J Korean Soc Radiol.
2010 Aug;63(2):107-113.
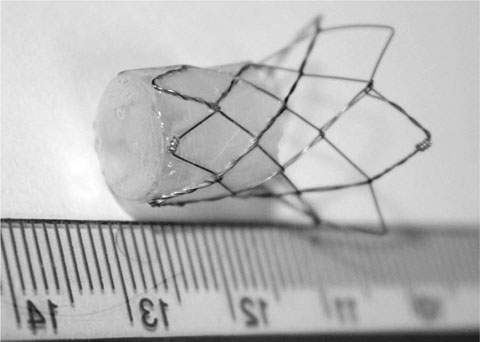
Endobronchial Occlusion Stent: A Preliminary Experimental Study
- Affiliations
-
- 1Department of Radiology, Hanyang University Medical School, Seoul, Korea. ywchoi@hanyang.ac.kr
- 2Department of Radiology, University of Ulsan College of Medicine, Asan Medical Center, Korea.
Abstract
- PURPOSE
To evaluate the safety and the technical feasibility of the use of an endobronchial occlusion stent and to get preliminary data for the development of the optimal material required for endobronchial occlusions.
MATERIALS AND METHODS
A commercialized, self-expandable tracheobronchial stent was modified; one half had a polyurethane cover with an occluded end and the other half was uncovered with a flaring configuration. The occluded end was placed such that it would face the distal lung. Under fluoroscopic guidance, seven stents were placed at the lower lobar bronchus in 6 mini-pigs. The bronchial obstruction was examined immediately after stent placement. Chest radiographs were taken at days 1, 7, 14, and 28 after stent placement and the removed airways from two, two, one, and one mini-pigs sacrificed on corresponding days were examined for the maintenance of bronchial obstruction.
RESULTS
Stents were successfully placed and induced the immediate bronchial obstruction in all mini-pigs. Five of seven airways with occlusion stents maintained an obstruction until the mini-pigs were sacrificed. Proximal stent migration occurred in two mini-pigs (29%), and pulmonary consolidations were observed distal to four of the stents (57%).
CONCLUSION
The placement of an endobronchial occlusion stent and the obstruction of targeted bronchi seem to be feasible, but an add-on check valve should be considered to prevent stent migration and obstructive pneumonia.
MeSH Terms
Figure
Reference
-
1. Iseman MD, Madsen L, Goble M, Pomerantz M. Surgical intervention in the treatment of pulmonary disease caused by drug-resistant Mycobacterium tuberculosis. Am Rev Respir Dis. 1990; 141:623–625.2. Kir A, Tahaoglu K, Okur E, Hatipoglu T. Role of surgery in multidrug-resistant tuberculosis: results of 27 cases. Eur J Cardiothorac Surg. 1997; 12:531–534.3. Sung SW, Kang CH, Kim YT, Han SK, Shim YS, Kim JH. Surgery increased the chance of cure in multi-drug resistant pulmonary tuberculosis. Eur J Cardiothorac Surg. 1999; 16:187–193.4. Weissberg D. Late complications of collapse therapy for pulmonary tuberculosis. Chest. 2001; 120:847–851.5. Ponn RB, D'Agostino RS, Stern H, Westcott JL. Treatment of peripheral bronchopleural fistulas with endobronchial occlusion coils. Ann Thorac Surg. 1993; 56:1343–1347.6. Uchida T, Wada M, Sakamoto J, Arai Y. Treatment for empyema with bronchopleural fistulas using endobronchial occlusion coils: report of a case. Surg Today. 1999; 29:186–189.7. Courtheoux P, Letourneux M, Jehan A, Theron J. Use of a detachable 2-compartment balloon in the treatment of a bronchopleural fistula. Apropos of a case. Ann Radiol. 1985; 28:560–556.8. Pace R, Rankin RN, Finley RJ. Detachable balloon occlusion of bronchopleural fistulae in dogs. Invest Radiol. 1983; 18:504–506.9. Houpt P, Van Zanten JJ, Bins MC. The use of balloon catheters in the treatment of high-flow bronchopleural fistulae complicating mechanical ventilation. Neth J Med. 1983; 26:34–38.10. Glover W, Chavis TV, Daniel TM, Kron IL, Spotnitz WD. Fibrin glue application through the flexible fiberoptic bronchoscope: closure of bronchopleural fistulas. J Thorac Cardiovasc Surg. 1987; 93:470–472.11. Ribet ME. Bronchopleural fistula: the use of tissue glue. J Thorac Cardiovasc Surg. 1994; 107:631–632.12. Travaline JM, McKenna RJ Jr, De Giacomo T, Venuta F, Hazelrigg SR, Boomer M, et al. Treatment of persistent pulmonary air leaks using endobronchial valves. Chest. 2009; 136:355–360.13. Toma TP, Kon OM, Oldfield W, Sanefuji R, Griffiths M, Wells F, et al. Reduction of persistent air leak with endoscopic valve implants. Thorax. 2007; 62:830–833.14. Singh SS, Pyragius MD, Shah PJ, Stubberfield J, Jurisevic CA, Chaloob S. Management of a large bronchopleural fistula using a tracheobronchial stent. Heart Lung Circ. 2007; 16:57–59.15. Mitchell KM, Boley TM, Hazelrigg SR. Endobronchial valves for treatment of bronchopleural fistula. Ann Thorac Surg. 2006; 81:1129–1131.16. Hopkinson NS, Toma TP, Hansell DM, Goldstraw P, Moxham J, Geddes DM, et al. Effect of bronchoscopic lung volume reduction on dynamic hyperinflation and exercise in emphysema. Am J Respir Crit Care Med. 2005; 171:453–460.17. Snell GI, Holsworth L, Borrill ZL, Thomson KR, Kalff V, Smith JA, et al. The potential for bronchoscopic lung volume reduction using bronchial prostheses: a pilot study. Chest. 2003; 124:1073–1080.18. Venuta F, de Giacomo T, Rendina EA, Ciccone AM, Diso D, Perrone A, et al. Bronchoscopic lung-volume reduction with one-way valves in patients with heterogenous emphysema. Ann Thorac Surg. 2005; 79:411–416.19. Yim AP, Hwong TM, Lee TW, Li WW, Lam S, Yeung TK, et al. Early results of endoscopic lung volume reduction for emphysema. J Thorac Cardiovasc Surg. 2004; 127:1564–1573.20. Song HY, Shim TS, Kang SG, Jung GS, Lee DY, Kim TH, et al. Tracheobronchial strictures: treatment with a polyurethane-covered retrievable expandable nitinol stent--initial experience. Radiology. 1999; 213:905–912.21. Ratliff JL, Hill JD, Tucker H, Fallat R. Endobronchial control of bronchopleural fistulae. Chest. 1977; 71:98–99.22. Hwang JC, Song HY, Kang SG, Suh JH, Ko GY, Lee DH, et al. Covered retrievable tracheobronchial hinged stent: an experimental study in dogs. J Vasc Interv Radiol. 2001; 12:1429–1436.23. Bolliger CT, Wyser C, Wu X, Hauser R, Studer W, Dalquen P, et al. Evaluation of a new self-expandable silicone stent in an experimental tracheal stenosis. Chest. 1999; 115:496–501.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous retrieval of a misplaced transjugular intrahepatic portosystemic shunt stent using the rigid endobronchial forceps
- A Case of Complication of Expandible Metallic Stent with Endobronchial Stenosis
- In-stent Radiofrequency Ablation for Tumor Ingrowth Causing Self-expandable Metal Stent Occlusion
- Preliminary Result of Intracoronary Stenting in Thrombus Containing Lesion
- Two cases of self expandable stent implantation in patient with occlusive restenosis of brachiocephalic vein stent