J Korean Med Assoc.
2018 Jul;61(7):383-391. 10.5124/jkma.2018.61.7.383.
Comparative analysis of medical, legal, and ethical considerations for establishing a standard operating protocol for artificial insemination by donor
- Affiliations
-
- 1Korea Institution for Public Sperm Bank, Busan, Korea. ohnsa@naver.com
- KMID: 2416408
- DOI: http://doi.org/10.5124/jkma.2018.61.7.383
Abstract
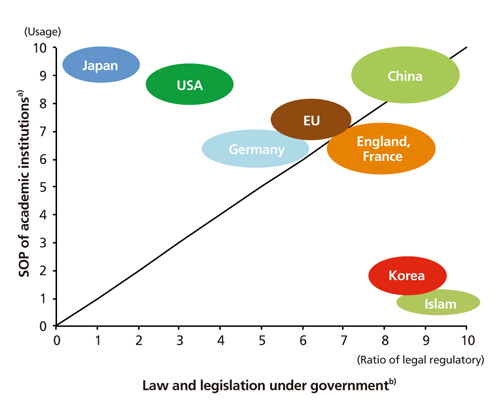
- Artificial insemination by donor is an important means of improving the likelihood of pregnancy in couples affected by male factor infertility, but it poses medical, legal, and ethical issues due to the involvement of third parties, such as the sperm donor. In Korea, the Bioethics and Safety Act was enacted for the purpose of preventing and eliminating unethical research on germ cells, and such research was limited to matters related to the use of assisted reproductive technologies, centering on embryos, oocytes, and protecting the health of oocyte donors. However, this law is incomplete in terms of specific standards or regulations relating to the donation and receipt of sperm. In Korea, artificial insemination by donor has been carried out without a standard operating protocol for donation and receipt of sperm, which would include testing sperm donors for diseases, limiting the number of donor offspring, compensation for donations, and the role of anonymity and non-anonymity. The diversity of policies worldwide shows that each country has its unique set of guidelines tailored for its own specific needs and practical considerations. Herein, I present a standard operating protocol of medical, legal, and ethical principles for artificial insemination by donor that is suitable for domestic circumstances, along with a comparison of recommendations and guidelines of other countries concerning sperm donation issues.
Keyword
MeSH Terms
Figure
Reference
-
1. Park NC. The current status of public sperm bank in Korea. J Korean Med Assoc. 2016; 59:194–204.
Article2. Moon H, Park SY, Kim MH. Online monitoring about illegal Surrogacy arrangement on a commercial basis in Korea. Korean J Med Ethics. 2016; 19:36–46.
Article3. Kim IH, Kim JH, Park MJ, Kang SM, Cho YS, Kim TY, Park NC. Inquiry survey of infertile couples for sperm donation and artificial insemination by donor. Korean J Health Promot. 2017; 17:242–251.
Article4. Park HJ, Park NC. An attitude survey of male infertile patients with artificial insemination by donor. Korean J Fertil Steril. 2003; 30:281–291.5. Kim SC. The legal standing of children born under AID. Law Rev. 2011; 41:85–108.6. Jung KW. Comments on the bioethics and biosafety Act-NT and stem cell research. Korean Soc Fam Law. 2005; 19:7–33.7. Kim E. Legislative issues related to assisted reproductive technology: focusing on the public regulation, the supporting system and the supervisory authority. Korean J Med Law. 2014; 22:43–76.
Article8. Gong D, Liu YL, Zheng Z, Tian YF, Li Z. An overview on ethical issues about sperm donation. Asian J Androl. 2009; 11:645–652.
Article9. Practice Committee of the American Society for Reproductive Medicine. Practice Committee of the Society for Assisted Reproductive Technology. 2006 Guidelines for gamete and embryo donation. Fertil Steril. 2006; 86:5 Suppl 1. S38–S50.10. American Society for Reproductive Medicine. Guidelines for sperm donation. Fertil Steril. 2004; 82:Suppl 1. S9–S12.11. Isley L, Falk RE, Shamonki J, Sims CA, Callum P. Management of the risks for inherited disease in donor-conceived offspring. Fertil Steril. 2016; 106:1479–1484.
Article12. Barratt C, Englert Y, Gottlieb C, Jouannet P. Gamete donation guidelines: the Corsendonk consensus document for the European Union. Hum Reprod. 1998; 13:500–501.
Article13. Kim JK. Suggestions on limiting the number of donor offsprings and sperm donor compensation for male infertility treatment [Internet]. Seoul: Korea National Institute for Bio-thics Policy;2013. cited 2018 Jun 26. Available from: http://nibp.kr/news/2013_01/3.pdf.14. De Melo-Martin I. The ethics of anonymous gamete donation: is there a right to know one’s genetic origins? Hastings Cent Rep. 2014; 44:28–35.15. Lee HA. Ethical review of sperm donations and recipients [Internet]. Seoul: Korea National Institute for Biothics Policy;2015. cited 2018 Jun 26. Available from: http://nibp.kr/news/2015_04/3.pdf.16. Golombok S. New families, old values: considerations regarding the welfare of the child. Hum Reprod. 1998; 13:2342–2347.
Article17. Korea Institute for Public Sperm Bank. Research report for systemic management of the sperm donation, receipt and storage. Sejong: Ministry of Health and Welfare;2016.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inquiry Survey of Infertile Couples for Sperm Donation and Artificial Insemination by Donor
- Reasons of shortage for donated sperm and plan to resolve deficiencies in the sperm donor system
- The current status of public sperm bank in Korea
- An attitude survey of male infertile patients with artificial insemination by donor
- A Case of Retrograde Ejaculation : Sucessful Artificial Insemination Husband