Korean Circ J.
2018 May;48(5):418-426. 10.4070/kcj.2017.0017.
Assessment of Potential Renal Dysfunction in Patients with Congenital Heart Disease after Biventricular Repair
- Affiliations
-
- 1Department of Pediatrics, Asahikawa Medical University, Asahikawa, Japan. oka5p@asahikawa-med.ac.jp
- KMID: 2414910
- DOI: http://doi.org/10.4070/kcj.2017.0017
Abstract
- BACKGROUND AND OBJECTIVES
There are few reports on renal dysfunction in the remote period after biventricular repair, and biomarkers for early detection of renal dysfunction are not well understood. We examined whether early fluctuation of biomarkers of renal function occurs in the remote period after biventricular repair in patients with congenital heart disease (CHD).
METHODS
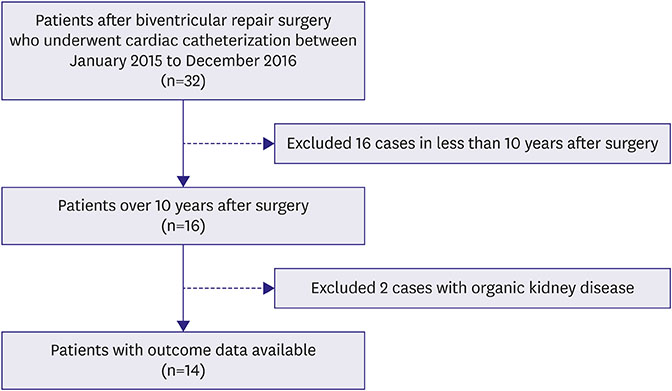
Fourteen patients with CHD after biventricular repair were included. The examination values obtained by cardiac catheterization test and renal function indices based on blood and urine sampling were compared.
RESULTS
The median estimated glomerular filtration rate (eGFR) of creatinine was 113 mL/min/1.73 m2, and the median eGFR of cystatin C was 117 mL/min/1.73 m2. A urine albumin-to-creatinine ratio (UACR) ≥10 mg/gCr was considered a risk factor for cardiovascular disease in 6 (43%) patients. There was a significant difference in right ventricular ejection fraction and deviation in right ventricular end-diastolic volume from the normal value between the 2 groups divided by UACR. Cyanosis before biventricular repair was noted in 2 (25%) patients with UACR < 10 mg/gCr and in 4 (67%) patients with UACR ≥10 mg/gCr.
CONCLUSIONS
Increased UACR was noted in 43% of patients. In patients with UACR ≥10 mg/gCr, right heart system abnormality was observed, and several patients had cyanosis before radical treatment. Measurement for UACR may be able to detect renal dysfunction early in the postoperative remote period.
MeSH Terms
Figure
Cited by 1 articles
-
Increased Urine Albumin-to-Creatinine Ratio-a Harbinger of Renal Dysfunction after Repair of Congenital Heart Disease?
Soo Jung Kang
Korean Circ J. 2018;48(5):435-437. doi: 10.4070/kcj.2018.0128.
Reference
-
1. Perloff JK, Warnes CA. Challenges posed by adults with repaired congenital heart disease. Circulation. 2001; 103:2637–2643.
Article2. Dimopoulos K, Diller GP, Koltsida E, et al. Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation. 2008; 117:2320–2328.
Article3. Guglin M, Rivero A, Matar F, Garcia M. Renal dysfunction in heart failure is due to congestion but not low output. Clin Cardiol. 2011; 34:113–116.
Article4. Sharma S, Ruebner RL, Furth SL, Dodds KM, Rychik J, Goldberg DJ. Assessment of kidney function in survivors following fontan palliation. Congenit Heart Dis. 2016; 11:630–636.
Article5. Uemura O, Nagai T, Ishikura K, et al. Creatinine-based equation to estimate the glomerular filtration rate in Japanese children and adolescents with chronic kidney disease. Clin Exp Nephrol. 2014; 18:626–633.
Article6. Uemura O, Nagai T, Ishikura K, et al. Cystatin C-based equation for estimating glomerular filtration rate in Japanese children and adolescents. Clin Exp Nephrol. 2014; 18:718–725.
Article7. Matsuo S, Imai E, Horio M, et al. Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis. 2009; 53:982–992.
Article8. Horio M, Imai E, Yasuda Y, Watanabe T, Matsuo S. GFR estimation using standardized serum cystatin C in Japan. Am J Kidney Dis. 2013; 61:197–203.
Article9. Nakazawa M, Marks RA, Isabel-Jones J, Jarmakani JM. Right and left ventricular volume characteristics in children with pulmonary stenosis and intact ventricular septum. Circulation. 1976; 53:884–890.
Article10. Yana A, Masutani S, Kojima T, et al. Usefulness of cystatin C in the postoperative management of pediatric patients with congenital heart disease. Circ J. 2013; 77:667–672.
Article11. Mogensen CE, Christensen CK. Predicting diabetic nephropathy in insulin-dependent patients. N Engl J Med. 1984; 311:89–93.
Article12. Nelson RG, Bennett PH, Beck GJ, et al. Development and progression of renal disease in Pima Indians with non-insulin-dependent diabetes mellitus. Diabetic Renal Disease Study Group. N Engl J Med. 1996; 335:1636–1642.13. Gerstein HC, Mann JF, Yi Q, et al. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA. 2001; 286:421–426.
Article14. Arnlöv J, Evans JC, Meigs JB, et al. Low-grade albuminuria and incidence of cardiovascular disease events in nonhypertensive and nondiabetic individuals: the Framingham Heart Study. Circulation. 2005; 112:969–975.15. Stehouwer CD, Nauta JJ, Zeldenrust GC, Hackeng WH, Donker AJ, den Ottolander GJ. Urinary albumin excretion, cardiovascular disease, and endothelial dysfunction in non-insulin-dependent diabetes mellitus. Lancet. 1992; 340:319–323.
Article16. Anne P, Du W, Mattoo TK, Zilberman MV. Nephropathy in patients after Fontan palliation. Int J Cardiol. 2009; 132:244–247.
Article17. Inatomi J, Matsuoka K, Fujimaru R, Nakagawa A, Iijima K. Mechanisms of development and progression of cyanotic nephropathy. Pediatr Nephrol. 2006; 21:1440–1445.
Article18. Mielniczuk LM, Chandy G, Stewart D, et al. Worsening renal function and prognosis in pulmonary hypertension patients hospitalized for right heart failure. Congest Heart Fail. 2012; 18:151–157.
Article19. Mullens W, Abrahams Z, Francis GS, et al. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009; 53:589–596.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Biventricular Repair in DORV with Remote VSD
- Increased Urine Albumin-to-Creatinine Ratio-a Harbinger of Renal Dysfunction after Repair of Congenital Heart Disease?
- Functional Assessment for Congenital Heart Disease
- Biventricular Repair after Bilateral Pulmonary Artery Banding as a Rescue Procedure for a Neonate with Hypoplastic Left Heart Complex
- Postcardiotomy Biventricular Assist Device in Adult Heart Disease