J Dent Anesth Pain Med.
2018 Jun;18(3):177-182. 10.17245/jdapm.2018.18.3.177.
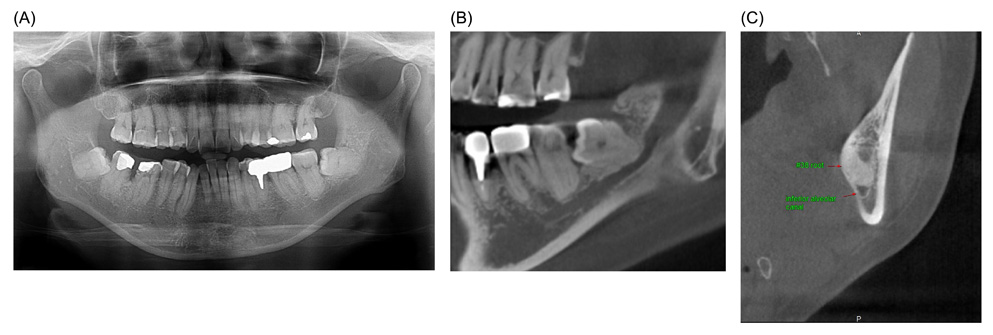
Delayed paresthesia of inferior alveolar nerve after dental surgery: case report and related pathophysiology
- Affiliations
-
- 1Department of Advanced General Dentistry, School of Dentistry, Dankook University, Cheonan, Korea. bestdenmin@naver.com
- KMID: 2415182
- DOI: http://doi.org/10.17245/jdapm.2018.18.3.177
Abstract
- Paresthesia is an altered sensation of the skin, manifesting as numbness, partial loss of local sensitivity, burning, or tingling. The inferior alveolar nerve (IAN) is the third branch of the trigeminal nerve and is very important in dental treatment. IAN paresthesia may occur after various dental procedures such as simple anesthetic injections, surgical procedures, and endodontic treatment, and is reported to range from 0.35% to 8.4%. The altered sensation usually follows immediately after the procedure, and reports of late onset of nerve involvement are rare. This report presents a rare case of delayed paresthesia after dental surgery and discusses the pathophysiology of IAN delayed paresthesia.
Figure
Cited by 1 articles
-
A ramus cortical bone harvesting technique without bone marrow invasion
Jeong-Kui Ku, Min-Soo Ghim, Jung Ho Park, Dae Ho Leem
J Korean Assoc Oral Maxillofac Surg. 2023;49(2):100-104. doi: 10.5125/jkaoms.2023.49.2.100.
Reference
-
1. Ahmad M. The Anatomical Nature of Dental Paresthesia: A Quick Review. Open Dent J. 2018; 12:155–159.
Article2. Shadmehr E, Shekarchizade N. Endodontic periapical lesion-induced mental nerve paresthesia. Dent Res J (Isfahan). 2015; 12:192–196.3. Smith MH, Lung KE. Nerve injuries after dental injection: a review of the literature. J Can Dent Assoc. 2006; 72:559–564.4. Lvovsky A, Bachrach S, Kim HC, Pawar A, Levinzon O, Ben Itzhak J, et al. Relationship between Root Apices and the Mandibular Canal: A Cone-beam Computed Tomographic Comparison of 3 Populations. J Endod. 2018; 44:555–558.
Article5. Devine M, Hirani M, Durham J, Nixdorf DR, Renton T. Identifying criteria for diagnosis of post-traumatic pain and altered sensation of the maxillary and mandibular branches of the trigeminal nerve: a systematic review. Oral Surg Oral Med Oral Pathol Oral Radiol. 2018; 125:526–540.
Article6. Sarikov R, Juodzbalys G. Inferior alveolar nerve injury after mandibular third molar extraction: a literature review. J Oral Maxillofac Res. 2014; 5:e1.
Article7. Shavit I, Juodzbalys G. Inferior alveolar nerve injuries following implant placement - importance of early diagnosis and treatment: a systematic review. J Oral Maxillofac Res. 2014; 5:e2.
Article8. Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg. 2010; 39:320–326.
Article9. Charan Babu HS, Reddy PB, Pattathan RK, Desai R, Shubha AB. Factors influencing lingual nerve paraesthesia following third molar surgery: a prospective clinical study. J Maxillofac Oral Surg. 2013; 12:168–172.
Article10. Borgonovo A, Bianchi A, Marchetti A, Censi R, Maiorana C. An uncommon clinical feature of IAN injury after third molar removal: a delayed paresthesia case series and literature review. Quintessence Int. 2012; 43:353–359.11. Flanagan D. Delayed onset of altered sensation following dental implant placement and mental block local anesthesia: a case report. Implant Dent. 2002; 11:324–330.
Article12. Goldberg MH, Galbraith DA. Late onset of mandibular and lingual dysesthesia secondary to postextraction infection. Oral Surg Oral Med Oral Pathol. 1984; 58:269–271.
Article13. Tolstunov L, Pogrel MA. Delayed paresthesia of inferior alveolar nerve after extraction of mandibular third molar: case report and possible etiology. J Oral Maxillofac Surg. 2009; 67:1764–1766.
Article14. Smyth J, Marley J. An unusual delayed complication of inferior alveolar nerve block. Br J Oral Maxillofac Surg. 2010; 48:51–52.
Article15. Kipp DP, Goldstein BH, Weiss WW Jr. Dysesthesia after mandibular third molar surgery: a retrospective study and analysis of 1,377 surgical procedures. J Am Dent Assoc. 1980; 100:185–192.
Article16. Poort LJ, van Neck JW, van der Wal KG. Sensory testing of inferior alveolar nerve injuries: a review of methods used in prospective studies. J Oral Maxillofac Surg. 2009; 67:292–300.
Article17. Seddon HJ. Three types of nerve injury. Brain. 1943; 66:237–288.
Article18. Donoff RB. Nerve regeneration: basic and applied aspects. Crit Rev Oral Biol Med. 1995; 6:18–24.
Article19. Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008; 119:1951–1965.
Article20. Dahlin LB, Danielsen N, Ehira T, Lundborg G, Rydevik B. Mechanical effects of compression of peripheral nerves. J Biomech Eng. 1986; 108:120–122.
Article21. Blum IR. Contemporary views on dry socket (alveolar osteitis): a clinical appraisal of standardization, aetiopathogenesis and management: a critical review. Int J Oral Maxillofac Surg. 2002; 31:309–317.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tooth hypersensitivity associated with paresthesia after inferior alveolar nerve injury: case report and related neurophysiology
- Diplopia after Inferior Alveolar Nerve Block Anesthesia: A Case Report
- Diplopia after inferior alveolar nerve block: case report and related physiology
- Mental nerve paresthesia secondary to initiation of endodontic therapy: a case report
- Surgical Removal of Dental Implants Dislocated Into the Mandibular Body