J Adv Prosthodont.
2018 Aug;10(4):259-264. 10.4047/jap.2018.10.4.259.
The effect of zirconia surface architecturing technique on the zirconia/veneer interfacial bond strength
- Affiliations
-
- 1Seoul Meerae Dental Clinic, Seoul, Republic of Korea.
- 2Korea Institute of Ceramic Engineering and Technology, Jinju, Republic of Korea.
- 3Restorative Dentistry and Biomaterials Sciences, Harvard School of Dental Medicine, Boston, MA, USA.
- 4Department of Dentistry, School of Medicine, Ewha Womans University, Seoul, Republic of Korea. prosth@ewha.ac.kr
- KMID: 2418630
- DOI: http://doi.org/10.4047/jap.2018.10.4.259
Abstract
- PURPOSE
The purpose of this study was to evaluate the effect of the zirconia surface architecturing technique (ZSAT) on the bond strength between veneering porcelain and zirconia ceramic.
MATERIALS AND METHODS
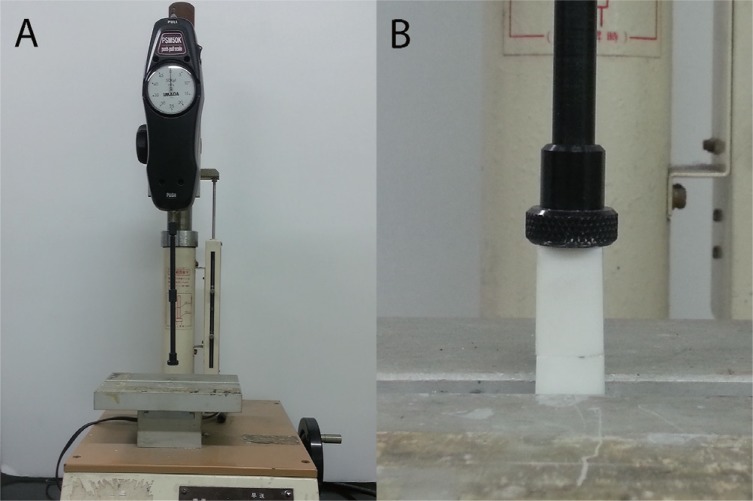
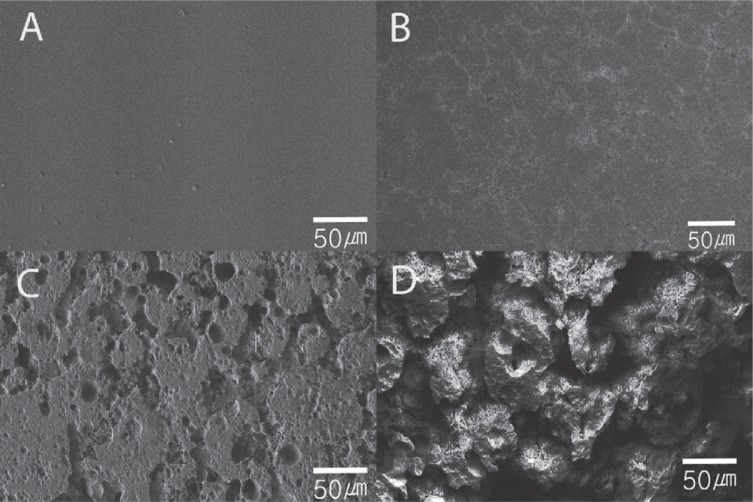
20 sintered zirconia ceramic specimens were used to determine the optimal surface treatment time, and were randomly divided into 4 groups based on treatment times of 0, 1, 2, and 3 hours. After etching with a special solution, the surface was observed under scanning electron microscope, and then the porcelain was veneered for scratch testing. Sixty 3 mol% yttria-stabilized tetragonal zirconia polycrystal ceramic blocks were used for tensile strength testing; 30 of these blocks were surface treated and the rest were not. Statistical analysis was performed using ANOVA, the Tukey post-hoc test, and independent t-test, and the level of significance was set at α=.05.
RESULTS
The surface treatment of the zirconia using ZSAT increased the surface roughness, and tensile strength test results showed that the ZSAT group significantly increased the bond strength between zirconia and veneering porcelain compared to the untreated group (36 MPa vs. 30 MPa). Optimal etching time was determined to be 2 hours based on the scratch test results.
CONCLUSION
ZSAT increases the surface roughness of zirconia, and this might contribute to the increased interfacial bond strength between zirconia and veneering porcelain.
Keyword
Figure
Cited by 1 articles
-
Effects of different surface treatments on the shear bond strength of veneering ceramic materials to zirconia
Adil Othman Abdullah, Yu Hui, Xudong Sun, Sarah Pollington, Fenik Kaml Muhammed, Yi Liu
J Adv Prosthodont. 2019;11(1):65-74. doi: 10.4047/jap.2019.11.1.65.
Reference
-
1. Piconi C, Maccauro G. Zirconia as a ceramic biomaterial. Biomaterials. 1999; 20:1–25. PMID: 9916767.
Article2. Chevalier J. What future for zirconia as a biomaterial? Biomaterials. 2006; 27:535–543. PMID: 16143387.
Article3. Koutayas SO, Vagkopoulou T, Pelekanos S, Koidis P, Strub JR. Zirconia in dentistry: part 2. Evidence-based clinical breakthrough. Eur J Esthet Dent. 2009; 4:348–380. PMID: 20111760.4. Cho JH, Kim SJ, Shim JS, Lee KW. Effect of zirconia surface treatment using nitric acid-hydrofluoric acid on the shear bond strengths of resin cements. J Adv Prosthodont. 2017; 9:77–84. PMID: 28435615.
Article5. Su N, Yue L, Liao Y, Liu W, Zhang H, Li X, Wang H, Shen J. The effect of various sandblasting conditions on surface changes of dental zirconia and shear bond strength between zirconia core and indirect composite resin. J Adv Prosthodont. 2015; 7:214–223. PMID: 26140173.
Article6. Mosharraf R, Rismanchian M, Savabi O, Ashtiani AH. Influence of surface modification techniques on shear bond strength between different zirconia cores and veneering ceramics. J Adv Prosthodont. 2011; 3:221–228. PMID: 22259706.
Article7. Sailer I, Fehér A, Filser F, Gauckler LJ, Lüthy H, Hämmerle CH. Five-year clinical results of zirconia frameworks for posterior fixed partial dentures. Int J Prosthodont. 2007; 20:383–388. PMID: 17695869.8. Molin MK, Karlsson SL. Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont. 2008; 21:223–227. PMID: 18548960.9. Sorrentino R, De Simone G, Tetè S, Russo S, Zarone F. Five-year prospective clinical study of posterior three-unit zirconia-based fixed dental prostheses. Clin Oral Investig. 2012; 16:977–985.
Article10. Ortorp A, Kihl ML, Carlsson GE. A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent. 2012; 40:527–530. PMID: 22387979.11. Vigolo P, Mutinelli S. Evaluation of zirconium-oxide-based ceramic single-unit posterior fixed dental prostheses (FDPs) generated with two CAD/CAM systems compared to porcelain-fused-to-metal single-unit posterior FDPs: a 5-year clinical prospective study. J Prosthodont. 2012; 21:265–269. PMID: 22339945.
Article12. Raigrodski AJ, Yu A, Chiche GJ, Hochstedler JL, Mancl LA, Mohamed SE. Clinical efficacy of veneered zirconium dioxide-based posterior partial fixed dental prostheses: five-year results. J Prosthet Dent. 2012; 108:214–222. PMID: 23031727.
Article13. Schmitter M, Mussotter K, Rammelsberg P, Gabbert O, Ohlmann B. Clinical performance of long-span zirconia frameworks for fixed dental prostheses: 5-year results. J Oral Rehabil. 2012; 39:552–557. PMID: 22574689.
Article14. Sax C, Hämmerle CH, Sailer I. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 2011; 14:183–202. PMID: 22141229.15. Al-Amleh B, Lyons K, Swain M. Clinical trials in zirconia: a systematic review. J Oral Rehabil. 2010; 37:641–652. PMID: 20406352.
Article16. Mackert JR Jr. Effects of thermally induced changes on porcelain-metal compatibility. In : Preston JD, editor. Perspectives in dental ceramics. Proceedings of the fourth international symposium on ceramics. Chicago: Quintessence;1988. p. 53–64.17. Isgrò G, Pallav P, van der Zel JM, Feilzer AJ. The influence of the veneering porcelain and different surface treatments on the biaxial flexural strength of a heat-pressed ceramic. J Prosthet Dent. 2003; 90:465–473. PMID: 14586311.
Article18. Murphy KM, Carter JM, Johnson RR, Sorensen SE. Determination of residual stresses in denture base polymers using the layer removal technique. J Biomed Mater Res. 1985; 19:971–980. PMID: 3880354.
Article19. de Kler M, de Jager N, Meegdes M, van der Zel JM. Influence of thermal expansion mismatch and fatigue loading on phase changes in porcelain veneered Y-TZP zirconia discs. J Oral Rehabil. 2007; 34:841–847. PMID: 17919251.
Article20. Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Effect of zirconia type on its bond strength with different veneer ceramics. J Prosthodont. 2008; 17:401–408. PMID: 18355163.
Article21. Fischer J, Stawarzcyk B, Trottmann A, Hämmerle CH. Impact of thermal misfit on shear strength of veneering ceramic/zirconia composites. Dent Mater. 2009; 25:419–423. PMID: 18990436.
Article22. Göstemeyer G, Jendras M, Dittmer MP, Bach FW, Stiesch M, Kohorst P. Influence of cooling rate on zirconia/veneer interfacial adhesion. Acta Biomater. 2010; 6:4532–4538. PMID: 20601242.
Article23. Guazzato M, Proos K, Quach L, Swain MV. Strength, reliability and mode of fracture of bilayered porcelain/zirconia (Y-TZP) dental ceramics. Biomaterials. 2004; 25:5045–5052. PMID: 15109867.
Article24. White SN, Caputo AA, Vidjak FM, Seghi RR. Moduli of rupture of layered dental ceramics. Dent Mater. 1994; 10:52–58. PMID: 7995477.
Article25. Zeng K, Odén A, Rowcliffe D. Evaluation of mechanical properties of dental ceramic core materials in combination with porcelains. Int J Prosthodont. 1998; 11:183–189. PMID: 9709610.26. Thompson GA. Influence of relative layer height and testing method on the failure mode and origin in a bilayered dental ceramic composite. Dent Mater. 2000; 16:235–243. PMID: 10831777.
Article27. Ozkurt Z, Kazazoğlu E. Clinical success of zirconia in dental applications. J Prosthodont. 2010; 19:64–68. PMID: 19754642.28. Taskonak B, Borges GA, Mecholsky JJ Jr, Anusavice KJ, Moore BK, Yan J. The effects of viscoelastic parameters on residual stress development in a zirconia/glass bilayer dental ceramic. Dent Mater. 2008; 24:1149–1155. PMID: 18329705.
Article29. Al-Dohan HM, Yaman P, Dennison JB, Razzoog ME, Lang BR. Shear strength of core-veneer interface in bi-layered ceramics. J Prosthet Dent. 2004; 91:349–355. PMID: 15116036.
Article30. Fischer J, Grohmann P, Stawarczyk B. Effect of zirconia surface treatments on the shear strength of zirconia/veneering ceramic composites. Dent Mater J. 2008; 27:448–454. PMID: 18717175.
Article31. Nakamura T, Wakabayashi K, Zaima C, Nishida H, Kinuta S, Yatani H. Tensile bond strength between tooth-colored porcelain and sandblasted zirconia framework. J Prosthodont Res. 2009; 53:116–119. PMID: 19345663.
Article32. Ozkurt Z, Kazazoglu E, Unal A. In vitro evaluation of shear bond strength of veneering ceramics to zirconia. Dent Mater J. 2010; 29:138–146. PMID: 20379023.33. Anusavice KJ, Kakar K, Ferree N. Which mechanical and physical testing methods are relevant for predicting the clinical performance of ceramic-based dental prostheses? Clin Oral Implants Res. 2007; 18:218–231. PMID: 17594384.
Article34. Fischer J, Grohmann P, Stawarczyk B. Effect of zirconia surface treatments on the shear strength of zirconia/veneering ceramic composites. Dent Mater J. 2008; 27:448–454. PMID: 18717175.
Article35. Aboushelib MN, Kleverlaan CJ, Feilzer AJ. Microtensile bond strength of different components of core veneered all-ceramic restorations. Part II: Zirconia veneering ceramics. Dent Mater. 2006; 22:857–863. PMID: 16376981.36. Sundh A, Sjögren G. A comparison of fracture strength of yttrium-oxide-partially-stabilized zirconia ceramic crowns with varying core thickness, shapes and veneer ceramics. J Oral Rehabil. 2004; 31:682–688. PMID: 15210030.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of glass-infiltration treatments on the shear bond strength between zirconia and ultra low-fusing porcelain veneer
- Repair bond strength of composite resin to zirconia restorations after different thermal cycles
- Effect of surface treatmet on the shear bond strength of a zirconia core to veneering ceramic
- Shear bond strength of veneer ceramic and colored zirconia by using aqueous metal chloride solutions
- Effect of zirconia surface treatment using nitric acid-hydrofluoric acid on the shear bond strengths of resin cements