Yonsei Med J.
2018 Mar;59(2):243-251. 10.3349/ymj.2018.59.2.243.
Effects of Physician Volume on Readmission and Mortality in Elderly Patients with Heart Failure: Nationwide Cohort Study
- Affiliations
-
- 1Department of Public Health, Yonsei University College of Medicine, Seoul, Korea.
- 2Institute of Health Services Research, Yonsei University College of Medicine, Seoul, Korea. thkim@yuhs.ac
- 3Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 4Department of Preventive Medicine, Eulji University College of Medicine, Daejeon, Korea.
- 5Department of Hospital Administration, Graduate School of Public Health, Yonsei University, Seoul, Korea.
- KMID: 2418787
- DOI: http://doi.org/10.3349/ymj.2018.59.2.243
Abstract
- PURPOSE
Readmission and mortality rates of patients with heart failure are good indicators of care quality. To determine whether hospital resources are associated with care quality for cardiac patients, we analyzed the effect of number of physicians and the combined effects of number of physicians and beds on 30-day readmission and 1-year mortality.
MATERIALS AND METHODS
We used national cohort sample data of the National Health Insurance Service (NHIS) claims in 2002-2013. Subjects comprised 2345 inpatients (age: >65 years) admitted to acute-care hospitals for heart failure. A multivariate Cox regression was used.
RESULTS
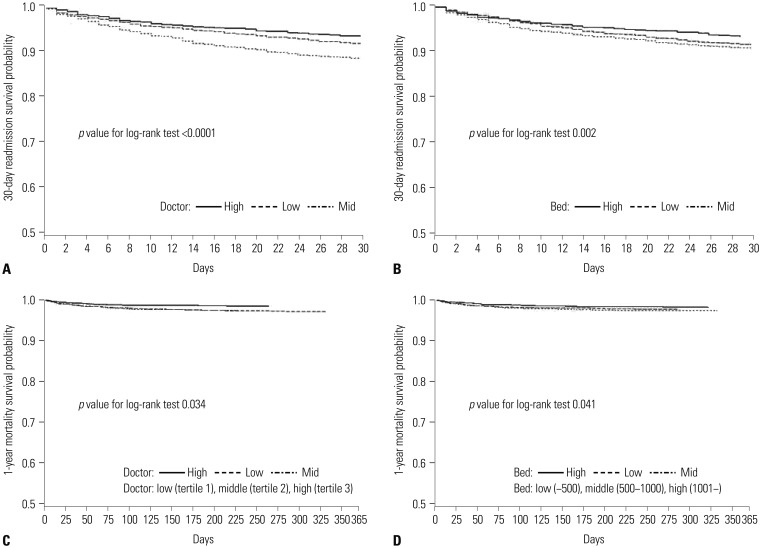
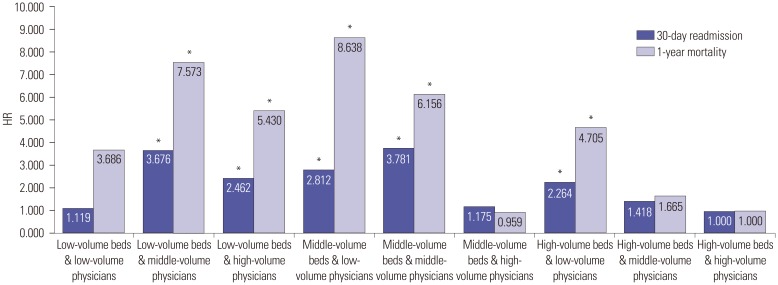
Of the 2345 patients hospitalized with heart failure, 812 inpatients (34.6%) were readmitted within 30 days and 190 (8.1%) had died within a year. Heart-failure patients treated at hospitals with low physician volumes had higher readmission and mortality rates than high physician volumes [30-day readmission: hazard ratio (HR)=1.291, 95% confidence interval (CI)=1.020-1.633; 1-year mortality: HR=2.168, 95% CI=1.415-3.321]. Patients admitted to hospitals with low or middle bed and physician volume had higher 30-day readmission and 1-year mortality rates than those admitted to hospitals with high volume (30-day readmission: HR=2.812, 95% CI=1.561-5.066 for middle-volume beds & low-volume physicians, 1-year mortality: HR=8.638, 95% CI=2.072-36.02 for middle-volume beds & low-volume physicians).
CONCLUSION
Physician volume is related to lower readmission and mortality for heart failure. Of interest, 30-day readmission and 1-year mortality were significantly associated with the combined effects of physician and institution bed volume.
Keyword
MeSH Terms
-
Aged
Aged, 80 and over
Cohort Studies
Female
Heart Failure/diagnosis/*mortality/therapy
Hospitalization
*Hospitals, High-Volume/statistics & numerical data
*Hospitals, Low-Volume/statistics & numerical data
Humans
Male
Middle Aged
Patient Readmission/*statistics & numerical data
Physicians/economics/*supply & distribution
Proportional Hazards Models
Quality Improvement
Quality Indicators, Health Care/*statistics & numerical data
Time Factors
Treatment Outcome
Figure
Reference
-
1. Keenan PS, Normand SL, Lin Z, Drye EE, Bhat KR, Ross JS, et al. An administrative claims measure suitable for profiling hospital performance on the basis of 30-day all-cause readmission rates among patients with heart failure. Circ Cardiovasc Qual Outcomes. 2008; 1:29–37. PMID: 20031785.
Article2. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009; 360:1418–1428. PMID: 19339721.
Article3. Ross JS, Chen J, Lin Z, Bueno H, Curtis JP, Keenan PS, et al. Recent national trends in readmission rates after heart failure hospitalization. Circ Heart Fail. 2010; 3:97–103. PMID: 19903931.
Article4. Jung HJ. Practice patterns for patients with heart failure. National Health Insurance Service;2014. accessed on 2016 April 20. Avaliable at: https://eiec.kdi.re.kr/skin_2016/common/epicdownload.jsp?num=135717&filenum=1.5. Kim SJ, Park EC, Kim TH, Yoo JW, Lee SG. Mortality, length of stay, and inpatient charges for heart failure patients at public versus private hospitals in South Korea. Yonsei Med J. 2015; 56:853–861. PMID: 25837196.
Article6. Choi DJ, Han S, Jeon ES, Cho MC, Kim JJ, Yoo BS, et al. Characteristics, outcomes and predictors of long-term mortality for patients hospitalized for acute heart failure: a report from the Korean Heart Failure Registry. Korean Circ J. 2011; 41:363–371. PMID: 21860637.
Article7. Padhukasahasram B, Reddy CK, Li Y, Lanfear DE. Joint impact of clinical and behavioral variables on the risk of unplanned readmission and death after a heart failure hospitalization. PLoS One. 2015; 10:e0129553. PMID: 26042868.
Article8. Korea Health Industry Development Institute. Guidelines for hospital evaluation program 2009. Ministry of Health and Welfare;2009. p. 254.9. Chen Y, Stewart P, Dales R, Johansen H, Scott G, Taylor G. Ecological measures of socioeconomic status and hospital readmissions for asthma among Canadian adults. Respir Med. 2004; 98:446–453. PMID: 15139574.
Article10. Joynt KE, Orav EJ, Jha AK. Physician volume, specialty, and outcomes of care for patients with heart failure. Circ Heart Fail. 2013; 6:890–897. PMID: 23926203.
Article11. Birkmeyer JD, Stukel TA, Siewers AE, Goodney PP, Wennberg DE, Lucas FL. Surgeon volume and operative mortality in the United States. N Engl J Med. 2003; 349:2117–2127. PMID: 14645640.
Article12. Hu JC, Gold KF, Pashos CL, Mehta SS, Litwin MS. Role of surgeon volume in radical prostatectomy outcomes. J Clin Oncol. 2003; 21:401–405. PMID: 12560426.
Article13. Moscucci M, Share D, Smith D, O'Donnell MJ, Riba A, McNamara R, et al. Relationship between operator volume and adverse outcome in contemporary percutaneous coronary intervention practice: an analysis of a quality-controlled multicenter percutaneous coronary intervention clinical database. J Am Coll Cardiol. 2005; 46:625–632. PMID: 16098426.
Article14. Krumholz HM, Merrill AR, Schone EM, Schreiner GC, Chen J, Bradley EH, et al. Patterns of hospital performance in acute myocardial infarction and heart failure 30-day mortality and readmission. Circ Cardiovasc Qual Outcomes. 2009; 2:407–413. PMID: 20031870.
Article15. Bueno H, Ross JS, Wang Y, Chen J, Vidàn MT, Normand SL, et al. Trends in length of stay and short-term outcomes among Medicare patients hospitalized for heart failure, 1993-2006. JAMA. 2010; 303:2141–2147. PMID: 20516414.
Article16. OECD. OECD Health Statistics 2016. 2016.17. Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heidenreich PA, Yancy CW, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010; 303:1716–1722. PMID: 20442387.
Article18. Dharmarajan K, Hsieh AF, Lin Z, Bueno H, Ross JS, Horwitz LI, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. JAMA. 2013; 309:355–363. PMID: 23340637.
Article19. Krumholz HM, Lin Z, Keenan PS, Chen J, Ross JS, Drye EE, et al. Relationship between hospital readmission and mortality rates for patients hospitalized with acute myocardial infarction, heart failure, or pneumonia. JAMA. 2013; 309:587–593. PMID: 23403683.
Article20. Mentz RJ, Cotter G, Cleland JG, Stevens SR, Chiswell K, Davison BA, et al. International differences in clinical characteristics, management, and outcomes in acute heart failure patients: better short-term outcomes in patients enrolled in Eastern Europe and Russia in the PROTECT trial. Eur J Heart Fail. 2014; 16:614–624. PMID: 24771609.
Article21. Weller WE, Rosati C, Hannan EL. Relationship between surgeon and hospital volume and readmission after bariatric operation. J Am Coll Surg. 2007; 204:383–391. PMID: 17324771.
Article22. Mesman R, Westert GP, Berden BJ, Faber MJ. Why do high-volume hospitals achieve better outcomes? A systematic review about intermediate factors in volume-outcome relationships. Health Policy. 2015; 119:1055–1067. PMID: 25958187.
Article23. Nuttall M, van der Meulen J, Phillips N, Sharpin C, Gillatt D, Mc-Intosh G, et al. A systematic review and critique of the literature relating hospital or surgeon volume to health outcomes for 3 urological cancer procedures. J Urol. 2004; 172(6 Pt 1):2145–2152. PMID: 15538220.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In-Hospital Mortality Rate and Predictors of 30-Day Readmission in Patients With Heart Failure Exacerbation and Atrial Fibrillation: A Cross-Sectional Study
- Hospital Case Volume, Health Care Providers, and Mortality in Patients Undergoing Coronary Artery Bypass Grafting: a Nationwide Cohort Study in South Korea
- How to tackle congestion in acute heart failure
- Understanding the Epidemiologic Profile and Predictors of Readmission of Heart Failure: Unveiling Opportunities for Improved Care
- Trends in Ischemic Heart Disease Mortality in Korea, 1985-2009: An Age-period-cohort Analysis