Cancer Res Treat.
2018 Jul;50(3):681-690. 10.4143/crt.2017.201.
Patient's Cognitive Function and Attitudes towards Family Involvement in Cancer Treatment Decision Making: A Patient-Family Caregiver Dyadic Analysis
- Affiliations
-
- 1Supportive Care Center, Samsung Comprehensive Cancer Center, Seoul, Korea.
- 2Department of Family Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 3Cancer Education Center, Samsung Comprehensive Cancer Center, School of Medicine and SAHIST, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 4Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
- 5Department of Health, Behavior, and Society, Johns Hopkins Bloomberg School of Public Health, Baltimore, MD, USA.
- 6Cancer Policy Branch, National Cancer Center, Goyang, Korea. jonghyock@gmail.com park.keeho@gmail.com
- 7Department of Public Health and Preventive Medicine, Chungbuk National University Hospital, Cheongju, Korea.
- 8College of Medicine/Graduate School of Health Science Business Convergence, Chungbuk National University, Cheongju, Korea.
- 9Department of Hematology-Oncology, Ajou University School of Medicine, Suwon, Korea.
- 10Department of Preventive Medicine, Chonnam National University Medical School, Gwangju, Korea.
- 11Department of Preventive Medicine, Gyeongsang National University School of Medicine, Gyeongsang Institute of Health Science, Jinju, Korea.
- KMID: 2417857
- DOI: http://doi.org/10.4143/crt.2017.201
Abstract
- PURPOSE
Older patient populations commonly have cognitive impairment, which might impact decisional capacity. We examined patients and family caregivers preferences for family involvement in treatment decision making assuming different level of cognitive impairment, and sought to explore the factors associated with the preferences and the degree to which patients and family members agree on preferences.
MATERIALS AND METHODS
A total of 358 elderly cancer patient and caregiver dyads were recruited from the 11 cancer centers in Korea andwere asked to express their preferences forfamily involvement in treatment decision making using hypothetical scenarios with three different levels of cognitive status (intact, mild impairment, and severe impairment).
RESULTS
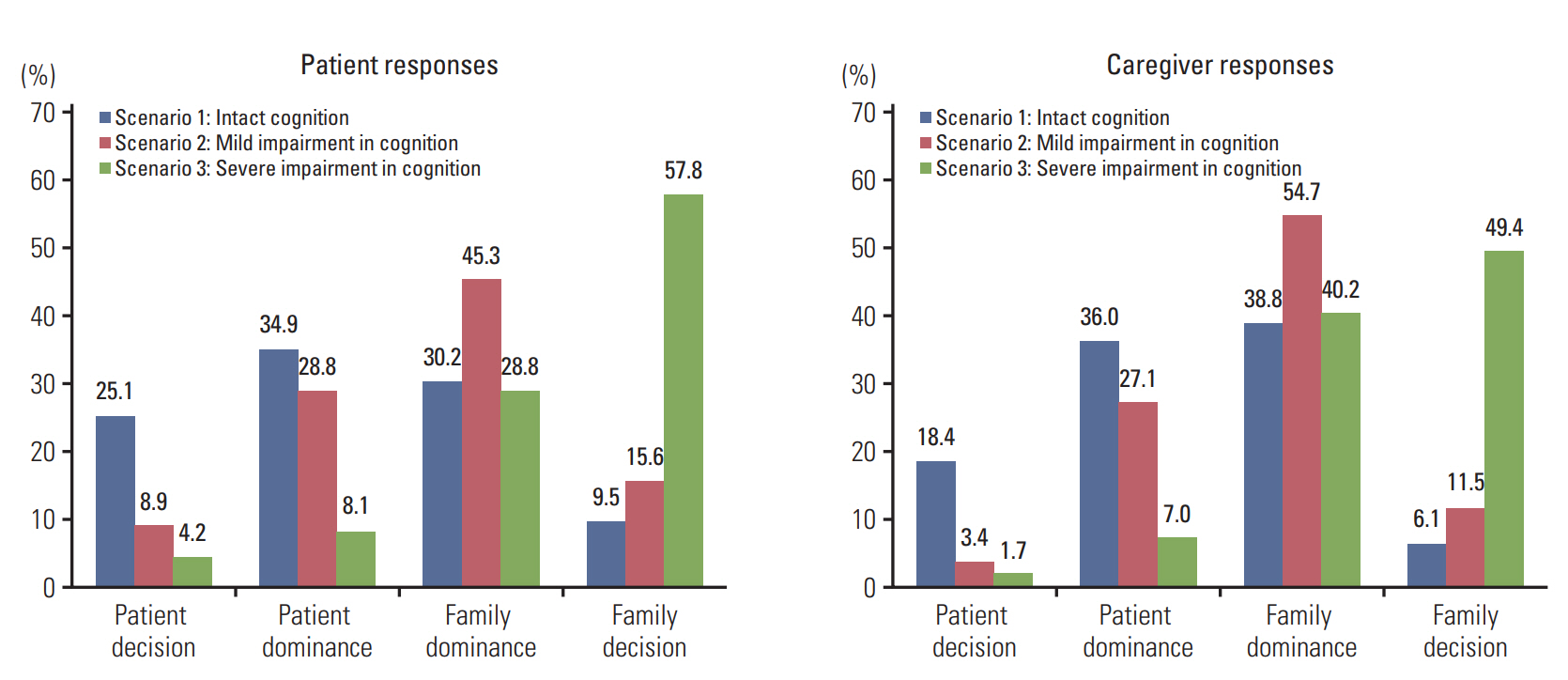
Both patients and family caregivers preferred greater family dominance in treatment decision makingwith the increasing the level of cognitive impairment (39.7%, 60.9%, and 86.6% for patients and 45.0%, 66.2%, and 89.7% for caregivers in each scenarios). Patient and family caregiver concordance in decisional control preference was small for all three scenarios (weighted κ=0.32, κ=0.26, and κ=0.36, respectively). Higher patient education was associated with preference for patient dominance in treatment decision in conditions of both mild and severe cognitive impairment. The association of higher patient education and patient-caregiver preference concordance was positive with intact cognition, while it was negative with severe cognitive impairment.
CONCLUSION
Decision control preferences were affected by hypothesized cognitive status of the patients. Findings from our study would be helpful to develop effective strategy for optimizing family involvement in cancer treatment decision in the context of deteriorating cognitive function of the patients.
MeSH Terms
Figure
Cited by 1 articles
-
What We Talk about When We Talk about Caregiving: The Distribution of Roles in Cancer Patient Caregiving in a Family-Oriented Culture
Ansuk Jeong, Dongwook Shin, Jong Hyock Park, Keeho Park
Cancer Res Treat. 2019;51(1):141-149. doi: 10.4143/crt.2017.557.
Reference
-
References
1. Hamann J, Bronner K, Margull J, Mendel R, Diehl-Schmid J, Buhner M, et al. Patient participation in medical and social decisions in Alzheimer's disease. J Am Geriatr Soc. 2011; 59:2045–52.
Article2. Sharma RK, Hughes MT, Nolan MT, Tudor C, Kub J, Terry PB, et al. Family understanding of seriously-ill patient preferences for family involvement in healthcare decision making. J Gen Intern Med. 2011; 26:881–6.
Article3. Nolan MT, Hughes M, Narendra DP, Sood JR, Terry PB, Astrow AB, et al. When patients lack capacity: the roles that patients with terminal diagnoses would choose for their physicians and loved ones in making medical decisions. J Pain Symptom Manage. 2005; 30:342–53.
Article4. Caillet P, Canoui-Poitrine F, Vouriot J, Berle M, Reinald N, Krypciak S, et al. Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA study. J Clin Oncol. 2011; 29:3636–42.
Article5. Molina-Garrido MJ, Guillen-Ponce C. Development of a cancer- specific comprehensive geriatric assessment in a university hospital in Spain. Crit Rev Oncol Hematol. 2011; 77:148–61.6. Grosshans DR, Meyers CA, Allen PK, Davenport SD, Komaki R. Neurocognitive function in patients with small cell lung cancer: effect of prophylactic cranial irradiation. Cancer. 2008; 112:589–95.7. Schagen SB, Boogerd W, Muller MJ, Huinink WT, Moonen L, Meinhardt W, et al. Cognitive complaints and cognitive impairment following BEP chemotherapy in patients with testicular cancer. Acta Oncol. 2008; 47:63–70.
Article8. Chen X, Zhu C, Li J, Qiu L, Zhang L, Yu F, et al. Dissociation of decision making under ambiguity and decision making under risk in breast cancer patients receiving adjuvant chemotherapy: a neuropsychological study. Brain Res. 2013; 1533:63–72.
Article9. Shin DW, Cho J, Roter DL, Kim SY, Sohn SK, Yoon MS, et al. Preferences for and experiences of family involvement in cancer treatment decision-making: patient-caregiver dyads study. Psychooncology. 2013; 22:2624–31.
Article10. Shin DW, Cho J, Roter DL, Kim SY, Yang HK, Park K, et al. Attitudes toward family involvement in cancer treatment decision making: the perspectives of patients, family caregivers, and their oncologists. Psychooncology. 2017; 26:770–8.
Article11. Degner LF, Sloan JA, Venkatesh P. The Control Preferences Scale. Can J Nurs Res. 1997; 29:21–43.12. Makoul G, Clayman ML. An integrative model of shared decision making in medical encounters. Patient Educ Couns. 2006; 60:301–12.
Article13. Harzing AW, Brown M, Koster K, Zhao S. Response style differences in cross-national research. Manag Int Rev. 2012; 52:341–63.
Article14. Wolfs CA, de Vugt ME, Verkaaik M, Haufe M, Verkade PJ, Verhey FR, et al. Rational decision-making about treatment and care in dementia: a contradiction in terms? Patient Educ Couns. 2012; 87:43–8.
Article15. Hirschman KB, Xie SX, Feudtner C, Karlawish JH. How does an Alzheimer's disease patient's role in medical decision making change over time? J Geriatr Psychiatry Neurol. 2004; 17:55–60.
Article16. Miller LM, Whitlatch CJ, Lyons KS. Shared decision-making in dementia: a review of patient and family carer involvement. Dementia (London). 2016; 15:1141–57.
Article17. Ishikawa H, Roter DL, Yamazaki Y, Hashimoto H, Yano E. Patients' perceptions of visit companions' helpfulness during Japanese geriatric medical visits. Patient Educ Couns. 2006; 61:80–6.
Article18. Hirschman KB, Joyce CM, James BD, Xie SX, Casarett DJ, Karlawish JH. Would caregivers of Alzheimer disease patients involve their relative in a decision to use an AD-slowing medication? Am J Geriatr Psychiatry. 2005; 13:1014–21.
Article19. Karel MJ, Moye J, Bank A, Azar AR. Three methods of assessing values for advance care planning: comparing persons with and without dementia. J Aging Health. 2007; 19:123–51.20. Karlawish JH, Casarett D, Propert KJ, James BD, Clark CM. Relationship between Alzheimer's disease severity and patient participation in decisions about their medical care. J Geriatr Psychiatry Neurol. 2002; 15:68–72.
Article21. Samsi K, Manthorpe J. Everyday decision-making in dementia: findings from a longitudinal interview study of people with dementia and family carers. Int Psychogeriatr. 2013; 25:949–61.
Article22. Feinberg LF, Whitlatch CJ. Are persons with cognitive impairment able to state consistent choices? Gerontologist. 2001; 41:374–82.
Article23. de Boer ME, Droes RM, Jonker C, Eefsting JA, Hertogh CM. Thoughts on the future: the perspectives of elderly people with early-stage Alzheimer's disease and the implications for advance care planning. AJOB Prim Res. 2012; 3:14–22.
Article24. MacQuarrie CR. Experiences in early stage Alzheimer's disease: understanding the paradox of acceptance and denial. Aging Ment Health. 2005; 9:430–41.
Article25. Hirschman KB, Joyce CM, James BD, Xie SX, Karlawish JH. Do Alzheimer's disease patients want to participate in a treatment decision, and would their caregivers let them? Gerontologist. 2005; 45:381–8.
Article26. Grisso T, Appelbaum PS. The MacArthur Treatment Competence Study. III: Abilities of patients to consent to psychiatric and medical treatments. Law Hum Behav. 1995; 19:149–74.
Article27. Hilgeman MM, Allen RS, Snow AL, Durkin DW, DeCoster J, Burgio LD. Preserving Identity and Planning for Advance Care (PIPAC): preliminary outcomes from a patient-centered intervention for individuals with mild dementia. Aging Ment Health. 2014; 18:411–24.
Article28. Murphy J, Oliver T. The use of Talking Mats to support people with dementia and their carers to make decisions together. Health Soc Care Community. 2013; 21:171–80.
Article29. Whitlatch CJ, Judge K, Zarit SH, Femia E. Dyadic intervention for family caregivers and care receivers in early-stage dementia. Gerontologist. 2006; 46:688–94.
Article30. Tariman JD, Berry DL, Cochrane B, Doorenbos A, Schepp K. Preferred and actual participation roles during health care decision making in persons with cancer: a systematic review. Ann Oncol. 2010; 21:1145–51.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dyadic Research of Patients and Their Family Caregivers in the Context of Chronic Illness: Current Status and Challenges
- Dyadic Interventions for Heart Failure Patients and Their Family Caregivers: A Systematic Review
- Factors Influencing Family Functioning in Family Caregivers of Patients with Cancer
- Recognition of Patients, Families, Nurses, and Physicians about Clinical Decision-making and Biomedical Ethics
- A study on the Family Caregiver Burden for Psychiatric Out-Patients