Yonsei Med J.
2017 Sep;58(5):988-993. 10.3349/ymj.2017.58.5.988.
Significance of Neutrophil-to-Lymphocyte Ratio as a Novel Indicator of Spontaneous Ureter Stone Passage
- Affiliations
-
- 1Department of Urology, Yonsei University College of Medicine, Seoul, Korea. GCKOO@yuhs.ac
- KMID: 2418935
- DOI: http://doi.org/10.3349/ymj.2017.58.5.988
Abstract
- PURPOSE
Stone size and location are generally considered the most important factors associated with spontaneous ureter stone passage (SSP). Several parameters related to inflammatory changes have been identified as predictors associated with SSP. Our aim was to investigate the predictive role of neutrophil-to-lymphocyte ratio (NLR) for SSP.
MATERIALS AND METHODS
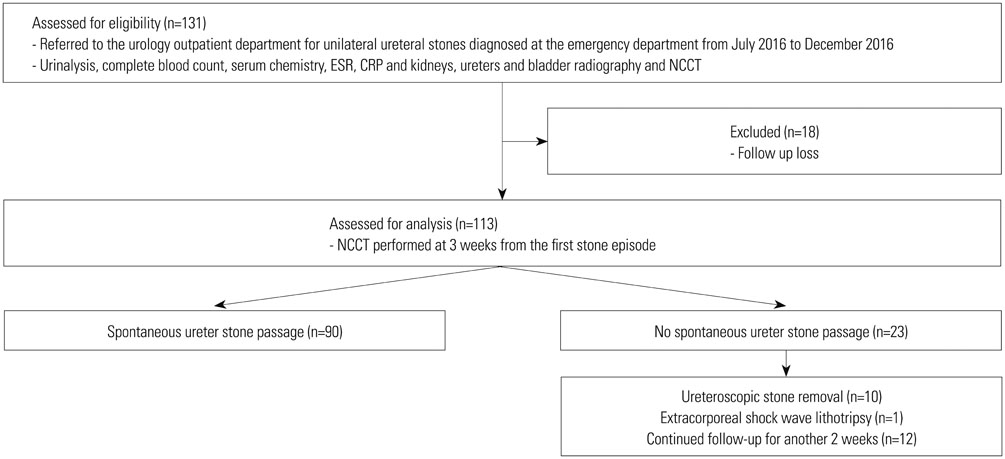
A retrospective review was performed on 131 patients who were referred to the urology outpatient clinic and diagnosed with unilateral ureteral stones at our emergency department between July 2016 and December 2016. The presence of ureteral stones was confirmed with non-contrast-enhanced computed tomography (NCCT) for all patients. SSP was confirmed with either the patient collecting the stone during urination or by NCCT performed at 3 weeks from the first stone episode. Physical examination, urinalysis, complete blood count, serum chemistry and inflammatory markers, plain radiographs, and NCCT at initial presentation were reviewed to analyze predictors of future SSP.
RESULTS
Of 113 patients included for analysis, 90 (79.6%) passed their stones spontaneously. The SSP rates within 3 weeks according to the stone's size (5-10 mm and ≤5 mm) were 62.2% and 88.2%, respectively. A lower stone location [odds ratio (OR), 11.54; p=0.001], smaller stone size (≤5 mm) (OR, 8.16; p=0.001), and NLR (<2.3) (OR, 9.03; p=0.003) were independent predictors of SSP.
CONCLUSION
Low NLR (<2.3) may predict SSP in patients with ureter stones ×1.0 cm in size. Our results suggest that ureteral inflammation plays an important role in SSP. Early intervention may be considered for patients presenting with high NLR (≥2.3).
Keyword
MeSH Terms
Figure
Reference
-
1. Dellabella M, Milanese G, Muzzonigro G. Efficacy of tamsulosin in the medical management of juxtavesical ureteral stones. J Urol. 2003; 170(6 Pt 1):2202–2205.
Article2. Aldaqadossi HA. Stone expulsion rate of small distal ureteric calculi could be predicted with plasma C-reactive protein. Urolithiasis. 2013; 41:235–239.
Article3. Sfoungaristos S, Kavouras A, Katafigiotis I, Perimenis P. Role of white blood cell and neutrophil counts in predicting spontaneous stone passage in patients with renal colic. BJU Int. 2012; 110(8 Pt B):E339–E345.
Article4. Park CH, Ha JY, Park CH, Kim CI, Kim KS, Kim BH. Relationship between spontaneous passage rates of ureteral stones less than 8 mm and serum C-reactive protein levels and neutrophil percentages. Korean J Urol. 2013; 54:615–618.
Article5. Özcan C, Aydogğdu O, Senocak C, Damar E, Eraslan A, Oztuna D, et al. Predictive factors for spontaneous stone passage and the potential role of serum C-reactive protein in patients with 4 to 10 mm distal ureteral stones: a prospective clinical study. J Urol. 2015; 194:1009–1013.
Article6. Ibrahim AI, Shetty SD, Awad RM, Patel KP. Prognostic factors in the conservative treatment of ureteric stones. Br J Urol. 1991; 67:358–361.
Article7. Ahmed AF, Gabr AH, Emara AA, Ali M, Abdel-Aziz AS, Alshahrani S. Factors predicting the spontaneous passage of a ureteric calculus of <10 mm. Arab J Urol. 2015; 13:84–90.
Article8. Fazlioglu A, Salman Y, Tandogdu Z, Kurtulus FO, Bas S, Cek M. The effect of smoking on spontaneous passage of distal ureteral stones. BMC Urol. 2014; 14:27.
Article9. Assasi N, Blackhouse G, Campbell K, Hopkins RB, Levine M, Richter T, et al. Comparative value of erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) testing in combination versus individually for the diagnosis of undifferentiated patients with suspected inflammatory disease or serious infection: a systematic review and economic analysis. Ottawa, ON: Canadian Agency for Drugs and Technologies in Health;2015.10. Baetta R, Corsini A. Role of polymorphonuclear neutrophils in atherosclerosis: current state and future perspectives. Atherosclerosis. 2010; 210:1–13.
Article11. Balta S, Celik T, Mikhailidis DP, Ozturk C, Demirkol S, Aparci M, et al. The relation between atherosclerosis and the neutrophil-lymphocyte ratio. Clin Appl Thromb Hemost. 2016; 22:405–411.
Article12. Preminger GM, Tiselius HG, Assimos DG, Alken P, Buck AC, Gallucci M, et al. 2007 Guideline for the management of ureteral calculi. Eur Urol. 2007; 52:1610–1631.
Article13. Morse RM, Resnick MI. Ureteral calculi: natural history and treatment in an era of advanced technology. J Urol. 1991; 145:263–265.
Article14. Hübner WA, Irby P, Stoller ML. Natural history and current concepts for the treatment of small ureteral calculi. Eur Urol. 1993; 24:172–176.
Article15. Siegel C. Relationship of spontaneous passage of ureteral calculi to stone size and location as revealed by unenhanced helical CT. J Urol. 2002; 168(4 Pt 1):1644.16. Segura JW, Preminger GM, Assimos DG, Dretler SP, Kahn RI, Lingeman JE, et al. Ureteral stones clinical guidelines panel summary report on the management of ureteral calculi. The American Urological Association. J Urol. 1997; 158:1915–1921.
Article17. Gibson PH, Croal BL, Cuthbertson BH, Small GR, Ifezulike AI, Gibson G, et al. Preoperative neutrophil-lymphocyte ratio and outcome from coronary artery bypass grafting. Am Heart J. 2007; 154:995–1002.
Article18. Hung HY, Chen JS, Yeh CY, Changchien CR, Tang R, Hsieh PS, et al. Effect of preoperative neutrophil-lymphocyte ratio on the surgical outcomes of stage II colon cancer patients who do not receive adjuvant chemotherapy. Int J Colorectal Dis. 2011; 26:1059–1065.
Article19. Kim HS, Han KH, Chung HH, Kim JW, Park NH, Song YS, et al. Neutrophil to lymphocyte ratio for preoperative diagnosis of uterine sarcomas: a case-matched comparison. Eur J Surg Oncol. 2010; 36:691–698.
Article20. Proctor MJ, Morrison DS, Talwar D, Balmer SM, Fletcher CD, O'Reilly DS, et al. A comparison of inflammation-based prognostic scores in patients with cancer. A Glasgow Inflammation Outcome Study. Eur J Cancer. 2011; 47:2633–2641.
Article21. Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, Terjanian T, et al. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol. 2012; 19:217–224.
Article22. Forget P, Khalifa C, Defour JP, Latinne D, Van Pel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes. 2017; 10:12.
Article23. Azab B, Camacho-Rivera M, Taioli E. Average values and racial differences of neutrophil lymphocyte ratio among a nationally representative sample of United States subjects. PLoS One. 2014; 9:e112361.
Article24. Takahashi N, Kawashima A, Ernst RD, Boridy IC, Goldman SM, Benson GS, et al. Ureterolithiasis: can clinical outcome be predicted with unenhanced helical CT? Radiology. 1998; 208:97–102.
Article25. Cervenàkov I, Fillo J, Mardiak J, Kopecný M, Smirala J, Lepies P. Speedy elimination of ureterolithiasis in lower part of ureters with the alpha 1-blocker--Tamsulosin. Int Urol Nephrol. 2002; 34:25–29.26. Williams RE. Long-term survey of 538 patients with upper urinary tract stone. Br J Urol. 1963; 35:416–437.27. Blacklock NJ. The pattern of urolithiasis in the Royal Navy. J R Nav Med Serv. 1965; 51:99–111.
Article28. Borghi L, Meschi T, Amato F, Briganti A, Novarini A, Giannini A. Urinary volume, water and recurrences in idiopathic calcium nephrolithiasis: a 5-year randomized prospective study. J Urol. 1996; 155:839–843.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous passage of ureteral stone by conservative treatment
- Spontaneous passage of ureteral stone by conservative treatment
- Correlation between the size of the ureter stone and the neutrophil-lymphocyte ratio, platelet lymphocyte ratio, and C-reactive protein in patients with ureter stone visiting the emergency department
- Relationship Between Spontaneous Passage Rates of Ureteral Stones Less Than 8 mm and Serum C-Reactive Protein Levels and Neutrophil Percentages
- Expectant Management of Ureter Stones: Outcome and Clinical Factors of Spontaneous Passage in a Single Institution's Experience