Cancer Res Treat.
2018 Jul;50(3):984-991. 10.4143/crt.2017.248.
Effects of Aspirin, Nonsteroidal Anti-inflammatory Drugs, Statin, and COX2 Inhibitor on the Developments of Urological Malignancies: A Population-Based Study with 10-Year Follow-up Data in Korea
- Affiliations
-
- 1Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Urology, Seoul National University Hospital, Seoul, Korea. drboss@gmail.com
- KMID: 2417887
- DOI: http://doi.org/10.4143/crt.2017.248
Abstract
- PURPOSE
The purpose of this study was to determine the impact of aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs), statin, and cyclooxygenase 2 (COX-2) inhibitor on the development of kidney, prostate, and urothelial cancers by analyzing the Korean National Health Insurance Service-National Sample Cohort (NHIS-NSC) database.
MATERIALS AND METHODS
Among a representative sample cohort of 1,025,340 participants in NHIS-NSC database in 2002, we extracted data of 799,850 individuals who visited the hospital more than once, and finally included 321,122 individuals aged 40 and older. Following a 1-year washout period between 2002 and 2003, we analyzed 143,870 (male), 320,861 and 320,613 individuals for evaluating the risk of prostate cancer, kidney cancer and urothelial cancer developments, respectively, during 10-year follow-up periods between 2004 and 2013. The medication group consisted of patients prescribed these drugs more than 60% of the time in 2003. To adjustfor various parameters of the patients, a multivariate Cox regression model was adopted.
RESULTS
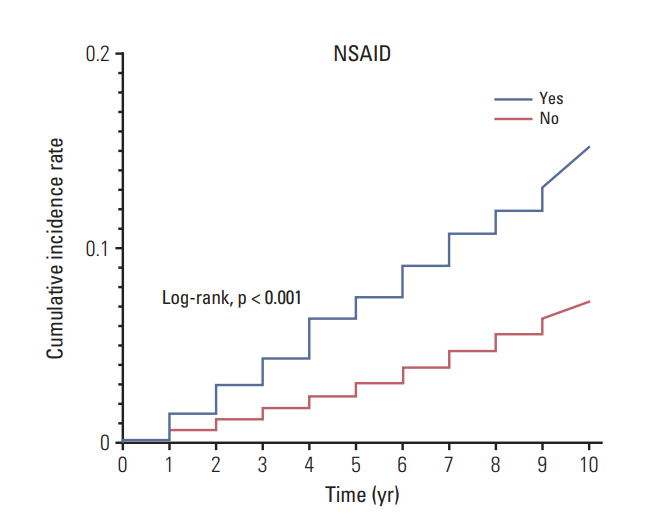
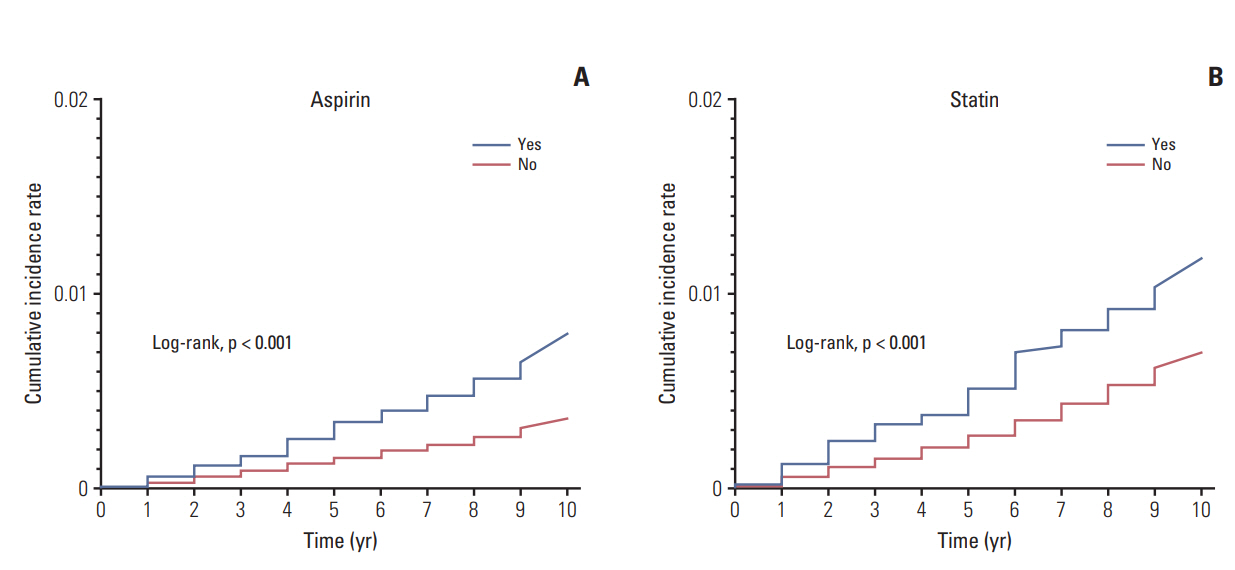
During 10-year follow-up periods between 2004 and 2013, 9,627 (6.7%), 1,107 (0.4%), and 2,121 (0.7%) patients were diagnosed with prostate cancer, kidney cancer, and urothelial cancer, respectively. Notably, multivariate analyses revealed that NSAIDs significantly increased the risk of prostate cancer (hazard ratio [HR], 1.35). Also, it was found that aspirin (HR, 1.28) and statin (HR, 1.55) elevated the risk of kidney cancer. No drugs were associated with the risk of urothelial cancer.
CONCLUSION
In sum, our study provides the valuable information for the impact of aspirin, NSAID, statin, and COX-2 inhibitor on the risk of prostate, kidney, and urothelial cancer development and its survival outcomes.
Keyword
MeSH Terms
-
Anti-Inflammatory Agents
Anti-Inflammatory Agents, Non-Steroidal
Aspirin*
Cohort Studies
Cyclooxygenase 2
Follow-Up Studies*
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors*
Kidney
Kidney Neoplasms
Korea*
Multivariate Analysis
National Health Programs
Prostate
Prostatic Neoplasms
Anti-Inflammatory Agents
Anti-Inflammatory Agents, Non-Steroidal
Aspirin
Cyclooxygenase 2
Figure
Cited by 1 articles
-
Establishment of the Seoul National University Prospectively Enrolled Registry for Genitourinary Cancer (SUPER-GUC): A prospective, multidisciplinary, bio-bank linked cohort and research platform
Chang Wook Jeong, Jungyo Suh, Hyeong Dong Yuk, Bum Sik Tae, Miso Kim, Bhumsuk Keam, Jin Ho Kim, Sang Youn Kim, Jeong Yeon Cho, Seung Hyup Kim, Kyung Chul Moon, Gi Jeong Cheon, Ja Hyeon Ku, Hyeon Hoe Kim, Cheol Kwak
Investig Clin Urol. 2019;60(4):235-243. doi: 10.4111/icu.2019.60.4.235.
Reference
-
References
1. Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002; 287:337–44.2. Iacobone M, Citton M, Viel G, Boetto R, Bonadio I, Mondi I, et al. Adrenalectomy may improve cardiovascular and metabolic impairment and ameliorate quality of life in patients with adrenal incidentalomas and subclinical Cushing's syndrome. Surgery. 2012; 152:991–7.
Article3. Patrignani P, Patrono C. Aspirin and cancer. J Am Coll Cardiol. 2016; 68:967–76.
Article4. Matusewicz L, Meissner J, Toporkiewicz M, Sikorski AF. The effect of statins on cancer cells: review. Tumour Biol. 2015; 36:4889–904.5. Rayburn ER, Ezell SJ, Zhang R. Anti-inflammatory agents for cancer therapy. Mol Cell Pharmacol. 2009; 1:29–43.
Article6. Bosetti C, Rosato V, Gallus S, La Vecchia C. Aspirin and urologic cancer risk: an update. Nat Rev Urol. 2012; 9:102–10.
Article7. Liu Y, Chen JQ, Xie L, Wang J, Li T, He Y, et al. Effect of aspirin and other non-steroidal anti-inflammatory drugs on prostate cancer incidence and mortality: a systematic review and metaanalysis. BMC Med. 2014; 12:55.
Article8. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: The National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46:e15.
Article9. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–83.
Article10. Ishiguro H, Kawahara T. Nonsteroidal anti-inflammatory drugs and prostatic diseases. Biomed Res Int. 2014; 2014:436123.
Article11. Kulp SK, Yang YT, Hung CC, Chen KF, Lai JP, Tseng PH, et al. 3-phosphoinositide-dependent protein kinase-1/Akt signaling represents a major cyclooxygenase-2-independent target for celecoxib in prostate cancer cells. Cancer Res. 2004; 64:1444–51.
Article12. Skriver C, Dehlendorff C, Borre M, Brasso K, Sorensen HT, Hallas J, et al. Low-dose aspirin or other nonsteroidal antiinflammatory drug use and prostate cancer risk: a nationwide study. Cancer Causes Control. 2016; 27:1067–79.
Article13. Veitonmaki T, Murtola TJ, Talala K, Taari K, Tammela T, Auvinen A. Non-steroidal anti-inflammatory drugs and cancer death in the Finnish Prostate Cancer Screening Trial. PLoS One. 2016; 11:e0153413.
Article14. Choueiri TK, Je Y, Cho E. Analgesic use and the risk of kidney cancer: a meta-analysis of epidemiologic studies. Int J Cancer. 2014; 134:384–96.
Article15. Tougeron D, Sha D, Manthravadi S, Sinicrope FA. Aspirin and colorectal cancer: back to the future. Clin Cancer Res. 2014; 20:1087–94.
Article16. Altwairgi AK. Statins are potential anticancerous agents (review). Oncol Rep. 2015; 33:1019–39.
Article17. Fang Z, Tang Y, Fang J, Zhou Z, Xing Z, Guo Z, et al. Simvastatin inhibits renal cancer cell growth and metastasis via AKT/mTOR, ERK and JAK2/STAT3 pathway. PLoS One. 2013; 8:e62823.
Article18. Liu W, Choueiri TK, Cho E. Statin use and the risk of renal cell carcinoma in 2 prospective US cohorts. Cancer. 2012; 118:797–803.
Article19. Zhang XL, Liu M, Qian J, Zheng JH, Zhang XP, Guo CC, et al. Statin use and risk of kidney cancer: a meta-analysis of observational studies and randomized trials. Br J Clin Pharmacol. 2014; 77:458–65.
Article20. Pottegard A, Clark P, Friis S, Hallas J, Lund L. Long-term use of statins and risk of renal cell carcinoma: a population-based case-control study. Eur Urol. 2016; 69:877–82.21. Daugherty SE, Pfeiffer RM, Sigurdson AJ, Hayes RB, Leitzmann M, Schatzkin A, et al. Nonsteroidal antiinflammatory drugs and bladder cancer: a pooled analysis. Am J Epidemiol. 2011; 173:721–30.
Article22. Kuo CC, Chiu HF, Lee IM, Kuo HW, Lee CT, Yang CY. Statin use and the risk of bladder cancer: a population-based casecontrol study. Expert Opin Drug Saf. 2012; 11:733–8.
Article23. Zhang XL, Geng J, Zhang XP, Peng B, Che JP, Yan Y, et al. Statin use and risk of bladder cancer: a meta-analysis. Cancer Causes Control. 2013; 24:769–76.
Article24. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46:799–800.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypersensitivity to Aspirin and Nonsteroidal Anti-inflammatory Drugs
- The Use of COX-2 Selective Nonsteroidal Anti-inflammatory Drugs for the Treatment of Osteoarthritis
- Cost-effectiveness of Non-steroidal Anti-inflammatory Drugs Adjusting for Upper and Lower Gastrointestinal Toxicities in Rheumatoid Arthritis Patients
- Diagnosis and treatment of Helicobacter pylori infection in patients treated with non-steroidal anti-inflammatory drugs
- Statin and aspirin for chemoprevention of hepatocellular carcinoma: Time to use or wait further?