastasis in vivo. Thromb Haemost. 1995; 74:282–290. PMID: 8578473.38. Lima LG, Monteiro RQ. Activation of blood coagulation in cancer: implications for tumour progression. Biosci Rep. 2013; 33:e00064. PMID: 23889169.39. Falanga A, Panova-Noeva M, Russo L. Procoagulant mechanisms in tumour cells. Best Pract Res Clin Haematol. 2009; 22:49–60. PMID: 19285272.40. Lee MS, Kim DB, Kim SK, Yoo KY, Kim HJ, Lee SH, et al. Prevalence of possible von Willebrand disease. Clin Pediatr Hematol Oncol. 2014; 21:16–22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bleeding time: Remained or Retired or Removed?
- Diagnostic workup of inherited platelet disorders
- Integration of an MC-80 Digital Image Analyzer With an Automated BC-6800Plus Hematology Analyzer Enables Accurate Platelet Counting in Samples With EDTA-Induced Pseudothrombocytopenia
- Effect of Platelet Transfusion on the Platelet Parameters of Recipient
- A Case of Platelet Satellitism with Platelet Phagocytosis by Neutrophils and Platelet-neutrophil Agglutination