Investig Clin Urol.
2017 Nov;58(6):416-422. 10.4111/icu.2017.58.6.416.
Lymph node yield in node-negative patients predicts cancer specific survival following radical cystectomy for transitional cell carcinoma
- Affiliations
-
- 1Department of Surgery, Austin Health, University of Melbourne, Melbourne, Australia. jackacrozier@gmail.com
- 2St Vincent's Hospital, Melbourne, Australia.
- 3Olivia Newton-John Cancer Research Institute, Melbourne, Australia.
- 4Department of Surgical Oncology, Peter MacCallum Cancer Centre, Melbourne, Australia.
- KMID: 2414768
- DOI: http://doi.org/10.4111/icu.2017.58.6.416
Abstract
- PURPOSE
To determine the oncological implications of increased nodal dissection in node-negative bladder cancer during radical cystectomy in a contemporary Australian series.
MATERIALS AND METHODS
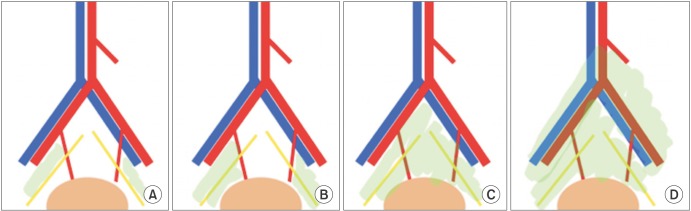
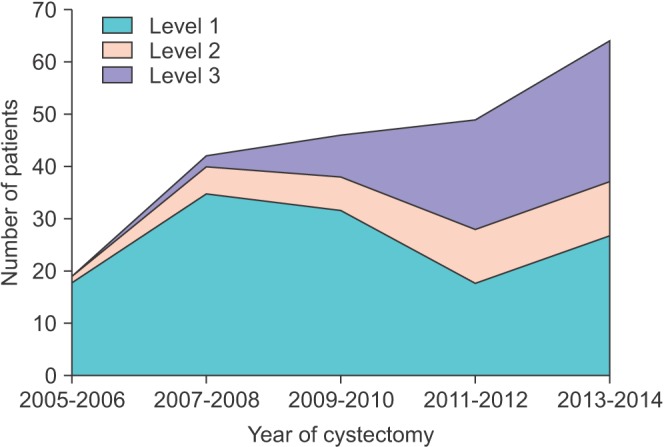
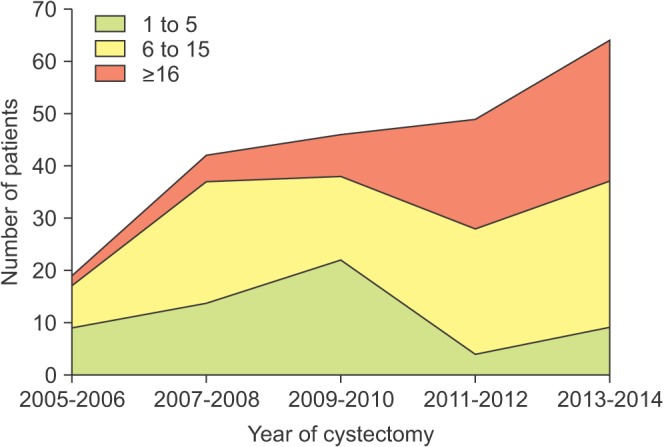
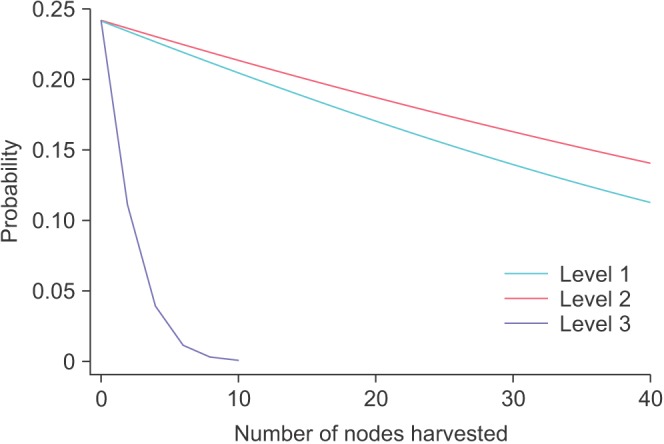
We performed a multicenter retrospective study, including more than 40 surgeons across 5 sites over a 10-year period. We identified 353 patients with primary bladder cancer undergoing radical cystectomy. Extent of lymphadenectomy was defined as follows; limited pelvic lymph node dissection (PLND) (perivesical, pelvic, and obturator), standard PLND (internal and external iliac) and extended PLND (common iliac). Multivariable cox proportional hazards and logistic regression models were used to determine LNY effect on cancer-specific survival.
RESULTS
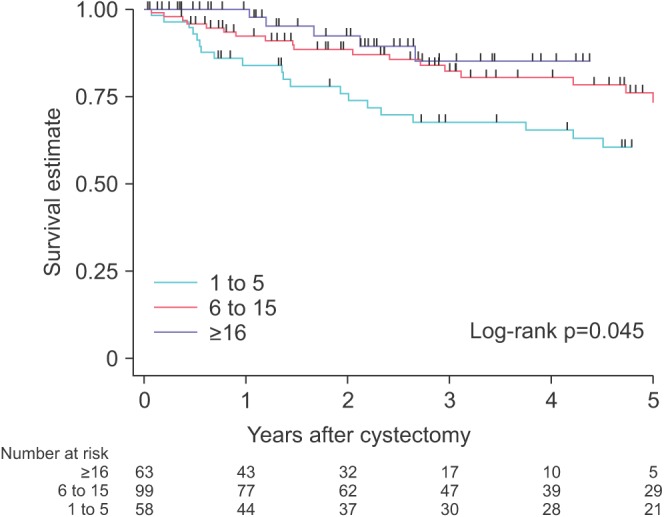
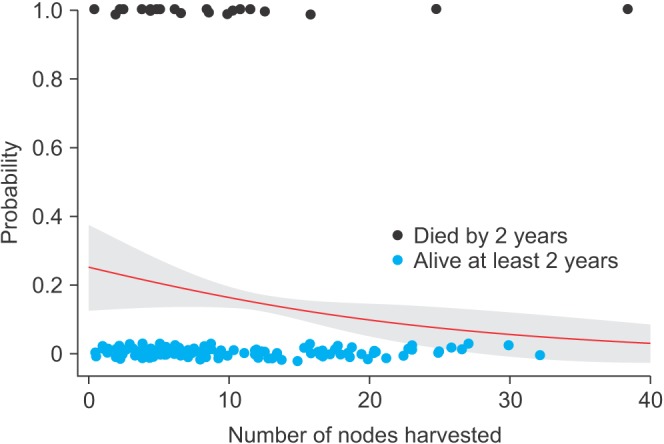
Over the study period, the extent of dissection and lymph node yield increased considerably. In node-negative patients, lymph node yield (LNY) conferred a significantly improved cancer-specific survival. Compared to cases where LNY of 1 to 5 nodes were taken, the hazard ratio (HR) for 6 to 15 nodes harvested was 0.78 (95% confidence interval [CI], 0.43-1.39) and for greater than 15 nodes the HR was 0.31 (95% CI, 0.17-0.57), adjusted for age, sex, T stage, margin status, and year of surgery. The predicted probability of cancer-specific death within 2 years of cystectomy was 16% (95% CI, 13%-19%) with 10 nodes harvested, falling to 5.5% (95% CI, 0%-12%) with 30 nodes taken. Increasing harvest in all PLND templates conferred a survival benefit.
CONCLUSIONS
The findings of the current study highlight the improved oncological outcomes with increased LNY, irrespective of the dissection template. Further prospective research is needed to aid LND data interpretation.
MeSH Terms
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016; 66:7–30. PMID: 26742998.
Article2. Witjes JA, Compérat E, Cowan NC, De Santis M, Gakis G, Lebret T, et al. EAU guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2013 guidelines. Eur Urol. 2014; 65:778–792. PMID: 24373477.
Article3. Patel MI, Bang A, Gillatt D, Smith DP. Contemporary radical cystectomy outcomes in patients with invasive bladder cancer: a population-based study. BJU Int. 2015; 116(Suppl 3):18–25.
Article4. Australian Institute of Health and Welfare. Cancer survival and prevalence in Australia: period estimates from 1982 to 2010. Asia Pac J Clin Oncol. 2013; 9:29–39. PMID: 23418847.5. Vartolomei MD, Kiss B, Vidal A, Burkhard F, Thalmann GN, Roth B. Long-term results of a prospective randomized trial assessing the impact of re-adaptation of the dorsolateral peritoneal layer after extended pelvic lymph node dissection and cystectomy. BJU Int. 2016; 117:618–628. PMID: 25959738.
Article6. Ku JH, Kang M, Kim HS, Jeong CW, Kwak C, Kim HH. Lymph node density as a prognostic variable in node-positive bladder cancer: a meta-analysis. BMC Cancer. 2015; 15:447. PMID: 26027955.
Article7. Simone G, Papalia R, Ferriero M, Guaglianone S, Castelli E, Collura D, et al. Stage-specific impact of extended versus standard pelvic lymph node dissection in radical cystectomy. Int J Urol. 2013; 20:390–397. PMID: 22970939.
Article8. Jensen JB, Ulhøi BP, Jensen KM. Extended versus limited lymph node dissection in radical cystectomy: impact on recurrence pattern and survival. Int J Urol. 2012; 19:39–47. PMID: 22050425.
Article9. Dhar NB, Klein EA, Reuther AM, Thalmann GN, Madersbacher S, Studer UE. Outcome after radical cystectomy with limited or extended pelvic lymph node dissection. J Urol. 2008; 179:873–878. PMID: 18221953.
Article10. Zehnder P, Studer UE, Skinner EC, Dorin RP, Cai J, Roth B, et al. Super extended versus extended pelvic lymph node dissection in patients undergoing radical cystectomy for bladder cancer: a comparative study. J Urol. 2011; 186:1261–1268. PMID: 21849183.
Article11. Koppie TM, Vickers AJ, Vora K, Dalbagni G, Bochner BH. Standardization of pelvic lymphadenectomy performed at radical cystectomy: can we establish a minimum number of lymph nodes that should be removed? Cancer. 2006; 107:2368–2374. PMID: 17041887.12. Wright JL, Lin DW, Porter MP. The association between extent of lymphadenectomy and survival among patients with lymph node metastases undergoing radical cystectomy. Cancer. 2008; 112:2401–2408. PMID: 18383515.
Article13. Holmer M, Bendahl PO, Davidsson T, Gudjonsson S, Månsson W, Liedberg F. Extended lymph node dissection in patients with urothelial cell carcinoma of the bladder: can it make a difference? World J Urol. 2009; 27:521–526. PMID: 19145436.
Article14. Crozier J, Papa N, Sengupta S, Bolton DM, Lawrentschuk N. Changing practice of pelvic lymph node dissection in management of primary bladder cancer. Minerva Urol Nefrol. 2016; 68:106–111. PMID: 26633553.15. Bi L, Huang H, Fan X, Li K, Xu K, Jiang C, et al. Extended vs non-extended pelvic lymph node dissection and their influence on recurrence-free survival in patients undergoing radical cystectomy for bladder cancer: a systematic review and metaanalysis of comparative studies. BJU Int. 2014; 113(5b):E39–E48. PMID: 24053715.
Article16. Cheng L, Montironi R, Davidson DD, Lopez-Beltran A. Staging and reporting of urothelial carcinoma of the urinary bladder. Mod Pathol. 2009; 22(Suppl 2):S70–S95. PMID: 19494855.
Article17. Møller MK, Høyer S, Jensen JB. Extended versus superextended lymph-node dissection in radical cystectomy: subgroup analysis of possible recurrence-free survival benefit. Scand J Urol. 2016; 50:175–180. PMID: 27049808.
Article18. Morgan TM, Barocas DA, Penson DF, Chang SS, Ni S, Clark PE, et al. Lymph node yield at radical cystectomy predicts mortality in node-negative and not node-positive patients. Urology. 2012; 80:632–640. PMID: 22795379.
Article19. May M, Herrmann E, Bolenz C, Brookman-May S, Tiemann A, Moritz R, et al. Association between the number of dissected lymph nodes during pelvic lymphadenectomy and cancer-specific survival in patients with lymph node-negative urothelial carcinoma of the bladder undergoing radical cystectomy. Ann Surg Oncol. 2011; 18:2018–2025. PMID: 21246405.
Article20. Siemens DR, Mackillop WJ, Peng Y, Wei X, Berman D, Booth CM. Lymph node counts are valid indicators of the quality of surgical care in bladder cancer: a population-based study. Urol Oncol. 2015; 33:425.e15–425.e23.
Article21. Konety BR, Joslyn SA, O'Donnell MA. Extent of pelvic lymphadenectomy and its impact on outcome in patients diagnosed with bladder cancer: analysis of data from the Surveillance, Epidemiology and End Results Program data base. J Urol. 2003; 169:946–950. PMID: 12576819.
Article22. Leissner J, Hohenfellner R, Thüroff JW, Wolf HK. Lymphadenectomy in patients with transitional cell carcinoma of the urinary bladder; significance for staging and prognosis. BJU Int. 2000; 85:817–823. PMID: 10792159.
Article23. Roth B, Burkhard FC. The role of lymphadenectomy in radical cystectomy. Eur Urol Suppl. 2010; 9:19–24.
Article24. Youssef RF, Raj GV. Lymphadenectomy in management of invasive bladder cancer. Int J Surg Oncol. 2011; 2011:758189. PMID: 22312522.
Article25. Gazquez C, Ribal MJ, Marín-Aguilera M, Kayed H, Fernández PL, Mengual L, et al. Biomarkers vs conventional histological analysis to detect lymph node micrometastases in bladder cancer: a real improvement? BJU Int. 2012; 110:1310–1316. PMID: 22416928.
Article26. Matsumoto R, Takada N, Abe T, Minami K, Harabayashi T, Nagamori S, et al. Prospective mapping of lymph node metastasis in Japanese patients undergoing radical cystectomy for bladder cancer: characteristics of micrometastasis. Jpn J Clin Oncol. 2015; 45:874–880. PMID: 26109677.
Article27. Buscarini M, Josephson DY, Stein JP. Lymphadenectomy in bladder cancer: a review. Urol Int. 2007; 79:191–199. PMID: 17940349.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effectiveness of Adjuvant Chemotherapy in the Transitional Cell Carcinoma of Urinary Bladder with Lymph Node Involvement Treated by Radical Cystectomy
- The Analysis of Lymph Node Metastases and Survival Rates in Transitional Cell Carcinoma of Urinary Bladder
- The Impact of Pelvic Lymphadenectomy on the Survival of Patients Who Underwent Radical Cystectomy for Transitional Cell Carcinoma of the Bladder
- The Significance of the p53 Protein Overexpression as a Prognostic Marker in Transitional Cell Carcinoma of the Bladder Treated with Radical Cystectomy
- Role of Pelvic Lymphadenectomy in the Treatment of Bladder Cancer: A Mini Review