Cancer Res Treat.
2018 Jul;50(3):712-719. 10.4143/crt.2017.100.
Which Patients with Isolated Para-aortic Lymph Node Metastasis Will Truly Benefit from Extended Lymph Node Dissection for Colon Cancer?
- Affiliations
-
- 1Division of Colorectal Surgery, Department of Surgery, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea.
- 2Division of Colorectal Surgery, Department of Surgery, Colorectal Cancer Clinic, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. namkyuk@yuhs.ac
- KMID: 2417860
- DOI: http://doi.org/10.4143/crt.2017.100
Abstract
- PURPOSE
The prognosis of patientswith colon cancer and para-aortic lymph node metastasis (PALNM) is poor. We analyzed the prognostic factors of extramesenteric lymphadenectomy for colon cancer patients with isolated PALNM.
MATERIALS AND METHODS
We retrospectively reviewed 49 patients with PALNM who underwent curative resection between October 1988 and December 2009.
RESULTS
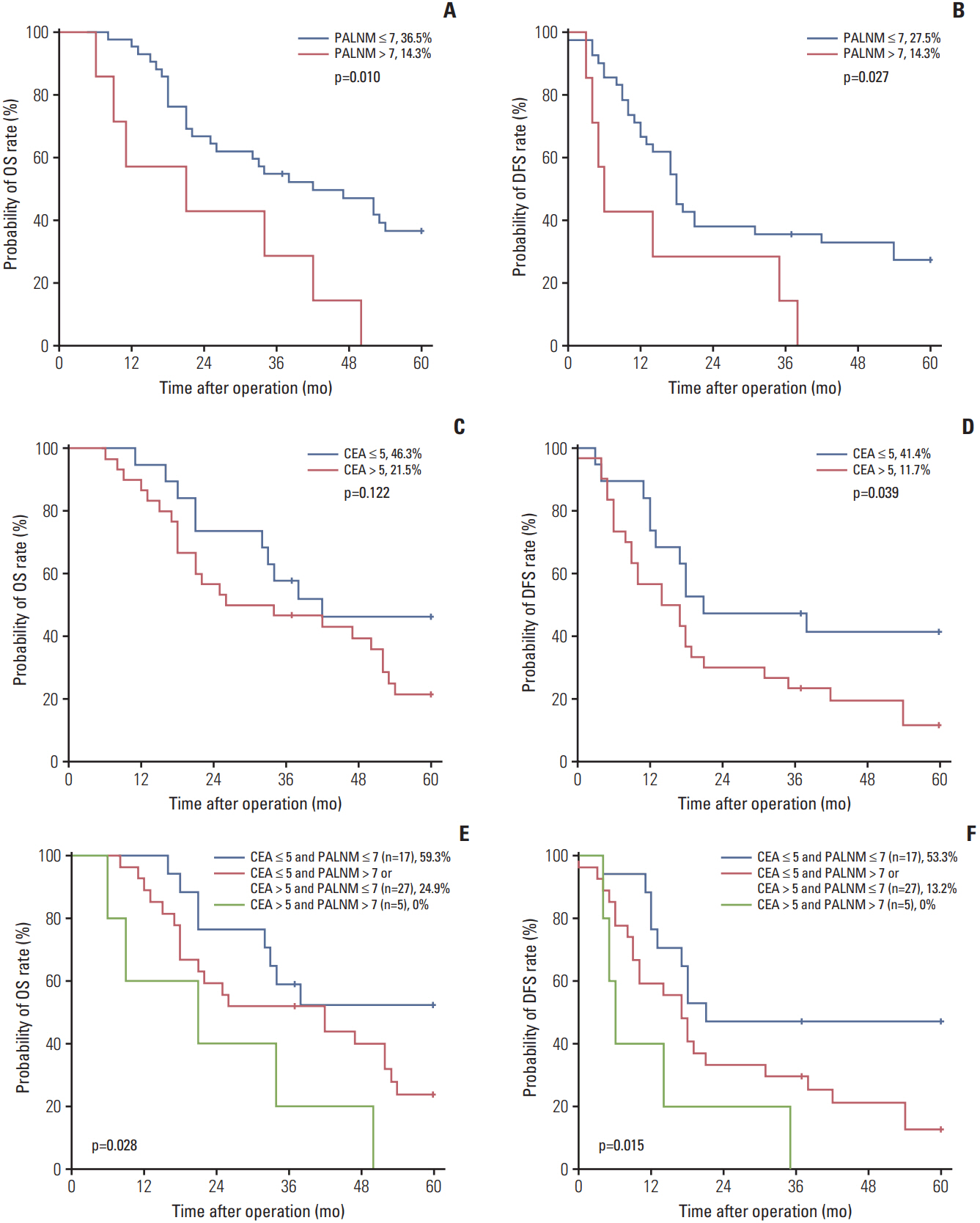
In univariate analyses, the 5-year overall survival (OS) and disease-free survival (DFS) rates were higher in patients with ≤ 7 positive para-aortic lymph node (PALN) (36.5% and 27.5%) than in those with > 7 PALN (14.3% and 14.3%; p=0.010 and p=0.027, respectively), and preoperative carcinoembryonic antigen (CEA) level > 5 was also correlated with a lower 5-year OS and DFS rate of 21.5% and 11.7% compared with those with CEA ≤ 5 (46.3% and 41.4%; p=0.122 and 0.039, respectively). Multivariate analysis found that the number of positive PALN (hazard ratio [HR], 3.291; 95% confidence interval [CI], 1.309 to 8.275; p=0.011) was an independent prognostic factor for OS and the number of positive PALN (HR, 2.484; 95% CI, 0.993 to 6.211; p=0.052) and preoperative CEA level (HR, 1.953; 95% CI, 0.940 to 4.057; p=0.073) were marginally independent prognostic factors for DFS. According to our prognostic model, the 5-year OS and DFS rate increased to 59.3% and 53.3%, respectively, in patients with ≤ 7 positive PALN and CEA level ≤ 5.
CONCLUSION
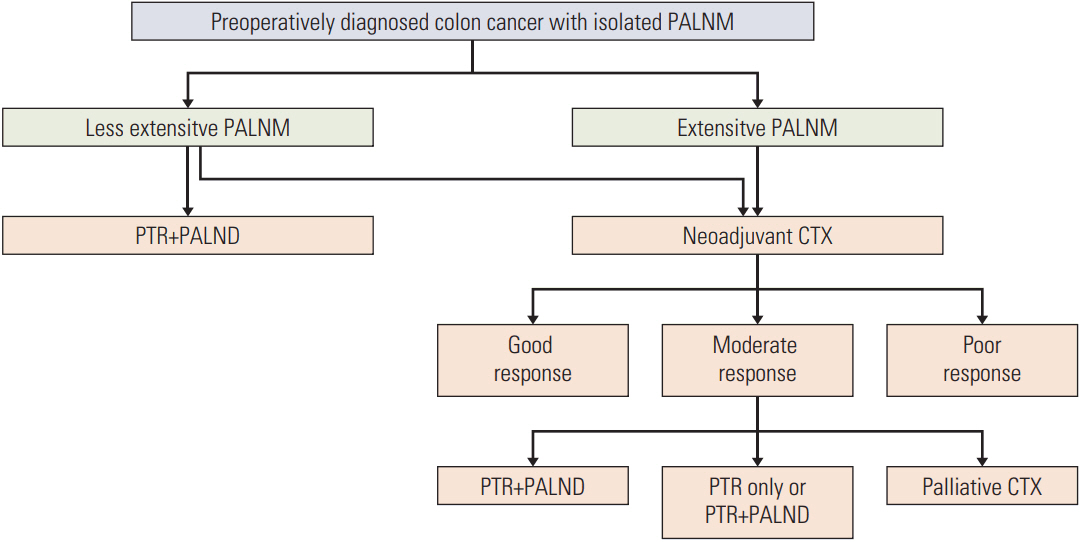
PALN dissection might be beneficial in carefully selected patients with a low CEA level and less extensive PALNM.
MeSH Terms
Figure
Cited by 1 articles
-
Multicenter study of prognostic factors in paraaortic lymph node dissection for metastatic colorectal cancer
Jun Woo Bong, Sanghee Kang, Pyoungjae Park
Ann Surg Treat Res. 2023;105(5):271-280. doi: 10.4174/astr.2023.105.5.271.
Reference
-
References
1. Choi PW, Kim HC, Kim AY, Jung SH, Yu CS, Kim JC. Extensive lymphadenectomy in colorectal cancer with isolated paraaortic lymph node metastasis below the level of renal vessels. J Surg Oncol. 2010; 101:66–71.
Article2. Gagniere J, Dupre A, Chabaud S, Peyrat P, Meeus P, Rivoire M. Retroperitoneal nodal metastases from colorectal cancer: curable metastases with radical retroperitoneal lymphadenectomy in selected patients. Eur J Surg Oncol. 2015; 41:731–7.3. Greene FL. The American Joint Committee on Cancer: updating the strategies in cancer staging. Bull Am Coll Surg. 2002; 87:13–5.4. Bae SU, Han YD, Cho MS, Hur H, Min BS, Baik SH, et al. Oncologic outcomes of colon cancer patients with extraregional lymph node metastasis: comparison of isolated paraaortic lymph node metastasis with resectable liver metastasis. Ann Surg Oncol. 2016; 23:1562–8.
Article5. Khatri VP, Petrelli NJ, Belghiti J. Extending the frontiers of surgical therapy for hepatic colorectal metastases: is there a limit? J Clin Oncol. 2005; 23:8490–9.
Article6. Ogura A, Akiyoshi T, Takatsu Y, Nagata J, Nagasaki T, Konishi T, et al. The significance of extended lymphadenectomy for colorectal cancer with isolated synchronous extraregional lymph node metastasis. Asian J Surg. 2017; 40:254–61.
Article7. Wiggers T, Arends JW, Volovics A. Regression analysis of prognostic factors in colorectal cancer after curative resections. Dis Colon Rectum. 1988; 31:33–41.
Article8. Park IJ, Choi GS, Lim KH, Kang BM, Jun SH. Serum carcinoembryonic antigen monitoring after curative resection for colorectal cancer: clinical significance of the preoperative level. Ann Surg Oncol. 2009; 16:3087–93.
Article9. Thirunavukarasu P, Sukumar S, Sathaiah M, Mahan M, Pragatheeshwar KD, Pingpank JF, et al. C-stage in colon cancer: implications of carcinoembryonic antigen biomarker in staging, prognosis, and management. J Natl Cancer Inst. 2011; 103:689–97.
Article10. Hokuto D, Nomi T, Yamato I, Yasuda S, Obara S, Yoshikawa T, et al. The prognosis of liver resection for patients with four or more colorectal liver metastases has not improved in the era of modern chemotherapy. J Surg Oncol. 2016; 114:959–65.
Article11. Gonzalez M, Poncet A, Combescure C, Robert J, Ris HB, Gervaz P. Risk factors for survival after lung metastasectomy in colorectal cancer patients: a systematic review and metaanalysis. Ann Surg Oncol. 2013; 20:572–9.
Article12. Tepper JE, O'Connell MJ, Niedzwiecki D, Hollis D, Compton C, Benson AB 3rd, et al. Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol. 2001; 19:157–63.
Article13. Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst. 2007; 99:433–41.
Article14. Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003; 21:2912–9.
Article15. Jang KU, Kim CW, Kim KH, Lim SB, Yu CS, Kim TW, et al. Prognostic factors in terms of the number of metastatic nodules in patients with colorectal cancer liver metastases. Ann Coloproctol. 2016; 32:92–100.
Article16. Park SJ, Lee KY, Kim SY. Clinical significance of lymph node micrometastasis in stage I and II colon cancer. Cancer Res Treat. 2008; 40:75–80.
Article17. Nordlinger B, Sorbye H, Glimelius B, Poston GJ, Schlag PM, Rougier P, et al. Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol. 2013; 14:1208–15.
Article18. Albandar MH, Cho MS, Bae SU, Kim NK. Surgical management of extra-regional lymph node metastasis in colorectal cancer. Expert Rev Anticancer Ther. 2016; 16:503–13.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Para-aortic Lymph Node Dissection in Gastric Cancer
- Laparoscopic Para-aortic Lymph Node Dissection in Patients with Gynecologic Malignancy
- Laparoscopic para-aortic lymph node dissection for patients with primary colorectal cancer and clinically suspected para-aortic lymph nodes
- Clinical Implication of Lateral Pelvic Lymph Node Metastasis in Rectal Cancer Treated with Neoadjuvant Chemoradiotherapy
- Prognosis of the Patients Showing Metastasis to the Para-aortic or/and Supraclavicular Lymph Nodes at the Time of Diagnosis of Recurrence of the Cervical Cancer