J Cardiovasc Imaging.
2018 Jun;26(2):93-102. 10.4250/jcvi.2018.26.e10.
Cardiac and Pericardial 18F-FDG Uptake on Oncologic PET/CT: Comparison with Echocardiographic Findings
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Seoul, St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea. younhj@catholic.ac.kr
- 3Division of Nuclear Medicine, Department of Radiology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 2415459
- DOI: http://doi.org/10.4250/jcvi.2018.26.e10
Abstract
- BACKGROUND
Interpretation of cardiac uptake on 18-fluorodeoxyglucose positron emission tomography/computed tomography (18F-FDG PET/CT) is often confounded by intense physiological FDG uptake and numerous benign conditions. The aim of the study was to describe the echocardiographic features in concordance with cardiac and pericardial 18F-FDG uptake on whole-body oncology PET/CT.
METHODS
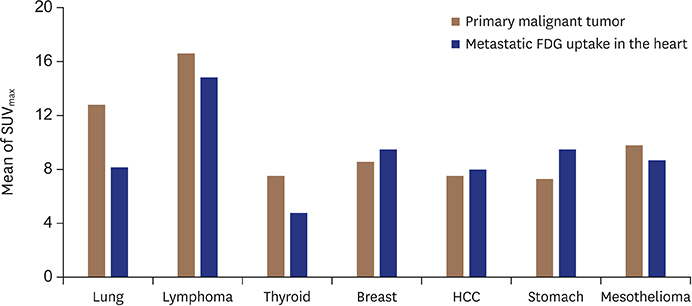
We enrolled 43 consecutive patients (34 solid tumors, 8 lymphomas and 1 leukemia) who were newly diagnosed with non-cardiac malignancy showing incidental cardiac or pericardial 18F-FDG uptake on PET/CT and underwent transthoracic Doppler echocardiography (TTE) within 1 month of PET/CT. The maximum standardized uptake (SUVmax) of all lesions was measured.
RESULTS
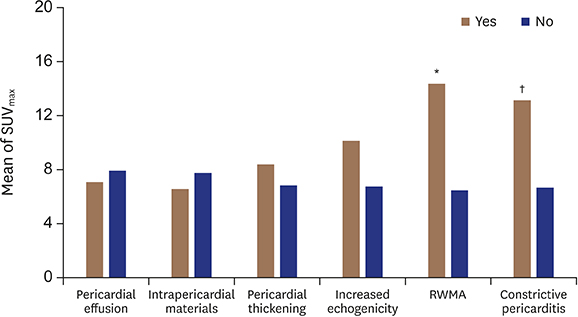
Fifty-six 18F-FDG uptake lesions (32 pericardium, 7 myocardium, 9 cardiac chambers and 8 great vessels) were found, and pericardial effusion was the most common echocardiographic finding (22/43, 51.2%) among study population. Pericardial FDG uptake was shown as pericardial effusion (68.8%), intrapericardial echogenic materials (31.3%), pericardial thickening (28.1%), hyperechogenicity of myopericardium (18.8%), and restricted sliding movement or constrictive pericarditis (15.6%) on TTE. Lesions with regional wall motion abnormality (p = 0.004) or constrictive pericarditis (p = 0.021) had significantly higher mean SUVmax than those without. Myocardial FDG uptake demonstrated pericardial effusion (57.1%), regional wall motion abnormality (57.1%), and increased myocardial wall thickness (42.9%). All cardiac chamber FDG uptakes showed intracardiac mass on TTE.
CONCLUSIONS
Cardiac or pericardial 18F-FDG uptake on oncology PET/CT shows characteristic echocardiographic features according to which heart sites are involved.
MeSH Terms
Figure
Reference
-
1. Bussani R, De-Giorgio F, Abbate A, Silvestri F. Cardiac metastases. J Clin Pathol. 2007; 60:27–34.
Article2. Bisel HF, Wroblewski F, Ladue JS. Incidence and clinical manifestations of cardiac metastases. J Am Med Assoc. 1953; 153:712–715.
Article3. Lam KY, Dickens P, Chan AC. Tumors of the heart. A 20-year experience with a review of 12,485 consecutive autopsies. Arch Pathol Lab Med. 1993; 117:1027–1031.4. Butany J, Leong SW, Carmichael K, Komeda M. A 30-year analysis of cardiac neoplasms at autopsy. Can J Cardiol. 2005; 21:675–680.5. McDonnell PJ, Mann RB, Bulkley BH. Involvement of the heart by malignant lymphoma: a clinicopathologic study. Cancer. 1982; 49:944–951.
Article6. Weber WA. Positron emission tomography as an imaging biomarker. J Clin Oncol. 2006; 24:3282–3292.
Article7. Fischman AJ. Positron emission tomography in the clinical evaluation of metastatic cancer. J Clin Oncol. 1996; 14:691–696.
Article8. Fletcher JW, Djulbegovic B, Soares HP, et al. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med. 2008; 49:480–508.
Article9. Ding HJ, Shiau YC, Wang JJ, Ho ST, Kao A. The influences of blood glucose and duration of fasting on myocardial glucose uptake of [18F]fluoro-2-deoxy-D-glucose. Nucl Med Commun. 2002; 23:961–965.
Article10. Kaneta T, Hakamatsuka T, Takanami K, et al. Evaluation of the relationship between physiological FDG uptake in the heart and age, blood glucose level, fasting period, and hospitalization. Ann Nucl Med. 2006; 20:203–208.
Article11. Fukuchi K, Ohta H, Matsumura K, Ishida Y. Benign variations and incidental abnormalities of myocardial FDG uptake in the fasting state as encountered during routine oncology positron emission tomography studies. Br J Radiol. 2007; 80:3–11.
Article12. Maurer AH, Burshteyn M, Adler LP, Steiner RM. How to differentiate benign versus malignant cardiac and paracardiac 18F FDG uptake at oncologic PET/CT. Radiographics. 2011; 31:1287–1305.13. Johnson MH, Soulen RL. Echocardiography of cardiac metastases. AJR. 1983; 141:677–681.
Article14. Kutalek SP, Panidis IP, Kotler MN, Mintz GS, Carver J, Ross JJ. Metastatic tumors of the heart detected by two-dimensional echocardiography. Am Heart J. 1985; 109:343–349.
Article15. Tominaga K, Shinkai T, Eguchi K, et al. The value of two-dimensional echocardiography in detecting malignant tumors in the heart. Cancer. 1986; 58:1641–1647.
Article16. Auger D, Pressacco J, Marcotte F, Tremblay A, Dore A, Ducharme A. Cardiac masses: an integrative approach using echocardiography and other imaging modalities. Heart. 2011; 97:1101–1109.
Article17. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270.
Article18. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the Evaluation of Left Ventricular Diastolic Function by Echocardiography: An Update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016; 17:1321–1360.
Article19. Klein AL, Abbara S, Agler DA, et al. American Society of Echocardiography clinical recommendations for multimodality cardiovascular imaging of patients with pericardial disease: endorsed by the Society for Cardiovascular Magnetic Resonance and Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2013; 26:965–1012.e15.20. Lobert P, Brown RK, Dvorak RA, Corbett JR, Kazerooni EA, Wong KK. Spectrum of physiological and pathological cardiac and pericardial uptake of FDG in oncology PET-CT. Clin Radiol. 2013; 68:e59–e71.21. Sheikine Y, Di Carli MF. Integrated PET/CT in the assessment of etiology and viability in ischemic heart failure. Curr Heart Fail Rep. 2008; 5:136–142.
Article22. Kobylecka M, Maczewska J, Fronczewska-Wieniawska K, Mazurek T, Plazińska MT, Królicki L. Myocardial viability assessment in 18FDG PET/CT study (18FDG PET myocardial viability assessment). Nucl Med Rev Cent East Eur. 2012; 15:52–60.
Article23. Reynen K, Köckeritz U, Strasser RH. Metastases to the heart. Ann Oncol. 2004; 15:375–381.
Article24. MacGee W. Metastatic and invasive tumours involving the heart in a geriatric population: a necropsy study. Virchows Arch A Pathol Anat Histopathol. 1991; 419:183–189.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison Study of Esophageal Findings on 18F-FDG PET/CT and Esophagogastroduodenoscopy
- Esophageal Leiomyoma with intense FDG uptake on 18F-FDG PET/CT
- Radiography, Bone Scan, and F-18 FDG PET/CT Imaging Findings in a Patient with Paget's Disease
- Use of 18F-FDG PET/CT in Second Primary Cancer
- Uptake of 18F-FDG in the Angioleiomyoma of the Leg