Yonsei Med J.
2018 Jan;59(1):162-166. 10.3349/ymj.2018.59.1.162.
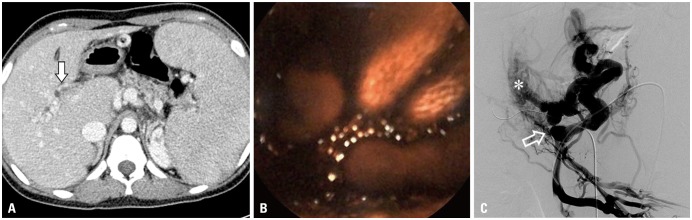
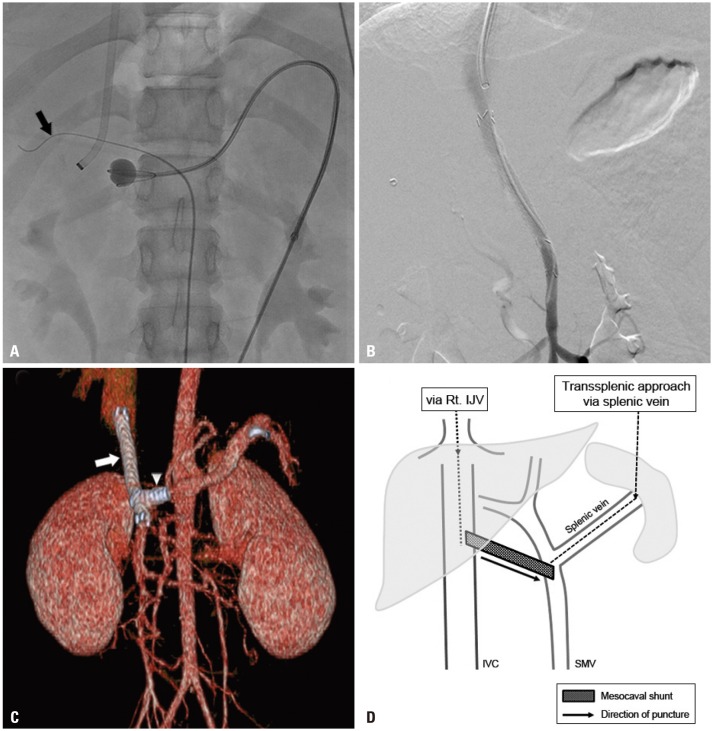
Mesocaval Shunt Creation for Jejunal Variceal Bleeding with Chronic Portal Vein Thrombosis
- Affiliations
-
- 1Department of Radiology, Severance Hospital, Research Institute of Radiological Science, Yonsei University College of Medicine, Seoul, Korea. mdkim@yuhs.ac
- 2Department of Pediatric Surgery, Severance Children's Hospital, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2418865
- DOI: http://doi.org/10.3349/ymj.2018.59.1.162
Abstract
- The creation of transjugular intrahepatic portosystemic shunt (TIPS) is a widely performed technique to relieve portal hypertension, and to manage recurrent variceal bleeding and refractory ascites in patients where medical and/or endoscopic treatments have failed. However, portosystemic shunt creation can be challenging in the presence of chronic portal vein occlusion. In this case report, we describe a minimally invasive endovascular mesocaval shunt creation with transsplenic approach for the management of recurrent variceal bleeding in a portal hypertension patient with intra- and extrahepatic portal vein occlusion.
Keyword
MeSH Terms
-
Adolescent
Chronic Disease
Esophageal and Gastric Varices/*complications/diagnostic imaging/*therapy
Female
Gastrointestinal Hemorrhage/*complications/diagnostic imaging/*therapy
Humans
Jejunum/*pathology
*Portacaval Shunt, Surgical
Portal Vein/diagnostic imaging/*pathology/surgery
Tomography, X-Ray Computed
Treatment Outcome
Venous Thrombosis/*complications/diagnostic imaging/*therapy
Figure
Reference
-
1. Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W;. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007; 46:922–938. PMID: 17879356.
Article2. Stine JG, Shah NL, Argo CK, Pelletier SJ, Caldwell SH, Northup PG. Increased risk of portal vein thrombosis in patients with cirrhosis due to nonalcoholic steatohepatitis. Liver Transpl. 2015; 21:1016–1021. PMID: 25845711.
Article3. Wils A, van der, van Hoek B, Pattynama PM. Transjugular intrahepatic portosystemic shunt in patients with chronic portal vein occlusion and cavernous transformation. J Clin Gastroenterol. 2009; 43:982–984. PMID: 19417681.
Article4. Nyman UR, Semba CP, Chang H, Hoffman C, Dake MD. Percutaneous creation of a mesocaval shunt. J Vasc Interv Radiol. 1996; 7:769–773. PMID: 8897349.
Article5. Hong R, Dhanani RS, Louie JD, Sze DY. Intravascular ultrasoundguided mesocaval shunt creation in patients with portal or mesenteric venous occlusion. J Vasc Interv Radiol. 2012; 23:136–141. PMID: 22221479.
Article6. Burke C, Taylor AG, Ring EJ, Kerlan RK Jr. Creation of a percutaneous mesocaval shunt to control variceal bleeding in a child. Pediatr Radiol. 2013; 43:1218–1220. PMID: 23447003.
Article7. Bercu ZL, Sheth SB, Noor A, Lookstein RA, Fischman AM, Nowakowski FS, et al. Percutaneous mesocaval shunt creation in a patient with chronic portal and superior mesenteric vein thrombosis. Cardiovasc Intervent Radiol. 2015; 38:1316–1319. PMID: 25189666.
Article8. Moriarty JM, Kokabi N, Kee ST. Transvenous creation of a mesocaval shunt: report of use in the management of extrahepatic portal vein occlusion. J Vasc Interv Radiol. 2012; 23:565–567. PMID: 22464719.
Article9. Davis J, Chun AK, Borum ML. Could there be light at the end of the tunnel? Mesocaval shunting for refractory esophageal varices in patients with contraindications to transjugular intrahepatic portosystemic shunt. World J Hepatol. 2016; 8:790–795. PMID: 27429715.
Article10. Chu HH, Kim HC, Jae HJ, Yi NJ, Lee KW, Suh KS, et al. Percutaneous transsplenic access to the portal vein for management of vascular complication in patients with chronic liver disease. Cardiovasc Intervent Radiol. 2012; 35:1388–1395. PMID: 22159907.
Article11. Bertram H, Pfister ED, Becker T, Schoof S. Transsplenic endovascular therapy of portal vein stenosis and subsequent complete portal vein thrombosis in a 2-year-old child. J Vasc Interv Radiol. 2010; 21:1760–1764. PMID: 20884237.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transjugular Intrahepatic Portosystemic Shunt in Patients with Active Variceal Bleeding Due to Portal Hypertension and Portal Vein Thrombosis
- Effect of Transjugular Intrahepatic Portosystemic Shunt for Variceal bleeding in Hepatocellular Carcinoma Patients with Portal Vein Thrombosis
- Clinical Results of the Transjugular Intrahepatic Portosystemic Shunt
- Successful use of a mesocaval shunt to treat refractory ascites in a chronic pancreatitis induced portal vein thrombosis
- A Case of Extrahepatic Portal Vein Thrombosis Treated by Transjugular Intrahepatic Portosystemic Shunt ( TIPS )