Clinical experience in managing temporomandibular joint ankylosis: five-year appraisal in a Nigerian subpopulation
- Affiliations
-
- 1Department of Dental and Maxillofacial Surgery, Usmanu Danfodiyo University Teaching Hospital, Sokoto, Nigeria. robdeji@yahoo.com
- 2Department of Surgery, College of Health Sciences, Usmanu Danfodiyo University, Sokoto, Nigeria.
- 3Department of Plastic and Oral & Maxillofacial Surgery, National Orthopaedic Hospital Dalla, Kano, Nigeria.
- 4Department of Oral and Maxillofacial Surgery, College of Medicine, University of Lagos, Lagos, Nigeria.
- 5Department of Oral & Maxillofacial Surgery and Oral Pathology, Obafemi Awolowo University Teaching Hospitals Complex, Ife, Nigeria.
- KMID: 2414430
- DOI: http://doi.org/10.5125/jkaoms.2018.44.3.112
Abstract
OBJECTIVES
Temporomandibular joint ankylosis (TMJA) is a joint pathology caused by bony and/or fibrous adhesion of the joint apparatus, resulting in partial or total loss of function.
MATERIALS AND METHODS
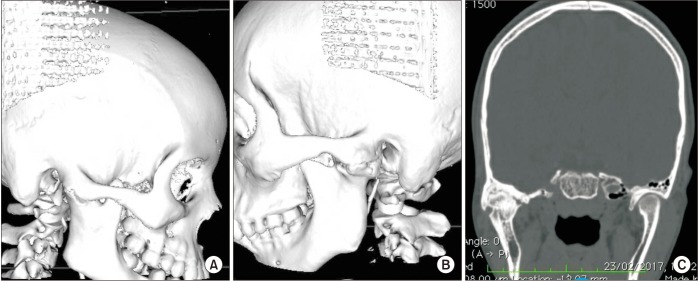
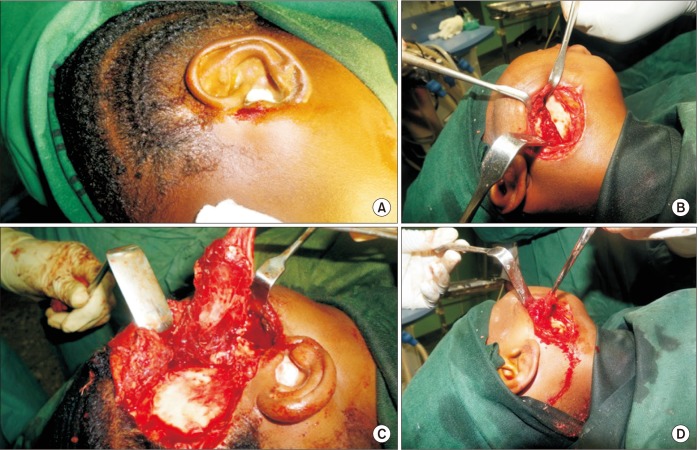
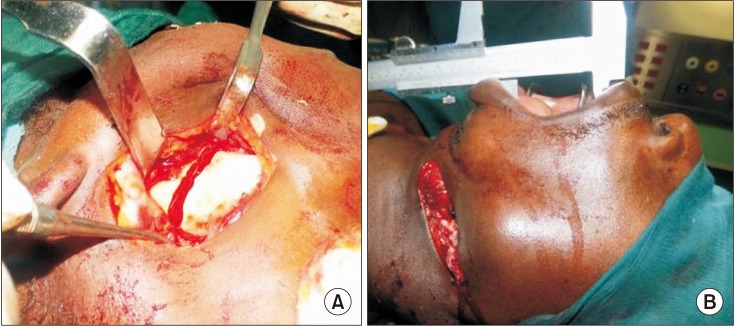
This is a retrospective study conducted between 2012 and 2016 in the northwest region of Nigeria. The data retrieved includes gender, age, etiology of ankylosis, duration of ankylosis, laterality of ankylosis, type of imaging technique, type of airway management, types of incision, surgical procedure, mouth opening, interpositional materials used, and complications. Results were presented as simple frequencies and descriptive statistics.
RESULTS
Thirty-six patients with TMJA were evaluated during the study period. There were 21 males (58.3%) and 15 females (41.7%), yielding a male:female ratio of 1.4:1. The patients' age ranged from 5 to 33 years with mean±standard deviation (13.8±6.6 years). Thirty-five cases (97.2%) were determined to be true/bony ankylosis, while only 1 case (2.8%) was false/fibrous ankylosis. Most of the TMJA cases (16 cases, 44.4%) were secondary to a fall. In our series, the most commonly utilized incision was the Bramley-Al-Kayat (15 cases, 41.7%). The mostly commonly performed procedures were condylectomies and upper ramus ostectomies (12 cases each, 33.3%), while the most commonly used interpositional material was temporalis fascia (14 cases, 38.9%). The complications that developed included 4 cases (11.1%) of severe hemorrhage, 1 case (2.8%) of facial nerve palsy, and 1 case (2.8%) of re-ankylosis.
CONCLUSION
Plain radiographs, with their shortcomings, still have significant roles in investigating TMJA. Aggressive postoperative physiotherapy for a minimum of 6 months is paramount for successful treatment.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Lateral arthroplasty along with buccal fat pad inter-positioning in the management of Sawhney type III temporomandibular joint ankylosis
Vijay Laxmy Malhotra, Virendra Singh, JK Dayashankara Rao, Sunil Yadav, Pranav Gupta, Radhey Shyam, Shruti Kirti
J Korean Assoc Oral Maxillofac Surg. 2019;45(3):129-134. doi: 10.5125/jkaoms.2019.45.3.129.Classification and surgical management of temporomandibular joint ankylosis: a review
Varsha Haridas Upadya, Hari Kishore Bhat, B.H. Sripathi Rao, Srinivas Gosla Reddy
J Korean Assoc Oral Maxillofac Surg. 2021;47(4):239-248. doi: 10.5125/jkaoms.2021.47.4.239.Classification of the journal category “oral surgery” in the Scopus and the Science Citation Index Expanded: flaws and suggestions
Seong-Gon Kim
J Korean Assoc Oral Maxillofac Surg. 2019;45(4):186-191. doi: 10.5125/jkaoms.2019.45.4.186.
Reference
-
1. Erol B, Tanrikulu R, Görgün B. A clinical study on ankylosis of the temporomandibular joint. J Craniomaxillofac Surg. 2006; 34:100–106. PMID: 16423530.
Article2. Roychoudhury A, Parkash H, Trikha A. Functional restoration by gap arthroplasty in temporomandibular joint ankylosis: a report of 50 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999; 87:166–169. PMID: 10052370.3. Obiechina AE, Arotiba JT, Fasola AO. Ankylosis of the temporomandibular joint as a complication of forceps delivery: report of a case. West Afr J Med. 1999; 18:144–146. PMID: 10504875.4. Güven O, Keskin A. Remodelling following condylar fractures in children. J Craniomaxillofac Surg. 2001; 29:232–237. PMID: 11562093.
Article5. Singh V, Sudhakar KNV, Mallela KK, Mohanty R. A review of temporomandibular joint-related papers published between 2014-2015. J Korean Assoc Oral Maxillofac Surg. 2017; 43:368–372. PMID: 29333366.
Article6. Pilmane M, Skagers A. Growth factors, genes, bone proteins and apoptosis in the temporomandibular joint (TMJ) of children with ankylosis and during disease recurrence. Stomatologija. 2011; 13:96–101. PMID: 22071418.7. Kazanjian VH. Ankylosis of the temporomandibular joint. Surg Gynecol Obstet. 1938; 67:333–348.
Article8. Sawhney CP. Bony ankylosis of the temporomandibular joint: follow-up of 70 patients treated with arthroplasty and acrylic spacer interposition. Plast Reconstr Surg. 1986; 77:29–40. PMID: 3941847.9. Vasconcelos BC, Porto GG, Bessa-Nogueira RV, Nascimento MM. Surgical treatment of temporomandibular joint ankylosis: follow-up of 15 cases and literature review. Med Oral Patol Oral Cir Bucal. 2009; 14:E34–E38. PMID: 19114954.
Article10. Erdem E, Alkan A. The use of acrylic marbles for interposition arthroplasty in the treatment of temporomandibular joint ankylosis: follow-up of 47 cases. Int J Oral Maxillofac Surg. 2001; 30:32–36. PMID: 11289618.
Article11. Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990; 48:1145–1151. PMID: 2213309.
Article12. Orubuloye IO, Oni JB. Health transition research in Nigeria in the era of the Structural Adjustment Programme. Health Transit Rev. 1996; (6 Suppl):6:301–324. PMID: 10165307.13. Ogunbekum I. Which direction for health care in Nigeria? Health Policy Plan. 1991; 6:254–261.
Article14. Singh V, Mohammad S, Singh G. Management of TMJ ankylosis and post ankylotic deformities a simultaneous procedure. J Maxillofac Oral Surg. 2005; 5:17–19.15. Miranda HB, Miranda VJE. Temporomandibular joint ankylosis treated with arthroplasty in a patient with reumathoid arthritis. Rev Odont Mex. 2011; 15:164–169.16. Kao SY, Chou J, Lo J, Yang J, Chou AP, Joe CJ, et al. Using three-dimensional-computerized tomography as a diagnostic tool for temporo-mandibular joint ankylosis: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1999; 62:244–249. PMID: 10367487.17. Loveless TP, Bjornland T, Dodson TB, Keith DA. Efficacy of temporomandibular joint ankylosis surgical treatment. J Oral Maxillofac Surg. 2010; 68:1276–1282. PMID: 20304543.
Article18. Zhi K, Ren W, Zhou H, Gao L, Zhao L, Hou C, et al. Management of temporomandibular joint ankylosis: 11 years' clinical experience. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009; 108:687–692. PMID: 19782622.
Article19. Elgazzar RF, Abdelhady AI, Saad KA, Elshaal MA, Hussain MM, Abdelal SE, et al. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg. 2010; 39:333–342. PMID: 20149597.
Article20. de Bont LG, van der Kuijl B, Stegenga B, Vencken LM, Boering G. Computed tomography in differential diagnosis of temporomandibular joint disorders. Int J Oral Maxillofac Surg. 1993; 22:200–209. PMID: 8409559.
Article21. El-Hakim IE, Metwalli SA. Imaging of temporomandibular joint ankylosis. A new radiographic classification. Dentomaxillofac Radiol. 2002; 31:19–23. PMID: 11803384.
Article22. Sanders R, MacEwen CJ, McCulloch AS. The value of skull radiography in ophthalmology. Acta Radiol. 1994; 35:429–433. PMID: 8086247.
Article23. Posnick JC, Goldstein JA. Surgical management of temporomandibular joint ankylosis in the pediatric population. Plast Reconstr Surg. 1993; 91:791–798. PMID: 8460181.
Article24. Joshi UM, Patil SG, Shah K, Allurkar S. Brisement force in fibrous ankylosis: a technique revisited. Indian J Dent Res. 2016; 27:661–663. PMID: 28169267.25. Kulkarni J, Shah K, Ahadghaffarkhan A, Khaire S. Anaesthetic management of temporomandibular joint ankylosis without fibrotic bronchoscope: a review of 31 cases. J Dent Med Sci. 2013; 8:50–54.26. Shah FR, Sharma KR, Hilloowalla RN, Karandikar AD. Anaesthetic considerations of temporomandibular joint ankylosis with obstructive sleep apnoea: a case report. J Indian Soc Pedod Prev Dent. 2002; 20:16–20. PMID: 12435028.27. Braimah RO, Oladejo T, Olarinoye TO, Adetoye AO, Osho PO. A multidisciplinary approach to the management of temporomandibular joint ankylosis in a sickle-cell anemia patient in a resource-limited setting. Ann Maxillofac Surg. 2016; 6:130–134. PMID: 27563622.
Article28. Ellis E, Zide MF. Approaches to the temporomandibular joint. In : Ellis E, Zide MF, editors. Surgical approaches to the facial skeleton. 2nd ed. Philadelphia: Lippincott Williams & Wilkins;2006. p. 191–212.29. Clauser L, Curioni C, Spanio S. The use of the temporalis muscle flap in facial and craniofacial reconstructive surgery. A review of 182 cases. J Craniomaxillofac Surg. 1995; 23:203–214. PMID: 7560105.
Article30. Balaji SM. Modified temporalis anchorage in craniomandibular reankylosis. Int J Oral Maxillofac Surg. 2003; 32:480–485. PMID: 14759105.
Article31. Mohan CM, Prasad BR, Bhat S, Bhat SS. Reconstruction of condyle following surgical correction of temporomandibular joint ankylosis: current concepts and considerations for the future. Nitte Univ J Health Sci. 2014; 4:39–46.32. Abbe R. An operation for the relief of ankylosis of the temporomaxillary joint, by exsection of the neck of the condyle of the lower jaw; with remarks. New York Med J. 1880; 31:362–366.33. Feinberg SE, Larsen PE. The use of a pedicled temporalis musclepericranial flap for replacement of the TMJ disc: preliminary report. J Oral Maxillofac Surg. 1989; 47:142–146. PMID: 2913247.
Article34. Metwalli S. Computerized tomography of the temporal bone in TMJ ankylosis. Cairo: Cairo University;1993.35. Wellisz T, Armstrong JK, Cambridge J, Fisher TC. Ostene, a new water-soluble bone hemostasis agent. J Craniofac Surg. 2006; 17:420–425. PMID: 16770175.
Article36. Wellisz T, Armstrong JK, Cambridge J, An YH, Wen X, Kang Q, et al. The effects of a soluble polymer and bone wax on sternal healing in an animal model. Ann Thorac Surg. 2008; 85:1776–1780. PMID: 18442583.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Difficult airway management in a case with lingual tonsil hypertrophy and temporo-mandibular joint partial ankylosis
- Temporomandibular joint bony ankylosis following postoperative radiotherapy for maxillary cancer
- One-stage total reconstruction of temporomandibular joint ankylosis and facial asymmetry
- Modified T-Plate Interpositional Arthroplasty for Temporomandibular Joint Ankylosis: A New and Versatile Option
- A Case Report of Temporomandibular Bilateral Osseous Ankylosis Treated by Total Joint Replacement in Ankylosing Spondylitis