J Korean Acad Community Health Nurs.
2018 Jun;29(2):170-183. 10.12799/jkachn.2018.29.2.170.
Interventions Using Technologies for Older Adults in Long-term Care Facilities: A Systematic Review
- Affiliations
-
- 1College of Nursing, Seoul National University, Seoul, Korea.
- 2Centers for Disease Control & Prevention, Cheongju, Korea.
- 3Research Institute of Nursing Science, Seoul National University, Seoul, Korea. yoon26@snu.ac.kr
- KMID: 2415575
- DOI: http://doi.org/10.12799/jkachn.2018.29.2.170
Abstract
- PURPOSE
Although innovative interventions using technologies have been introduced in long-term care settings, available evidence is still anecdotal. The purpose of this study is to investigate and synthesize the outcomes of interventions using technologies delivered to nursing home residents.
METHODS
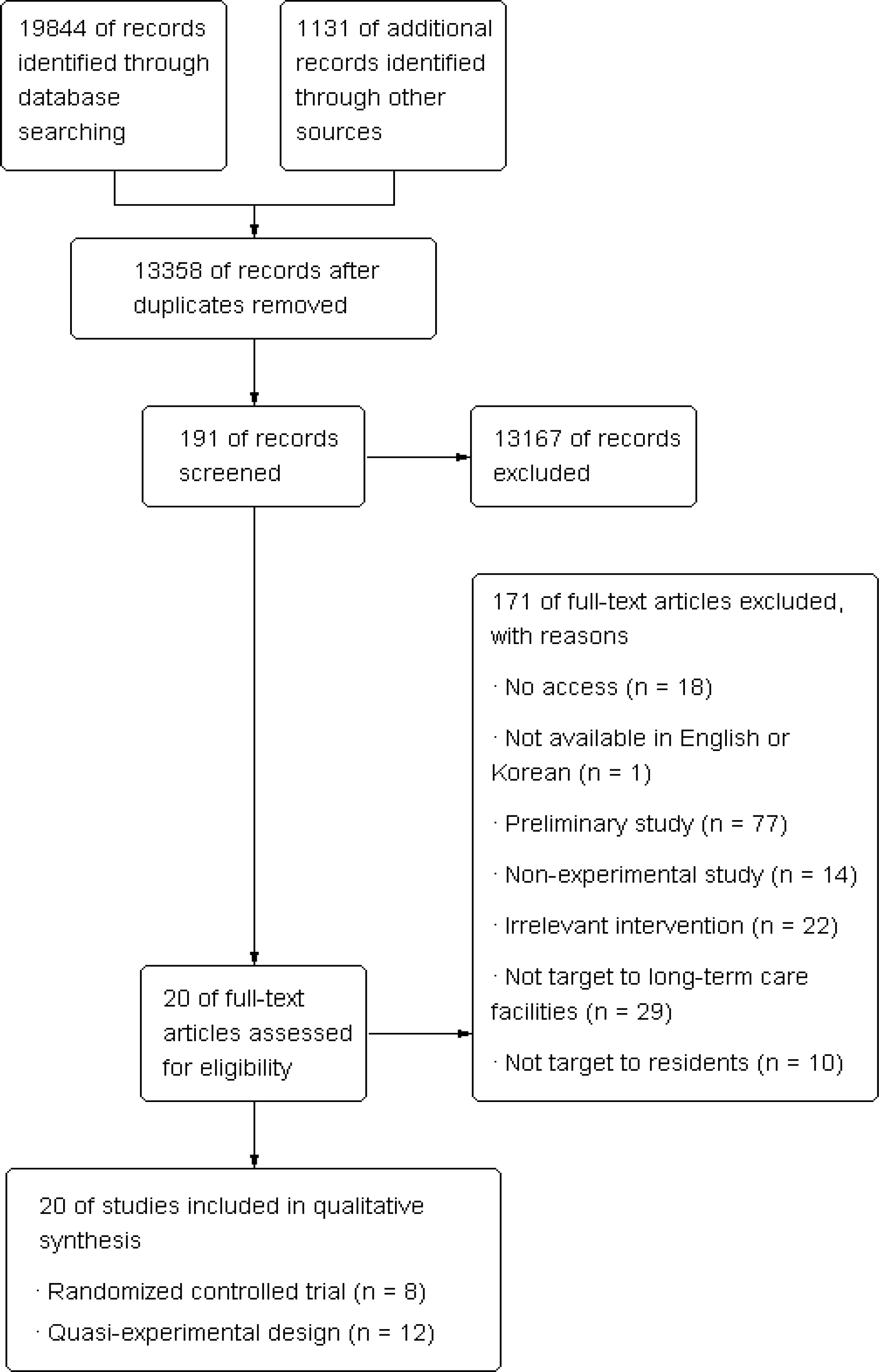
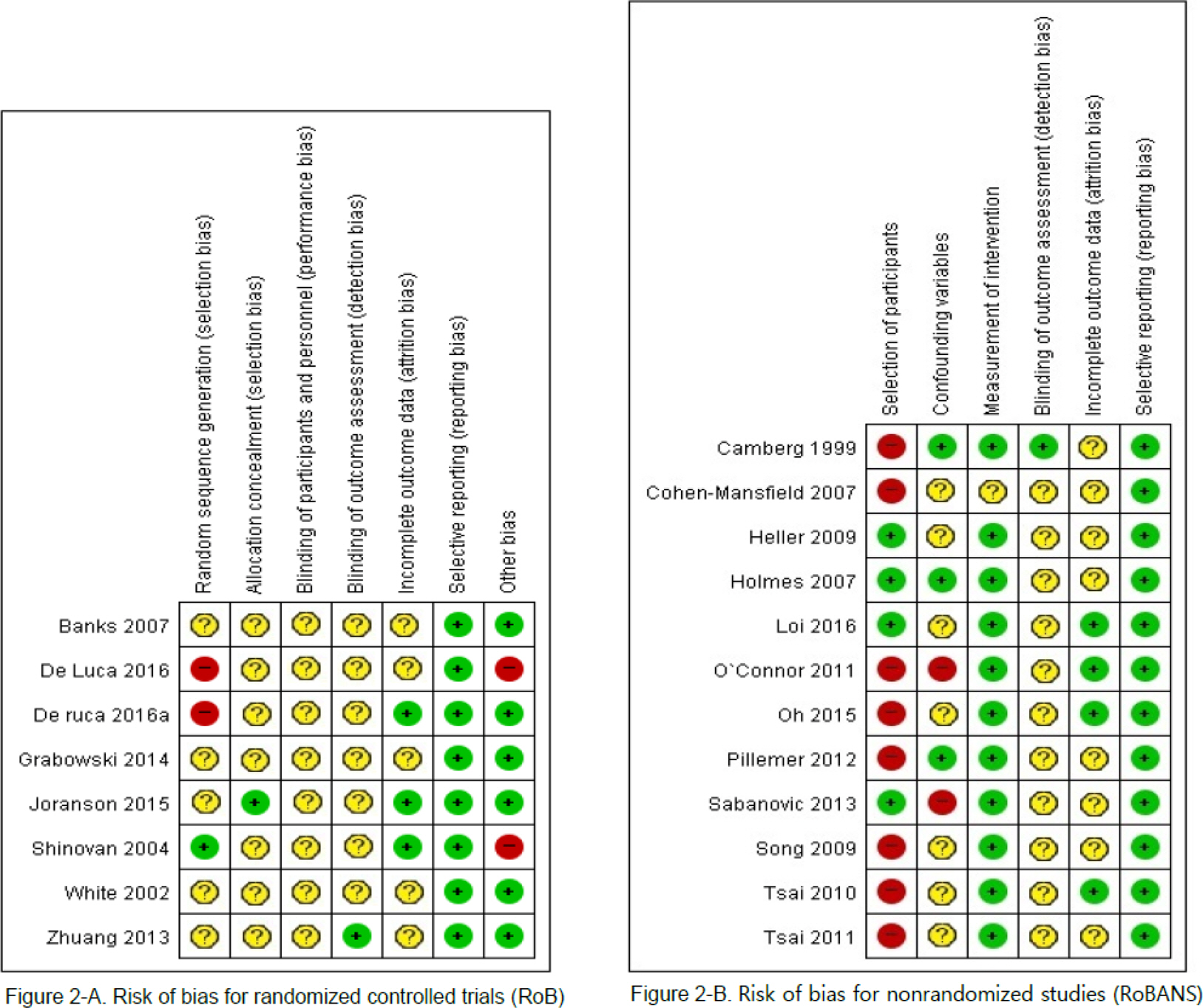
Published clinical trials were identified through PubMed, CINHAL, Cochrane and PsycINFO databases and manually hand-searching. Eligible studies were articles published between 1997-2016 in English or Korean with a randomized controlled trial or quasi-experimental design in which interventions using technologies were delivered to nursing home residents.
RESULTS
A total of 20 studies were selected for this review. Types of interventions using technologies were classified into the electronic documentation technology (n=1), the clinical decision support system (n=1), the safety technology (n=1), the health and wellness technology (n=10), and the social connectedness technology (n=7). Overall resident outcomes indicated that interventions using technologies improved behavioral symptoms and psycho-social outcomes, but mixed results were shown in the aspects of physical function, cognitive function, social relationship and quality of service.
CONCLUSION
This review demonstrates that incorporating technologies into nursing home care have positive effects on residents' psycho-social outcomes and behavioral symptoms. To disseminate the effectiveness of interventions using technologies, further research is needed to determine what mechanisms underlying such relationships exist.
Keyword
MeSH Terms
Figure
Reference
-
References
1. OECD and European Union. A good life in old age? Monitoring and improving quality in long-term care, OECD health policy studies. Paris: OECD Publishing;2013. p. 268. https://doi.org/10.1787/9789264194564-en.2. Czaja SJ. Long-term care services and support systems for older adults: The role of technology. The American Psychologist. 2016; 71(4):294–301. https://doi.org/10.1037/a0040258.
Article3. Mettler T, Raptis DA. What constitutes the field of health information systems? Fostering a systematic framework and research agenda. Health Informatics Journal. 2012; 18(2):147–156. https://doi.org/10.1177/1460458212452496.
Article4. Barnard A. Radical nursing and the emergence of technique as healthcare technology. Nursing Philosophy. 2016; 17(1):8–18. https://doi.org/10.1111/nup.12103.
Article5. Yoon KJ, Song TM, Choi SE, Jung Y, Lee KH. Challenges for activating the convergence of ICT and healthcare services. Sejong: Korea Institute for Health and Social Affairs;2016. December. Report No.:2016-51.6. Tak SH, Benefield LE, Mahoney DF. Technology for long-term care. Research in Gerontological Nursing. 2010; 3(1):61–72. https://doi.org/10.3928/19404921-20091103-01.
Article7. Braun R, Catalani C, Wimbush J, Israelski D. Community health workers and mobile technology: A systematic review of the literature. Public Library of Science ONE. 2013; 8(6):e65772. https://doi.org/10.1371/journal.pone.0065772.
Article8. Jamal A, McKenzie K, Clark M. The impact of health information technology on the quality of medical and health care: A systematic review. Health Information Management Journal. 2009; 38(3):26–37. https://doi.org/10.1177/183335830903800305.
Article9. Prgomet M, Georgiou A, Westbrook JI. The impact of mobile handheld technology on hospital physicians' work practices and patient care: A systematic review. Journal of the American Medical Informatics Association. 2009; 16(6):792–801. https://doi.org/10.1197/jamia.M3215.
Article10. Choi M, Kong S, Jung D. Computer and internet interventions for loneliness and depression in older adults: A meta-analysis. Healthcare Informatics Research. 2012; 18(3):191–198. https://doi.org/10.4258/hir.2012.18.3.191.
Article11. Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petti-crew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews. 2015; 4(1):https://doi.org/10.1186/2046-4053-4-1.
Article12. Scottish Intercollegiate Guidelines Network. SIGN 50: A guideline developer's handbook. Edinburgh: Scottish Intercollegiate Guidelines Network;2015. p. 104.13. Kim SY, Park JE, Seo HJ, Lee YJ, Jang BH, Son HJ, Suh HS, Shin CM. NECA's guidance for undertaking systematic reviews and meta-analyses for intervention. Seoul: National Evidence-based Healthcare Collaborating Agency;2011. p. 271.14. Stevenson D. Information and communications technology in UK schools: An independent inquiry. London: Independent ICT in Schools Commission;1997. March. p. 41.15. LeadingAge CAST. State of technology in aging services [Internet]. Washington D.C.: LeadingAge;2011. [cited 2016 Sep 1]. Available from:. http://hweb.leadingage.org/State_of_Technology_in_Aging_Services_Report.aspx.16. LeadingAge CAST. Telehealth and remote patient monitoring for long-term and post-acute care: a primer and provider selection guide [Internet]. Washington D.C.: LeadingAge;2013. [cited 2016 Sep 1]. Available from:. http://www.leadingage.org/white-papers/telehealth-and-remote-patient-monitoring-long-term-and-post-acute-care-primer-and.17. Czaja SJ. The potential role of technology in supporting older adults. Public Policy & Aging Report,. 2017; 27(2):44–48. https://doi.org/10.1093/ppar/prx006.
Article18. Finkel S. Introduction to behavioural and psychological symptoms of dementia (BPSD). International Journal of Geriatric Psychiatry. 2000; 15(1):S2–S4. https://doi.org/10.1002/(SICI)1099-1166(200004)15:1+3.0.CO;2-3.
Article19. O'Connor C, Smith R, Nott M, Lorang C, Mathews RM. Using video simulated presence to reduce resistance to care and increase participation of adults with dementia. American Journal of Alzheimer's Disease & Other Dementias. 2011; 26(4):317–325. https://doi.org/10.1177/1533317511410558.20. Camberg L, Woods P, Ooi WL, Hurley A, Volicer L, Ashley J, et al. Evaluation of simulated presence: A personalized approach to enhance well-being in persons with Alzheimer's disease. Journal of the American Geriatrics Society. 1999; 47(4):446–452. https://doi.org/10.1111/j.1532-5415.1999.tb07237.x.
Article21. Smalbrugge M, Pot AM, Jongenelis L, Gundy CM, Beekman ATF, Eefsting JA. The impact of depression and anxiety on well being, disability and use of health care services in nursing home patients. International Journal of Geriatric Psychiatry. 2006; 21(4):325–332. https://doi.org/10.1002/gps.1466.
Article22. Barca ML, Engedal K, Laks J, Selbaek G. A 12 months follow-up study of depression among nursing-home patients in Norway. Journal of Affective Disorders. 2010; 120(1-3):141–148. https://doi.org/10.1016/j.jad.2009.04.028.23. Jøranson N, Pedersen I, Rokstad AMM, Ihlebæk C. Effects on symptoms of agitation and depression in persons with dementia participating in robot-assisted activity: A cluster-randomized controlled trial. The Journal of Post-Acute and Long-Term Care Medicine. 2015; 16(10):867–873. https://doi.org/10.1016/j.jamda.2015.05.002.
Article24. Tsai HH, Tsai YF. Changes in depressive symptoms, social support, and loneliness over 1 year after a minimum 3-month vid-eoconference program for older nursing home residents. Journal of Medical Internet Research. 2011; 13(4):e93.
Article25. De Luca R, Bramanti A, De Cola MC, Leonardi S, Torrisi M, Aragona B, et al. Cognitive training for patients with dementia living in a sicilian nursing home: A novel web-based approach. Neurological Sciences. 2016; 37(10):1685–1691. https://doi.org/10.1007/s10072-016-2659-x.
Article26. Sihvonen SE, Sipilä S, Era PA. Changes in postural balance in frail elderly women during a 4-week visual feedback training: A randomized controlled trial. Gerontology. 2004; 50(2):87–95. https://doi.org/10.1159/000075559.
Article27. Kong HJ, Kim J, Hwang EJ, Hong JY, Kin SH. Effects of healthcare smart home exercise program on the metabolic syndrome risk factors of obese elderly women. Journal of the Korean Gerontological Society. 2014; 34(1):103–114.28. Korea Ministry of Health & Welfare. Eup-myeon-dong welfare hub, greatly expanded from 980 to 2,100 [Internet]. Sejong: Korea Ministry of Health & Welfare;2017. [cited 2017 August 19]. Available from:. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=52&CONT_SEQ=338039.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Case study of a long-term care resident with oral health problem
- The Effects of Non-pharmacological Interventions on Sleep among Older Adults in Korean Long-term Care Facilities: A Systematic Review and Meta-analysis
- Geriatric Long-Term Care Practice in Korea
- Sleep Patterns of Older Residents in Long-Term-Care Facilities: A Comparison with Older Adults in Home-Care Services and Community-Dwelling Older Adults
- Research trends on dysphagia among Korean older adults in long-term care facilities: A scoping review