Obstet Gynecol Sci.
2017 Nov;60(6):520-526. 10.5468/ogs.2017.60.6.520.
Risk factors for massive postpartum bleeding in pregnancies in which incomplete placenta previa are located on the posterior uterine wall
- Affiliations
-
- 1Department of Obstetrics and Gynecology, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. lenna@hanmail.net
- KMID: 2418352
- DOI: http://doi.org/10.5468/ogs.2017.60.6.520
Abstract
OBJECTIVE
To identify factors associated with massive postpartum bleeding in pregnancies complicated by incomplete placenta previa located on the posterior uterine wall.
METHODS
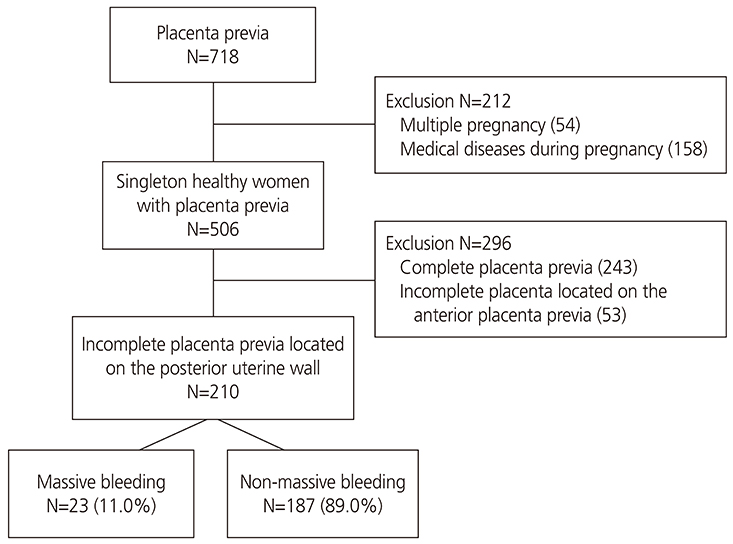
A retrospective case-control study was performed. We identified 210 healthy singleton pregnancies with incomplete placenta previa located on the posterior uterine wall, who underwent elective or emergency cesarean section after 24 weeks of gestation between January 2006 and April 2016. The cases with intraoperative blood loss (≥2,000 mL) or transfusion of packed red blood cells (≥4) or uterine artery embolization or hysterectomy were defined as massive bleeding.
RESULTS
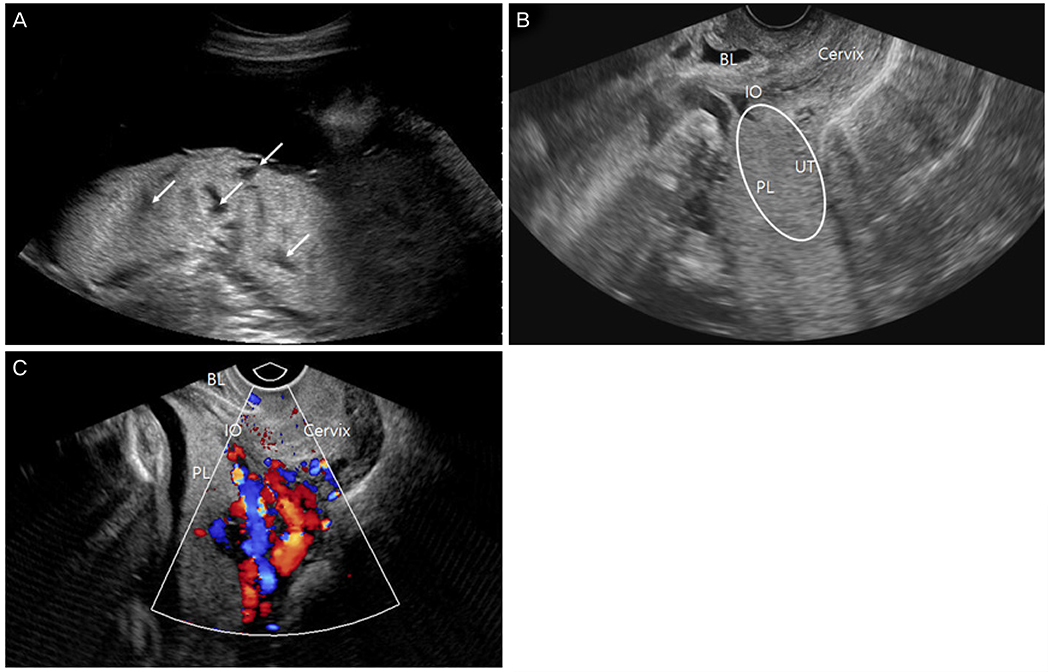
Twenty-three women experienced postpartum profuse bleeding (11.0%). After multivariable analysis, 4 variables were associated with massive postpartum hemorrhage (PPH): experience of 2 or more prior uterine curettage (adjusted odds ratio [aOR], 4.47; 95% confidence interval [CI], 1.29 to 15.48; P=0.018), short cervical length before delivery (<2.0 cm) (aOR, 7.13; 95% CI, 1.01 to 50.25; P=0.049), fetal non-cephalic presentation (aOR, 12.48; 95% CI, 1.29 to 121.24; P=0.030), and uteroplacental hypervascularity (aOR, 6.23; 95% CI, 2.30 to 8.83; P=0.001).
CONCLUSION
This is the first study of cases with incomplete placenta previa located on the posterior uterine wall, which were complicated by massive PPH. Our findings might be helpful to guide obstetric management and provide useful information for prediction of massive PPH in pregnancies with incomplete placenta previa located on the posterior uterine wall.
MeSH Terms
Figure
Reference
-
1. Placenta previa. In : Cunningham FG, Leveno KJ, Bloom SL, Spong CY, Dashe JS, Hoffman BL, editors. Williams obstetrics. 24th ed. New York (NY): McGraw-Hill Education;2014. p. 799–804.2. Lal AK, Hibbard JU. Placenta previa: an outcome-based cohort study in a contemporary obstetric population. Arch Gynecol Obstet. 2015; 292:299–305.3. Hasegawa J, Matsuoka R, Ichizuka K, Mimura T, Sekizawa A, Farina A, et al. Predisposing factors for massive hemorrhage during Cesarean section in patients with placenta previa. Ultrasound Obstet Gynecol. 2009; 34:80–84.4. Tuzovic L. Complete versus incomplete placenta previa and obstetric outcome. Int J Gynaecol Obstet. 2006; 93:110–117.5. Shevell T, Malone FD. Management of obstetric hemorrhage. Semin Perinatol. 2003; 27:86–104.6. Leduc D, Senikas V, Lalonde AB, Ballerman C, Biringer A, Delaney M, et al. Active management of the third stage of labour: prevention and treatment of postpartum hemorrhage. J Obstet Gynaecol Can. 2009; 31:980–993.7. Green L, Knight M, Seeney FM, Hopkinson C, Collins PW, Collis RE, et al. The epidemiology and outcomes of women with postpartum haemorrhage requiring massive transfusion with eight or more units of red cells: a national cross-sectional study. BJOG. 2016; 123:2164–2170.8. Oya A, Nakai A, Miyake H, Kawabata I, Takeshita T. Risk factors for peripartum blood transfusion in women with placenta previa: a retrospective analysis. J Nippon Med Sch. 2008; 75:146–151.9. Pivano A, Alessandrini M, Desbriere R, Agostini A, Opinel P, d’Ercole C, et al. A score to predict the risk of emergency caesarean delivery in women with antepartum bleeding and placenta praevia. Eur J Obstet Gynecol Reprod Biol. 2015; 195:173–176.10. Sekiguchi A, Nakai A, Kawabata I, Hayashi M, Takeshita T. Type and location of placenta previa affect preterm delivery risk related to antepartum hemorrhage. Int J Med Sci. 2013; 10:1683–1688.11. Giambattista E, Ossola MW, Duiella SF, Crovetto F, Acaia B, Somigliana E, et al. Predicting factors for emergency peripartum hysterectomy in women with placenta previa. Arch Gynecol Obstet. 2012; 285:901–906.12. Mimura T, Hasegawa J, Nakamura M, Matsuoka R, Ichizuka K, Sekizawa A, et al. Correlation between the cervical length and the amount of bleeding during cesarean section in placenta previa. J Obstet Gynaecol Res. 2011; 37:830–835.13. Hasegawa J, Nakamura M, Hamada S, Matsuoka R, Ichizuka K, Sekizawa A, et al. Prediction of hemorrhage in placenta previa. Taiwan J Obstet Gynecol. 2012; 51:3–6.14. Comstock CH, Love JJ Jr, Bronsteen RA, Lee W, Vettraino IM, Huang RR, et al. Sonographic detection of placenta accreta in the second and third trimesters of pregnancy. Am J Obstet Gynecol. 2004; 190:1135–1140.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of massive hemorrhage in pregnant women with placenta previa
- Anesthetic management of a parturient with placenta previa totalis undergoing preventive uterine artery embolization before placental expulsion during cesarean delivery: a case report
- Aortic Compression to Control Massive Postpartum Hemorrhage
- Intraoperative bleeding control during cesarean delivery of complete placenta previa with transient occlusion of uterine arteries
- A Case of Placenta Percreta Involving the Urinary Bladder