Investig Magn Reson Imaging.
2018 Jun;22(2):86-93. 10.13104/imri.2018.22.2.86.
Comparison of Contrast-Enhanced T2 FLAIR and 3D T1 Black-Blood Fast Spin-Echo for Detection of Leptomeningeal Metastases
- Affiliations
-
- 1Department of Radiology, Ewha Womans University College of Medicine, Seoul, Korea. aahng77@yuhs.ac
- 2Department of Radiology, Yonsei University, College of Medicine, Seoul, Korea.
- KMID: 2415886
- DOI: http://doi.org/10.13104/imri.2018.22.2.86
Abstract
- PURPOSE
Imaging plays a significant role in diagnosing leptomeningeal metastases. However, the most appropriate sequence for the detection of leptomeningeal metastases has yet to be determined. This study compares the efficacies of contrast-enhanced T2 fluid attenuated inversion recovery (FLAIR) and contrast-enhanced 3D T1 black-blood fast spin echo (FSE) imaging for the detection of leptomeningeal metastases.
MATERIALS AND METHODS
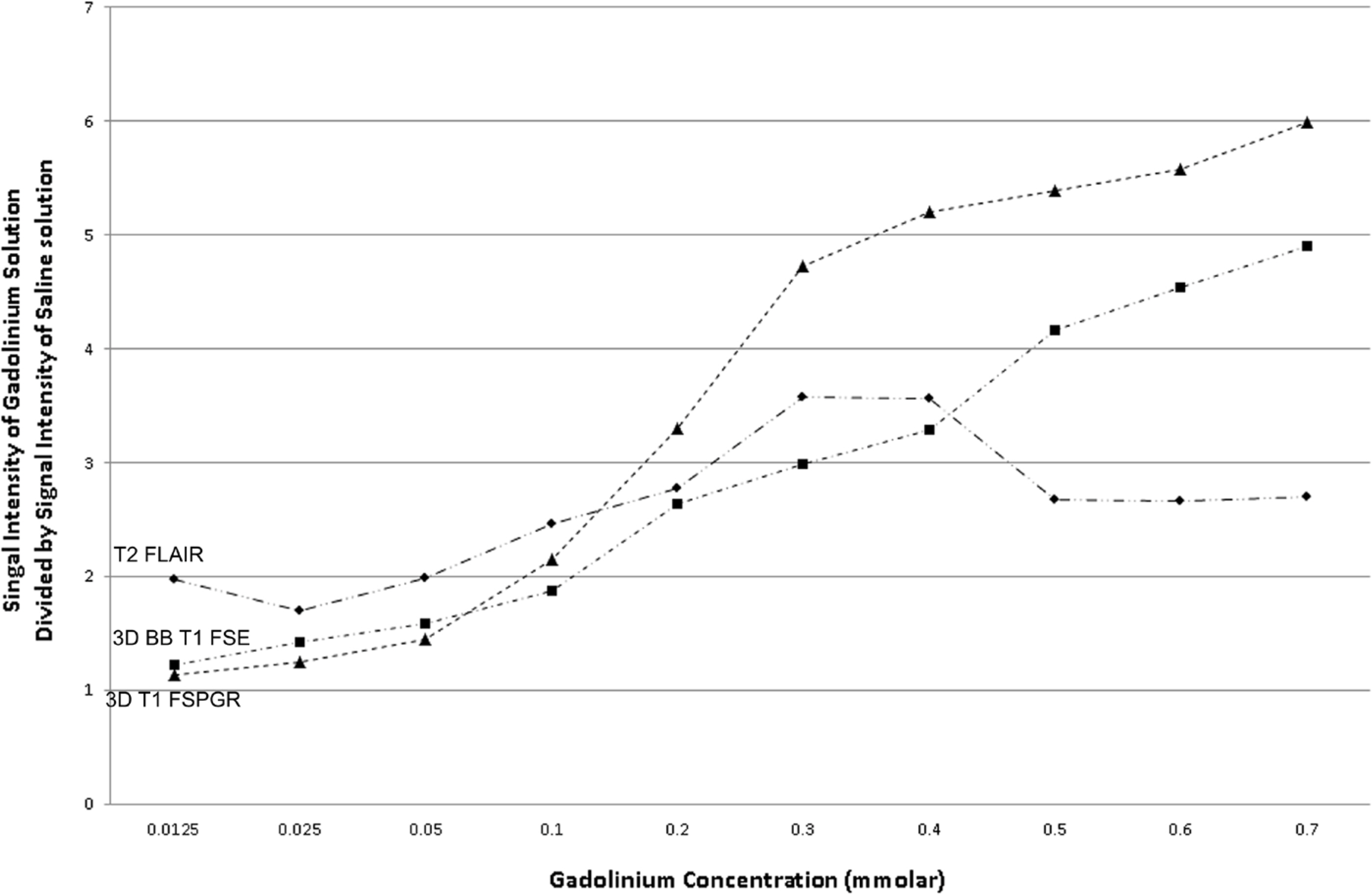
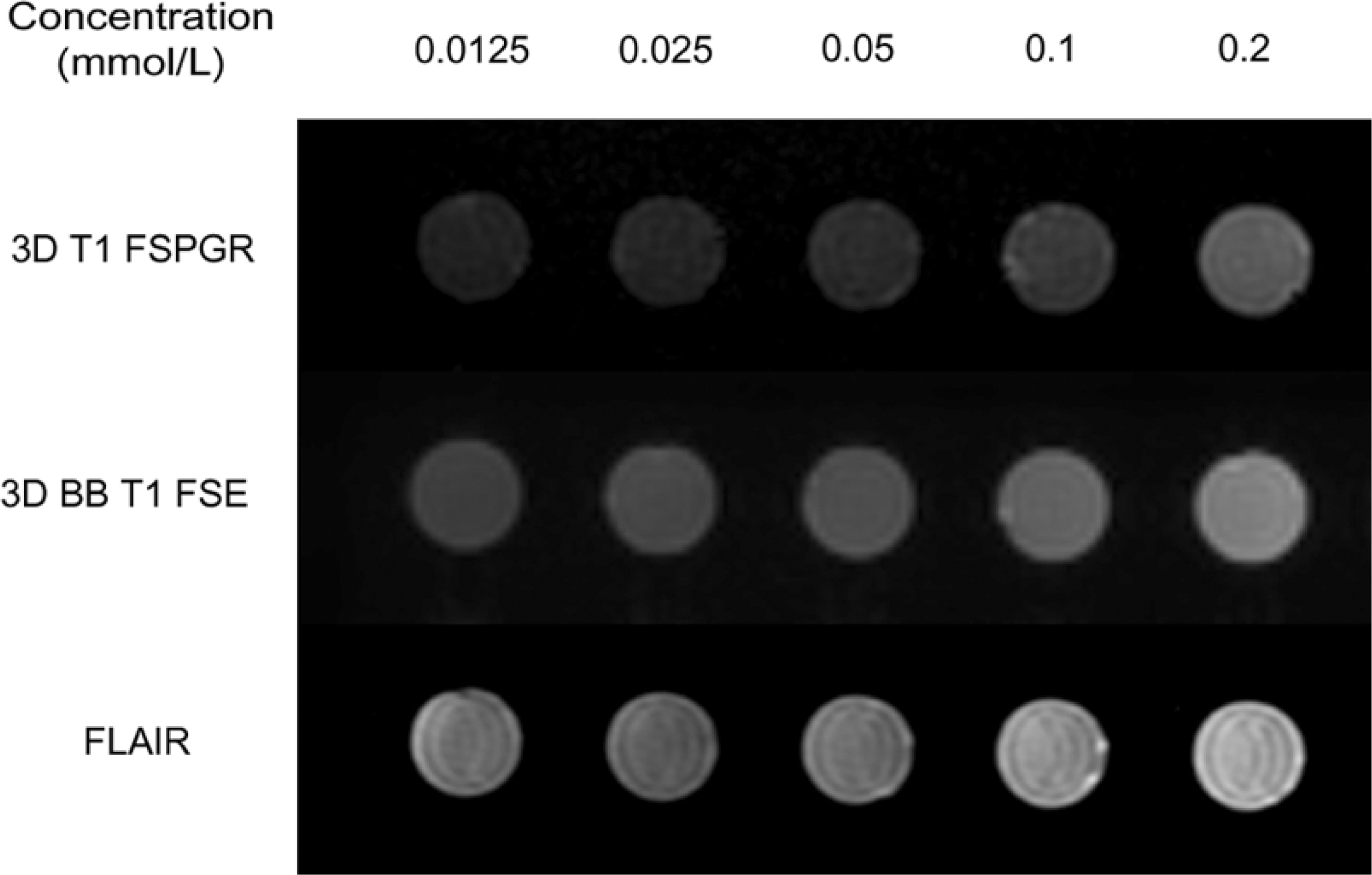
Tube phantoms containing varying concentrations of gadobutrol solution were scanned using T2 FLAIR and 3D T1 black-blood FSE. Additionally, 30 patients with leptomeningeal metastases were retrospectively evaluated to compare conspicuous lesions and the extent of leptomeningeal metastases detected by T2 FLAIR and 3D T1 black-blood FSE.
RESULTS
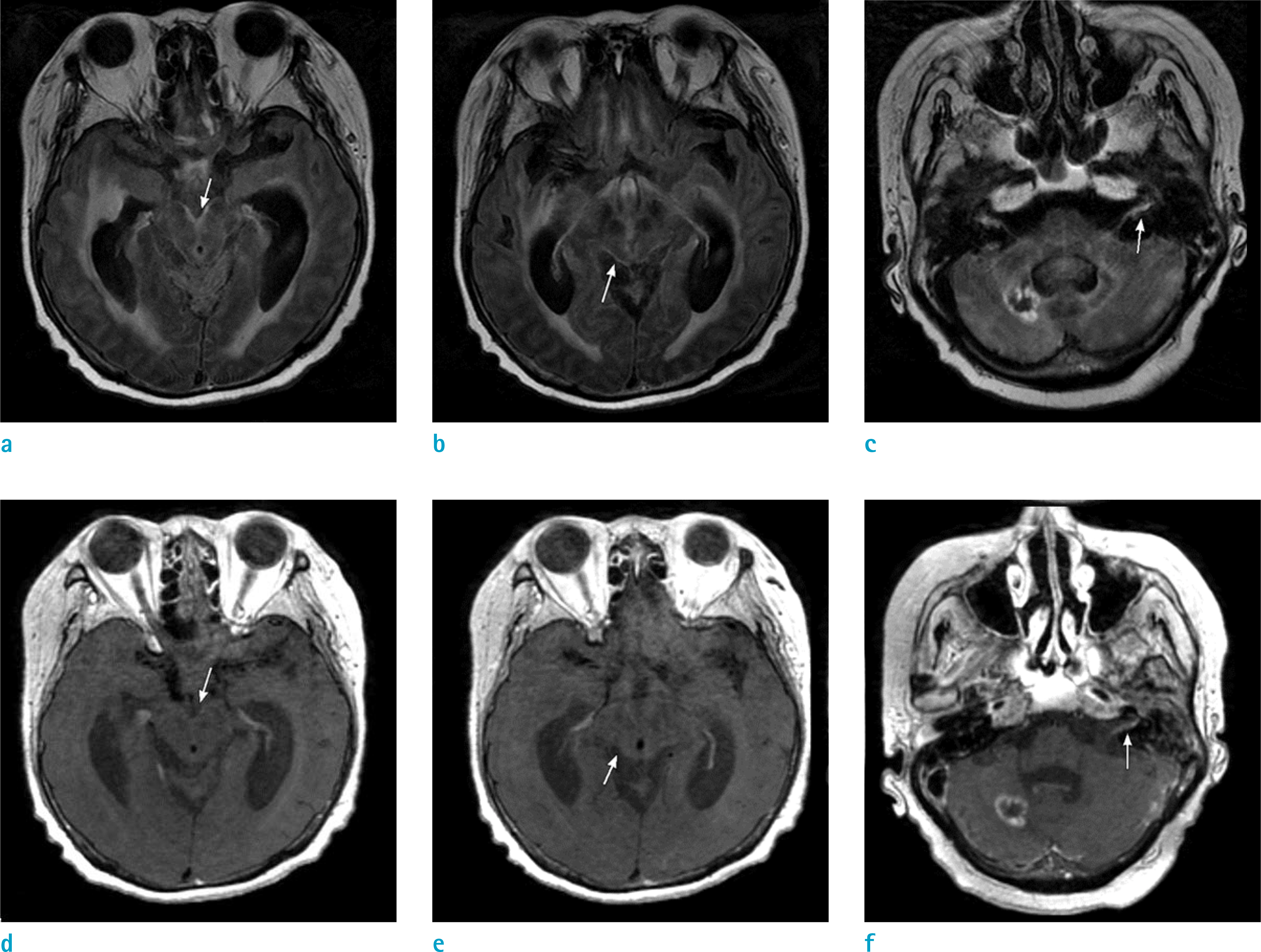
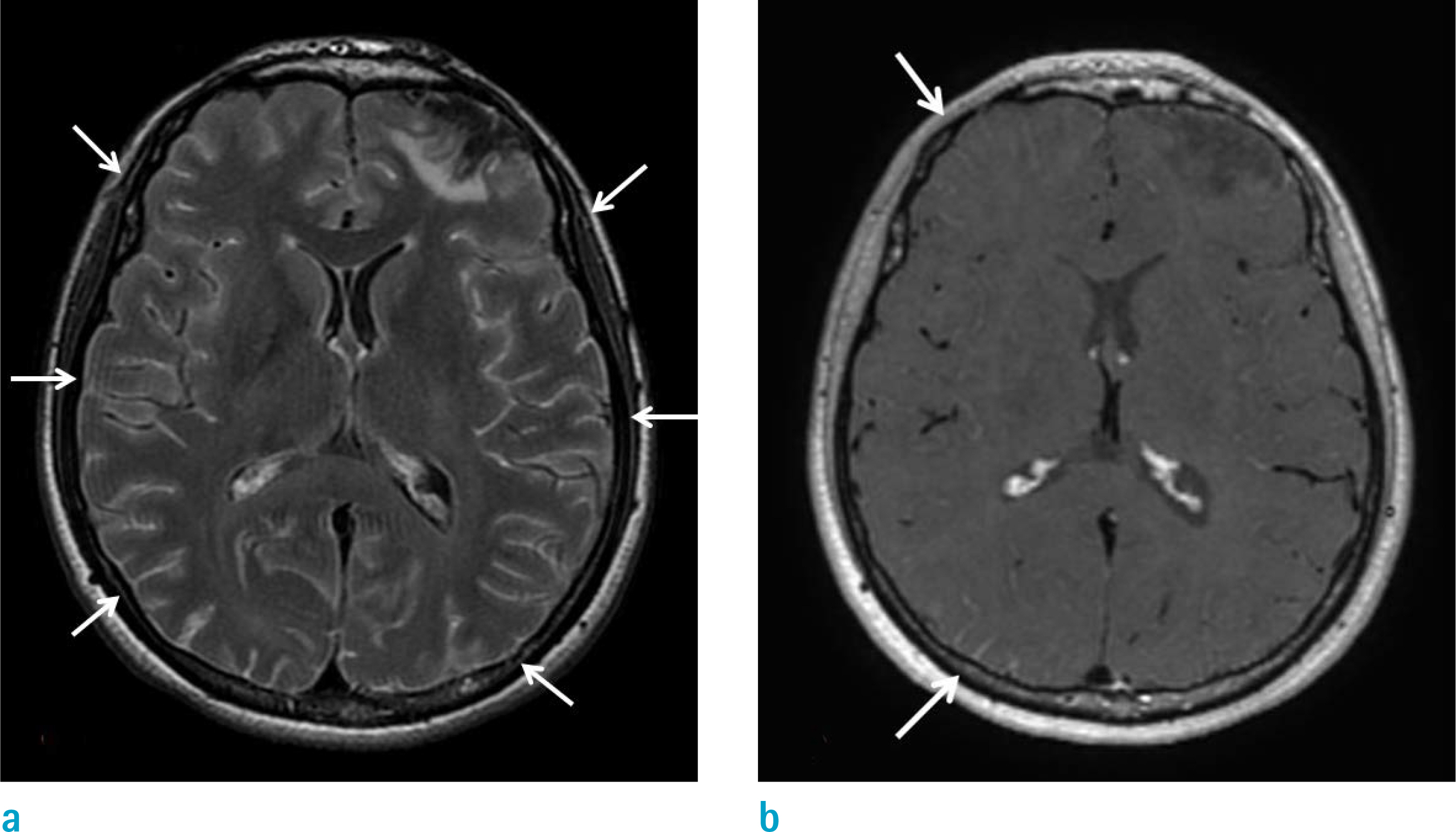
The signal intensities of low-concentration gadobutrol solutions (< 0.5 mmol/L) on T2 FLAIR images were higher than in 3D T1 black-blood FSE. The T2 FLAIR sequences exhibited significantly greater visual conspicuity scores than the 3D T1 black-blood sequence in leptomeningeal metastases of the pial membrane of cistern (P = 0.014). T2 FLAIR images exhibited a greater or equal extent (96.7%) of leptomeningeal metastases than 3D T1 black-blood FSE images.
CONCLUSION
Because of its high sensitivity even at low gadolinium concentrations, contrast-enhanced T2 FLAIR images delineated leptomeningeal metastases in a wider territory than 3D T1 black-blood FSE.
Figure
Reference
-
References
1. Grossman SA, Krabak MJ. Leptomeningeal carcinomatosis. Cancer Treat Rev. 1999; 25:103–119.
Article2. Wasserstrom WR, Glass JP, Posner JB. Diagnosis and treatment of leptomeningeal metastases from solid tumors: experience with 90 patients. Cancer. 1982; 49:759–772.
Article3. Kremer S, Abu Eid M, Bierry G, et al. Accuracy of delayed postcontrast FLAIR MR imaging for the diagnosis of leptomeningeal infectious or tumoral diseases. J Neuroradiol. 2006; 33:285–291.
Article4. Misaki K, Nakada M, Hayashi Y, et al. Contrast-enhanced fluid-attenuated inversion recovery MRI is useful to detect the CSF dissemination of glioblastoma. J Comput Assist Tomogr. 2001; 25:953–956.
Article5. Mathews VP, Caldemeyer KS, Lowe MJ, Greenspan SL, Weber DM, Ulmer JL. Brain: gadolinium-enhanced fast fluid-attenuated inversion-recovery MR imaging. Radiology. 1999; 211:257–263.
Article6. Terae S, Yoshida D, Kudo K, Tha KK, Fujino M, Miyasaka K. Contrast-enhanced FLAIR imaging in combination with pre- and postcontrast magnetization transfer T1-weighted imaging: usefulness in the evaluation of brain metastases. J Magn Reson Imaging. 2007; 25:479–487.
Article7. Fukuoka H, Hirai T, Okuda T, et al. Comparison of the added value of contrast-enhanced 3D fluid-attenuated inversion recovery and magnetization-prepared rapid acquisition of gradient echo sequences in relation to conventional postcontrast T1-weighted images for the evaluation of leptomeningeal diseases at 3T. AJNR Am J Neuroradiol. 2010; 31:868–873.
Article8. Tomura N, Narita K, Takahashi S, et al. Contrast-enhanced multi-shot echoplanar FLAIR in the depiction of metastatic tumors of the brain: comparison with contrast-enhanced spin-echo T1-weighted imaging. Acta Radiol. 2007; 48:1032–1037.
Article9. Jackson EF, Hayman LA. Meningeal enhancement on fast FLAIR images. Radiology. 2000; 215:922–924.
Article10. Park J, Kim J, Yoo E, Lee H, Chang JH, Kim EY. Detection of small metastatic brain tumors: comparison of 3D contrast-enhanced whole-brain black-blood imaging and MP-RAGE imaging. Invest Radiol. 2012; 47:136–141.11. Kammer NN, Coppenrath E, Treitl KM, Kooijman H, Dietrich O, Saam T. Comparison of contrast-enhanced modified T1-weighted 3D TSE black-blood and 3D MP-RAGE sequences for the detection of cerebral metastases and brain tumours. Eur Radiol. 2016; 26:1818–1825.
Article12. Park J, Kim EY. Contrast-enhanced, three-dimensional, whole-brain, black-blood imaging: application to small brain metastases. Magn Reson Med. 2010; 63:553–561.
Article13. Korosec FR, Grist TM, Polzin JA, Weber DM, Mistretta CA. MR angiography using velocity-selective preparation pulses and segmented gradient-echo acquisition. Magn Reson Med. 1993; 30:704–714.
Article14. Norris DG, Schwarzbauer C. Velocity selective radiofrequency pulse trains. J Magn Reson. 1999; 137:231–236.
Article15. Nagao E, Yoshiura T, Hiwatashi A, et al. 3D turbo spin-echo sequence with motion-sensitized driven-equilibrium preparation for detection of brain metastases on 3T MR imaging. AJNR Am J Neuroradiol. 2011; 32:664–670.
Article16. Busse RF, Brau AC, Vu A, et al. Effects of refocusing flip angle modulation and view ordering in 3D fast spin echo. Magn Reson Med. 2008; 60:640–649.
Article17. Takemoto K, Takano K, Abe H, et al. The new MRI modalities "BPAS and VISTA" for the diagnosis of VA dissection. Acta Neurochir Suppl. 2011; 112:59–65.
Article18. Kato Y, Higano S, Tamura H, et al. Usefulness of contrast-enhanced T1-weighted sampling perfection with application-optimized contrasts by using different flip angle evolutions in detection of small brain metastasis at 3T MR imaging: comparison with magnetization-prepared rapid acquisition of gradient echo imaging. AJNR Am J Neuroradiol. 2009; 30:923–929.
Article19. Collie DA, Brush JP, Lammie GA, et al. Imaging features of leptomeningeal metastases. Clin Radiol. 1999; 54:765–771.
Article20. Freilich RJ, Krol G, DeAngelis LM. Neuroimaging and cerebrospinal fluid cytology in the diagnosis of leptomeningeal metastasis. Ann Neurol. 1995; 38:51–57.
Article21. Straathof CS, de Bruin HG, Dippel DW, Vecht CJ. The diagnostic accuracy of magnetic resonance imaging and cerebrospinal fluid cytology in leptomeningeal metastasis. J Neurol. 1999; 246:810–814.
Article22. Ahn SJ, Suh SH, Lee KY, Kim JH, Seo KD, Lee S. Hyperintense vessels on T2-PROPELLER-FLAIR in patients with acute MCA stroke: prediction of arterial stenosis and perfusion abnormality. AJNR Am J Neuroradiol. 2015; 36:2042–2047.
Article23. Ahn SJ, Lee KY, Ahn SS, Suh H, Kim BS, Lee SK. Can FLAIR hyperintense vessel (FHV) signs be influenced by varying MR parameters and flow velocities? A flow phantom analysis. Acta Radiol. 2016; 57:580–586.
Article24. Ahn SJ, Chung TS, Chang JH, Lee SK. The added value of double dose gadolinium enhanced 3D T2 fluid-attenuated inversion recovery for evaluating small brain metastases. Yonsei Med J. 2014; 55:1231–1237.
Article25. Jeong HK, Oh SW, Kim J, Lee SK, Ahn SJ. Reduction of oxygen-induced CSF hyperintensity on FLAIR MR images in sedated children: usefulness of magnetization-prepared FLAIR imaging. AJNR Am J Neuroradiol. 2016; 37:1549–1555.
Article26. Siegal T, Sandbank U, Gabizon A, et al. Alteration of blood-brain-CSF barrier in experimental meningeal carcinomatosis. A morphologic and adriamycin-penetration study. J Neurooncol. 1987; 4:233–242.27. Ludemann L, Grieger W, Wurm R, Wust P, Zimmer C. Quantitative measurement of leakage volume and permeability in gliomas, meningiomas and brain metastases with dynamic contrast-enhanced MRI. Magn Reson Imaging. 2005; 23:833–841.28. Pintaske J, Martirosian P, Graf H, et al. Relaxivity of Gadopentetate Dimeglumine (Magnevist), Gadobutrol (Gadovist), and Gadobenate Dimeglumine (MultiHance) in human blood plasma at 0.2, 1.5, and 3 Tesla. Invest Radiol. 2006; 41:213–221.
Article29. van der Molen AJ, Bellin MF. Extracellular gadolinium-based contrast media: differences in diagnostic efficacy. Eur J Radiol. 2008; 66:168–174.
Article30. Ruff RL, Dougherty JH Jr. Complications of lumbar puncture followed by anticoagulation. Stroke. 1981; 12:879–881.
Article31. Clarke JL, Perez HR, Jacks LM, Panageas KS, Deangelis LM. Leptomeningeal metastases in the MRI era. Neurology. 2010; 74:1449–1454.
Article32. Glass JP, Melamed M, Chernik NL, Posner JB. Malignant cells in cerebrospinal fluid (CSF): the meaning of a positive CSF cytology. Neurology. 1979; 29:1369–1375.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Contrast-enhanced Fast Fluid-attenuated Inversion Recovery MR Imaging in Patients with Brain Tumors
- The Added Value of Double Dose Gadolinium Enhanced 3D T2 Fluid-Attenuated Inversion Recovery for Evaluating Small Brain Metastases
- T1-, T2-weighted, and FLAIR Imaging: Clinical Application
- Single-Slab 3D Fast Spin Echo Imaging: T1 -Contrast Perspective
- Benefit of Using Early ContrastEnhanced 2D T2-Weighted Fluid-Attenuated Inversion Recovery Image to Detect Leptomeningeal Metastasis in Lung-Cancer Staging