J Endocr Surg.
2018 Mar;18(1):84-89. 10.16956/jes.2018.18.1.84.
Adrenal Hemangioma: a Rare Incidentaloma
- Affiliations
-
- 1Department of General Surgery, Seth GS Medical College and King Edward Memorial Hospital, Mumbai, India. dramiteshwar@gmail.com
- KMID: 2414425
- DOI: http://doi.org/10.16956/jes.2018.18.1.84
Abstract
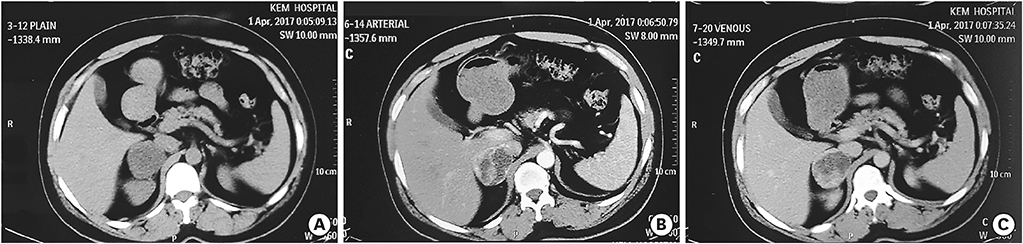
- Hemangioma of the adrenal gland is a rare benign tumor. The diagnosis is often postoperative on histopathological examination with the presence of blood filled, dilated vascular channels. Approximately 60 surgical cases have been reported in the literature so far. We present a case of a 41 years old man who was incidentally found to have a 5 cm right adrenal mass, on abdominal ultrasonography done to evaluate for right renal colicky pain. Contrast enhanced computed tomography (CT) of the abdomen revealed a 5 cm right adrenal lesion with peripheral enhancement on arterial phase with central necrosis consistent with a pheochromocytoma. Laparoscopic adrenalectomy (LA) was performed through a transperitoneal flank approach. Pathological examination revealed a 6 cm adrenal mass with extensive central necrotic areas mixed with dilated vascular channels with the diagnosis of adrenal hemangioma. Adrenal hemangiomas are extremely uncommon. They are mostly incidentally diagnosed owing to their non-secretory nature with non-specific symptom profile. LA is technically safe and feasible for large adrenal tumors, but controversy exists in cases of suspected malignancy. We prefer laparoscopic approach on the basis of preoperative abdominal CT scan that excludes radiological signs of adrenocortical carcinoma such as peri-adrenal infiltration and vascular invasion. LA is considered the standard treatment in case of diagnosis of benign lesions. The most important thing preoperatively is to work out the risk of malignancy and hormonal profile of the patient before going for the excision of the adrenal incidentaloma.
MeSH Terms
Figure
Reference
-
1. Young WF Jr. Clinical practice. The incidentally discovered adrenal mass. N Engl J Med. 2007; 356:601–610.2. Mansmann G, Lau J, Balk E, Rothberg M, Miyachi Y, Bornstein SR. The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev. 2004; 25:309–340.
Article3. Grumbach MM, Biller BM, Braunstein GD, Campbell KK, Carney JA, Godley PA, et al. Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann Intern Med. 2003; 138:424–429.
Article4. Kloos RT, Gross MD, Francis IR, Korobkin M, Shapiro B. Incidentally discovered adrenal masses. Endocr Rev. 1995; 16:460–484.
Article5. Barzon L, Sonino N, Fallo F, Palu G, Boscaro M. Prevalence and natural history of adrenal incidentalomas. Eur J Endocrinol. 2003; 149:273–285.
Article6. Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, et al. Management of adrenal incidentalomas: European Society of Endocrinology clinical practice guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016; 175:G1–G34.
Article7. Salup R, Finegold R, Borochovitz D, Boehnke M, Posner M. Cavernous hemangioma of the adrenal gland. J Urol. 1992; 147:110–112.
Article8. Thiele JW, Bodie B. Adrenal hemangioma. Surgery. 2001; 129:373–374.
Article9. Forbes TL. Retroperitoneal hemorrhage secondary to a ruptured cavernous hemangioma. Can J Surg. 2005; 48:78–79.10. Boraschi P, Campatelli A, Di Vito A, Perri G. Hemorrhage in cavernous hemangioma of the adrenal gland: US, CT and MRI appearances with pathologic correlation. Eur J Radiol. 1995; 21:41–43.
Article