Healthc Inform Res.
2018 Apr;24(2):118-124. 10.4258/hir.2018.24.2.118.
Evaluation of the IngVaL Pedobarography System for Monitoring of Walking Speed
- Affiliations
-
- 1Embedded Sensor Systems for Health at the School of Innovation, Design and Engineering, Mälardalen University, Västerås, Sweden. per.hellstrom@mdh.se
- 2School of Health, Care and Social Welfare, Mälardalen University, Västerås, Sweden.
- KMID: 2418180
- DOI: http://doi.org/10.4258/hir.2018.24.2.118
Abstract
OBJECTIVES
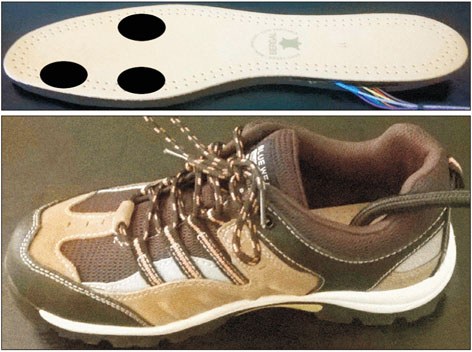
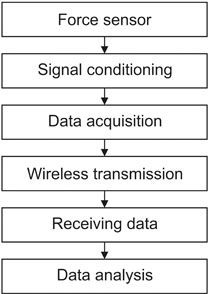
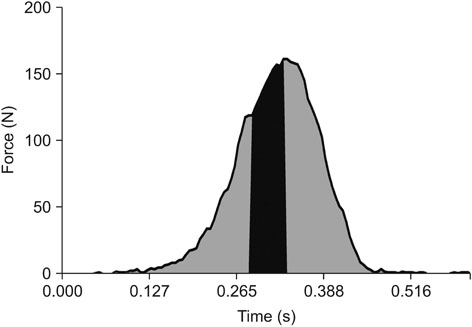
Walking speed is an important component of movement and is a predictor of health in the elderly. Pedobarography, the study of forces acting between the plantar surface of the foot and a supporting surface, is an approach to estimating walking speed even when no global positioning system signal is available. The developed portable system, Identifying Velocity and Load (IngVaL), is a cost effective alternative to commercially available pedobarography systems because it only uses three force sensing resistors. In this study, the IngVaL system was evaluated. The three variables investigated in this study were the sensor durability, the proportion of analyzable steps, and the linearity between the system output and the walking speed.
METHODS
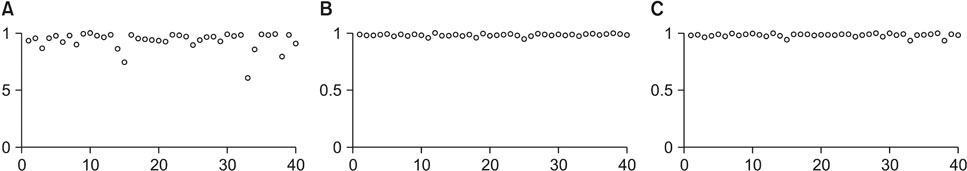
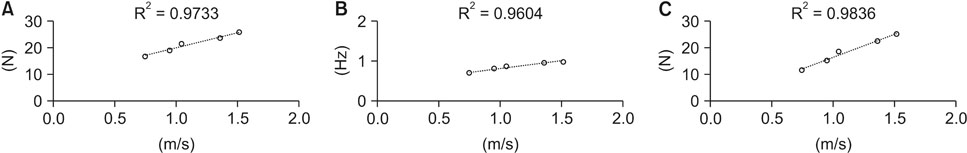
Data was collected from 40 participants, each of whom performed five walks at five different self-paced walking speeds. The linearity between the walking speed and step frequency measured with R2 values was compared for the walking speed obtained "˜A' only using amplitude data from the force sensors, "˜B' that obtained only using the step frequency, and "˜C' that obtained by combining amplitude data for each of the 40 test participants.
RESULTS
Improvement of the wireless data transmission increased the percentage of analyzable steps from 83.1% measured with a prototype to 96.6% for IngVaL. The linearity comparison showed that the methods A, B, and C were accurate for 2, 15, and 23 participants, respectively.
CONCLUSIONS
Increased sensor durability and a higher percentage of analyzed steps indicates that IngVaL is an improvement over the prototype system. The combined strategy of amplitude and step frequency was confirmed as the most accurate method.
Keyword
Figure
Reference
-
1. World Health Organization. Global health and aging. Geneva, Switzerland: World Health Organization;2011.2. Nia AM, Mozaffari-Kermani M, Sur-Kolay S, Raghunathan A, Jha NK. Energy-efficient long-term continuous personal health monitoring. IEEE Trans Multiscale Comput Syst. 2015; 1(2):85–98.
Article3. Mostaghel R. Innovation and technology for the elderly: systematic literature review. J Bus Res. 2016; 69(11):4896–4900.
Article4. World Health Organization. Global recommendations on physical activity for health. Geneva, Switzerland: World Health Organization;2010.5. Tao W, Liu T, Zheng R, Feng H. Gait analysis using wearable sensors. Sensors (Basel). 2012; 12(2):2255–2283.
Article6. Muro-de-la-Herran A, Garcia-Zapirain B, Mendez-Zorrilla A. Gait analysis methods: an overview of wearable and non-wearable systems, highlighting clinical applications. Sensors (Basel). 2014; 14(2):3362–3394.
Article7. Haghi M, Thurow K, Stoll R. Wearable devices in medical Internet of Things: scientific research and commercially available devices. Healthc Inform Res. 2017; 23(1):4–15.
Article8. El-Amrawy F, Nounou MI. Are currently available wearable devices for activity tracking and heart rate monitoring accurate, precise, and medically beneficial? Healthc Inform Res. 2015; 21(4):315–320.
Article9. Miller DJ, Freedson PS, Kline GM. Comparison of activity levels using the Caltrac accelerometer and five questionnaires. Med Sci Sports Exerc. 1994; 26(3):376–382.
Article10. Lee YS, Ho CS, Shih Y, Chang SY, Robert FJ, Shiang TY. Assessment of walking, running, and jumping movement features by using the inertial measurement unit. Gait Posture. 2015; 41(4):877–881.
Article11. Vrijkotte TG, van Doornen LJ, de Geus EJ. Effects of work stress on ambulatory blood pressure, heart rate, and heart rate variability. Hypertension. 2000; 35(4):880–886.
Article12. Bastien GJ, Willems PA, Schepens B, Heglund NC. Effect of load and speed on the energetic cost of human walking. Eur J Appl Physiol. 2005; 94(1-2):76–83.
Article13. Purser JL, Weinberger M, Cohen HJ, Pieper CF, Morey MC, Li T, et al. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005; 42(4):535–546.
Article14. Shinkai S, Watanabe S, Kumagai S, Fujiwara Y, Amano H, Yoshida H, et al. Walking speed as a good predictor for the onset of functional dependence in a Japanese rural community population. Age Ageing. 2000; 29(5):441–446.
Article15. Corbellini S, Ramella C, Fallauto C, Pirola M, Stassi S, Canavese G. Low-cost wearable measurement system for continuous real-time pedobarography. In : Proceedings of the IEEE International Symposium on Medical Measurements and Applications (MeMeA); 2015 May 7–9; Turin, Italy. p. 639–644.16. Zhang T, Lu J, Uswatte G, Taub E, Sazonov ES. Measuring gait symmetry in children with cerebral palsy using the SmartShoe. In : Proceedings of the IEEE Healthcare Innovation Conference (HIC); 2014 Oct 8–10; Seattle, WA. p. 48–51.17. Sazonov ES, Fulk G, Hill J, Schutz Y, Browning R. Monitoring of posture allocations and activities by a shoe-based wearable sensor. IEEE Trans Biomed Eng. 2011; 58(4):983–990.
Article18. Boulton AJ, Franks CI, Betts RP, Duckworth T, Ward JD. Reduction of abnormal foot pressures in diabetic neuropathy using a new polymer insole material. Diabetes Care. 1984; 7(1):42–46.
Article19. Lawrence TL, Schmidt RN. Wireless in-shoe force system [for motor prosthesis]. In : Proceedings of the 19th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 1997 Oct 30–Nov 2; Chicago, IL. p. 2238–2241.20. Konno A, Kato N, Shirata S, Furuta T, Uchiyama M. Development of a light-weight biped humanoid robot. In : Proceedings of the IEEE/RSJ International Conference on Intelligent Robots and Systems (IROS); 2000 Oct 31–Nov 5; Takamatsu, Japan. p. 1565–1570.21. Eils E, Streyl M, Linnenbecker S, Thorwesten L, Volker K, Rosenbaum D. Characteristic plantar pressure distribution patterns during soccer-specific movements. Am J Sports Med. 2004; 32(1):140–145.
Article22. Hellstrom P, Folke M, Ekstrom M. Wearable weight estimation system. Procedia Comput Sci. 2015; 64:146–152.
Article23. Joo SB, Oh SE, Sim T, Kim H, Choi CH, Koo H, et al. Prediction of gait speed from plantar pressure using artificial neural networks. Expert Syst Appl. 2014; 41(16):7398–7405.
Article24. Warren GL, Maher RM, Higbie EJ. Temporal patterns of plantar pressures and lower-leg muscle activity during walking: effect of speed. Gait Posture. 2004; 19(1):91–100.
Article25. Segal A, Rohr E, Orendurff M, Shofer J, O'Brien M, Sangeorzan B. The effect of walking speed on peak plantar pressure. Foot Ankle Int. 2004; 25(12):926–933.
Article26. Pataky TC, Caravaggi P, Savage R, Parker D, Goulermas JY, Sellers WI, et al. New insights into the plantar pressure correlates of walking speed using pedobarographic statistical parametric mapping (pSPM). J Biomech. 2008; 41(9):1987–1994.
Article27. Hellstrom PA, Akerberg A, Ekstrom M, Folke M. Walking intensity estimation with a portable pedobarography system. Stud Health Technol Inform. 2016; 224:27–32.28. Rieke J. Ioiometer-pc [Internet]. San Francisco (CA): GitHub Inc.;2016. cited at 2018 Apr 1. Available from: https://github.com/jrieke/ioiometer-pc.29. Bohannon RW. Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing. 1997; 26(1):15–19.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Asymmetrical Weight Bearing during Straight and Circular Walking in Hemiplegic Patients
- Effect of Slow Walking Speed on Gait
- Comparing Self-Selected Speed Walking of the Elderly With Self-Selected Slow, Moderate, and Fast Speed Walking of Young Adults
- Effects of Backward Walking Training with Task Orientation on the Functional Gait of Children with Spastic Hemiplegia
- Effect of Treadmill Backward Walking Training on Motor Capacity in Cerebral Palsy: A Randomized Controlled Study