Obstet Gynecol Sci.
2017 Nov;60(6):527-534. 10.5468/ogs.2017.60.6.527.
Safety of umbilical cord milking in very preterm neonates: a randomized controlled study
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Chungnam National University Hospital, Chungnam National University School of Medicine, Daejeon, Korea. minari73@cnuh.co.kr
- KMID: 2418353
- DOI: http://doi.org/10.5468/ogs.2017.60.6.527
Abstract
OBJECTIVE
To investigate the safety of umbilical cord milking on both the mother and neonate among very preterm deliveries of less than 33 weeks of gestation.
METHODS
Pregnant women who were expected to deliver at between 24 0/7 and 32 6/7 weeks of gestation were randomized to either the umbilical cord milking or immediate cord clamping group. Maternal and neonatal data associated with delivery, in addition to neonatal morbidity and mortality data, were collected and analyzed.
RESULTS
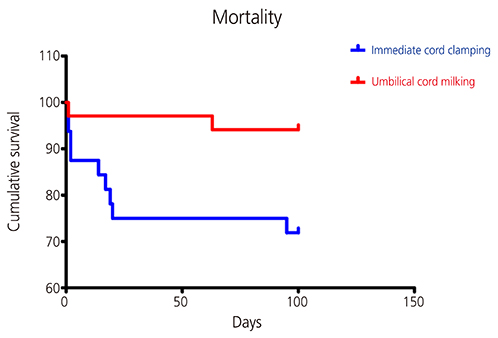
Of the 66 preterm deliveries included in the study, 34 were randomized into the milking and 32 into the clamping group. Differences between maternal pre- and post-partum hemoglobin levels were 1.35 g/dL in the milking and 1.58 g/dL in the clamping group (P=0.451). Neonatal Apgar scores at both 1 and 5 minutes, initial blood gas analysis results, body temperature at admission, need for early intubation, and maximum bilirubin levels were all similar between the 2 groups. However, neonatal hemoglobin levels at birth (15.79 vs. 14.69 g/dL; P<0.05) and at 24 hours of age (14.83 vs. 13.29 g/dL; P<0.05) were significantly higher in the milking group. Neonates in the clamping group required more blood transfusion (1.78 vs. 0.93; P=0.049), and a higher percentage of neonates in the clamping group required inotropic drugs (63% vs. 29%; P=0.007). The mortality rate was significantly lower in the milking group (6% vs. 28%; P=0.015).
CONCLUSION
Umbilical cord milking can be a safe and beneficial procedure for both the mother and the neonate in deliveries of less than 33 weeks of gestation.
MeSH Terms
Figure
Reference
-
1. Strauss RG, Mock DM, Johnson KJ, Cress GA, Burmeister LF, Zimmerman MB, et al. A randomized clinical trial comparing immediate versus delayed clamping of the umbilical cord in preterm infants: short-term clinical and laboratory endpoints. Transfusion. 2008; 48:658–665.2. Sommers R, Stonestreet BS, Oh W, Laptook A, Yanowitz TD, Raker C, et al. Hemodynamic effects of delayed cord clamping in premature infants. Pediatrics. 2012; 129:e667–e672.3. Kinmond S, Aitchison TC, Holland BM, Jones JG, Turner TL, Wardrop CA. Umbilical cord clamping and preterm infants: a randomised trial. BMJ. 1993; 306:172–175.4. Rabe H, Diaz-Rossello JL, Duley L, Dowswell T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev. 2012; CD003248.5. Mercer JS, Vohr BR, McGrath MM, Padbury JF, Wallach M, Oh W. Delayed cord clamping in very preterm infants reduces the incidence of intraventricular hemorrhage and late-onset sepsis: a randomized, controlled trial. Pediatrics. 2006; 117:1235–1242.6. Committee on Obstetric Practice, American College of Obstetricians and Gynecologists. Committee opinion no.543: timing of umbilical cord clamping after birth. Obstet Gynecol. 2012; 120:1522–1526.7. Wiberg N, Källén K, Olofsson P. Delayed umbilical cord clamping at birth has effects on arterial and venous blood gases and lactate concentrations. BJOG. 2008; 115:697–703.8. Saigal S, Usher RH. Symptomatic neonatal plethora. Biol Neonate. 1977; 32:62–72.9. Saigal S, O'Neill A, Surainder Y, Chua LB, Usher R. Placental transfusion and hyperbilirubinemia in the premature. Pediatrics. 1972; 49:406–419.10. Evans N. Assessment and support of the preterm circulation. Early Hum Dev. 2006; 82:803–810.11. Ghavam S, Batra D, Mercer J, Kugelman A, Hosono S, Oh W, et al. Effects of placental transfusion in extremely low birthweight infants: meta-analysis of long- and short-term outcomes. Transfusion. 2014; 54:1192–1198.12. Rabe H, Jewison A, Alvarez RF, Crook D, Stilton D, Bradley R, et al. Milking compared with delayed cord clamping to increase placental transfusion in preterm neonates: a randomized controlled trial. Obstet Gynecol. 2011; 117:205–211.13. Papile LA, Burstein J, Burstein R, Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978; 92:529–534.14. Kumar B, Upadhyay A, Gothwal S, Jaiswal V, Joshi P, Dubey K. Umbilical cord milking and hematological parameters in moderate to late preterm neonates: a randomized controlled trial. Indian Pediatr. 2015; 52:753–757.15. Backes CH, Rivera BK, Haque U, Bridge JA, Smith CV, Hutchon DJ, et al. Placental transfusion strategies in very preterm neonates: a systematic review and meta-analysis. Obstet Gynecol. 2014; 124:47–56.16. Hosono S, Mugishima H, Fujita H, Hosono A, Minato M, Okada T, et al. Umbilical cord milking reduces the need for red cell transfusions and improves neonatal adaptation in infants born at less than 29 weeks' gestation: a randomised controlled trial. Arch Dis Child Fetal Neonatal Ed. 2008; 93:F14–F19.17. March MI, Hacker MR, Parson AW, Modest AM, de Veciana M. The effects of umbilical cord milking in extremely preterm infants: a randomized controlled trial. J Perinatol. 2013; 33:763–767.18. Rashid N, Al-Sufayan F, Seshia MM, Baier RJ. Post transfusion lung injury in the neonatal population. J Perinatol. 2013; 33:292–296.19. Reynolds GJ. Beyond sweetness and warmth: transition of the preterm infant. Arch Dis Child Fetal Neonatal Ed. 2008; 93:F2–F3.20. Katheria AC, Truong G, Cousins L, Oshiro B, Finer NN. Umbilical cord milking versus delayed cord clamping in preterm infants. Pediatrics. 2015; 136:61–69.21. Dang D, Zhang C, Shi S, Mu X, Lv X, Wu H. Umbilical cord milking reduces need for red cell transfusions and improves neonatal adaptation in preterm infants: meta-analysis. J Obstet Gynaecol Res. 2015; 41:890–895.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Cord Clamping Compared with Cord Milking in Preterm Neonates
- Safety of delayed umbilical cord clamping in preterm neonates of less than 34 weeks of gestation: a randomized controlled trial
- Delivery Room Management: First Step to the Best Neonatal Outcome
- Umbilical Cord Arterial Concentrations of Isoprostane(8-iso-PGF2alpha) in Newborn Infants
- Effect of Umbilical Cord Milking in Extremely Low Birth Weight Infants