J Endocr Surg.
2018 Mar;18(1):21-36. 10.16956/jes.2018.18.1.21.
Improving Safety of Neural Monitoring in Thyroid Surgery: Educational Considerations in Learning New Procedure
- Affiliations
-
- 1Division for Endocrine and Minimally Invasive Surgery, Department of Human Pathology in Adulthood and Childhood “G. Barresiâ€, University Hospital G. Martino, University of Messina, Messina, Italy. gdionigi@unime.it
- KMID: 2414420
- DOI: http://doi.org/10.16956/jes.2018.18.1.21
Abstract
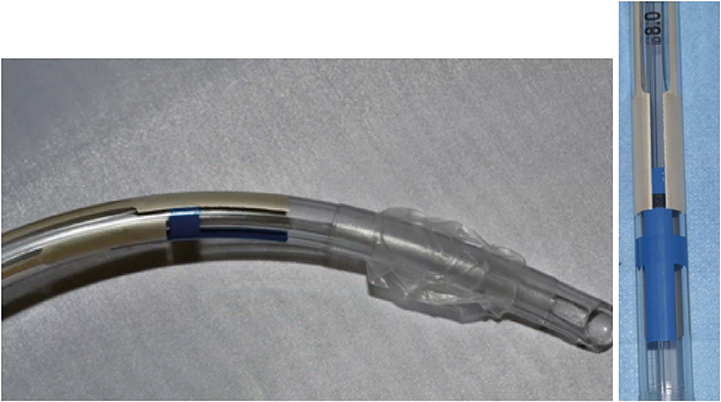
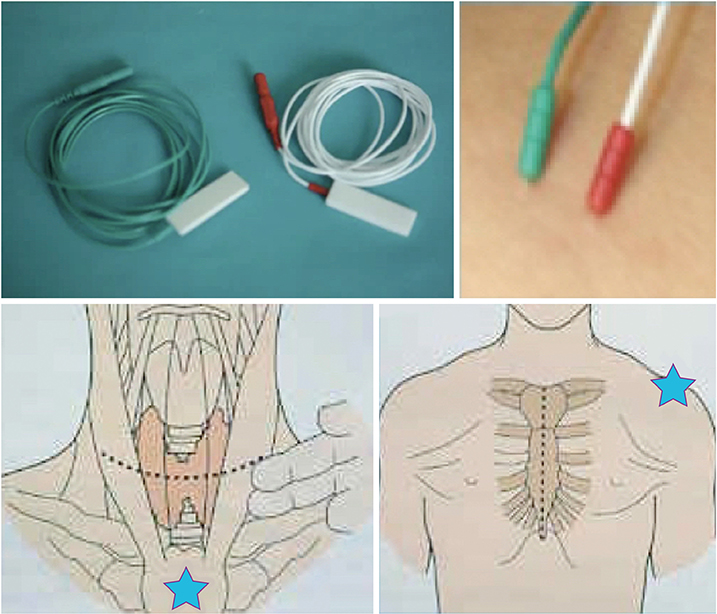
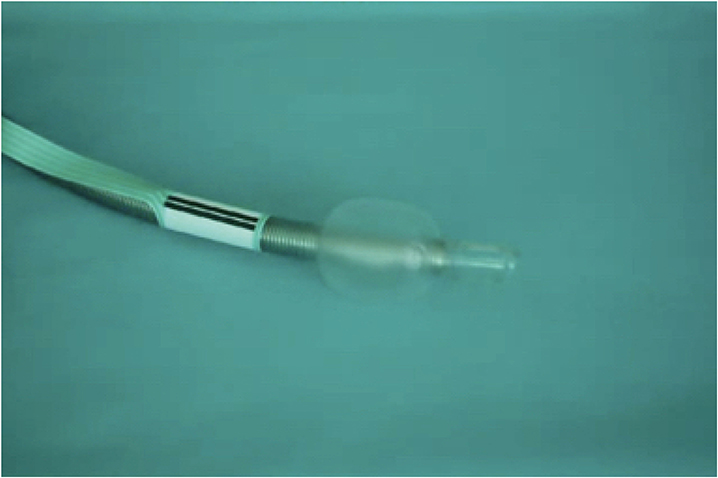
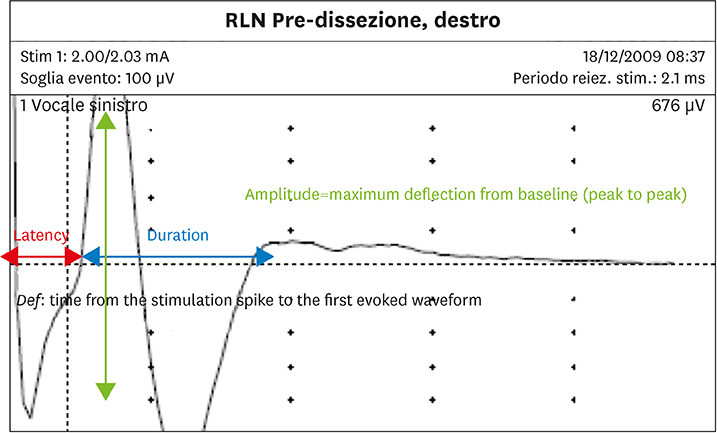
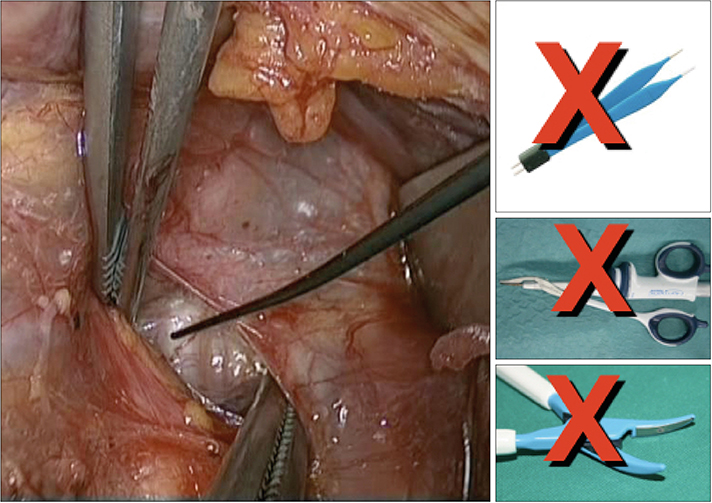
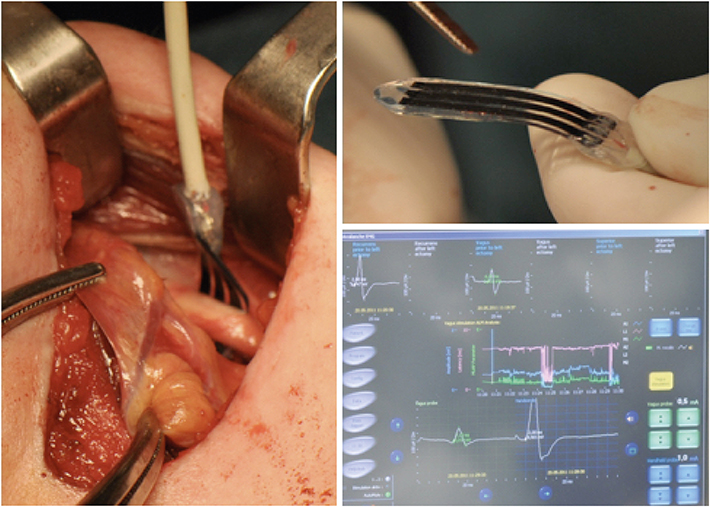
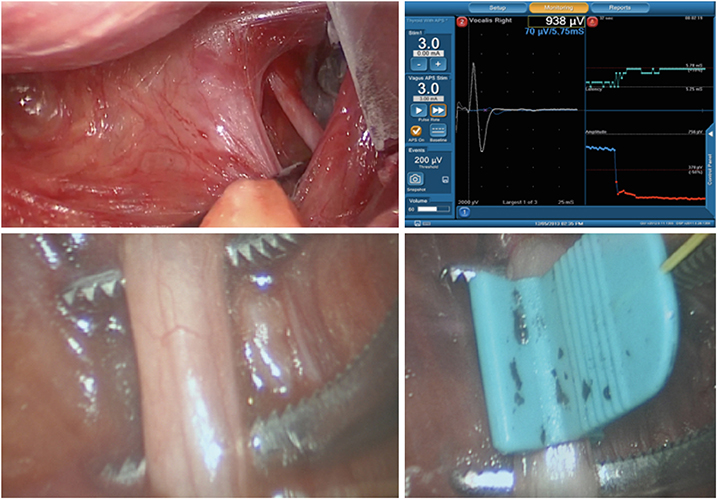
- Literature on intraoperative neuro monitoring (IONM) during endocrine surgery have increased over recent years. A comprehensive understanding of the role of IONM for prevention of nerve injuries is critical to maximize safety during surgery of the anterior compartment of the neck. Neuromonitoring techniques are currently considered safe technique and technology; however, albeit sporadically, have been reported some complications and related side effects using such methods. The complications described can be related to the electrodes positioned at the larynx, at the obstruction of the endotracheal tube, the drugs used for anesthesia and the effects of electrical stimulation on nerve structures and systemic levels. This review will explore the safety issues of IONM to improve the outcomes among patients undergoing monitored thyroidectomy.
MeSH Terms
Figure
Cited by 1 articles
-
The Consistency of Intraoperative Neural Monitoring in Thyroid Surgery
Gianlorenzo Dionigi, Young Jun Chai, Francesco Freni, Özer Makay, Bruno Galletti, Francesco Galletti, Hoon Yub Kim
J Endocr Surg. 2018;18(2):91-97. doi: 10.16956/jes.2018.18.2.91.
Reference
-
1. Lahey FH, Hoover WB. Injuries to the recurrent laryngeal nerve in thyroid operations: their management and avoidance. Ann Surg. 1938; 108:545–562.2. Dralle H, Sekulla C, Haerting J, Timmermann W, Neumann HJ, Kruse E, et al. Risk factors of paralysis and functional outcome after recurrent laryngeal nerve monitoring in thyroid surgery. Surgery. 2004; 136:1310–1322.
Article3. Randolph GW, Dralle H, Abdullah H, Barczynski M, Bellantone R, Brauckhoff M, et al. Electrophysiologic recurrent laryngeal nerve monitoring during thyroid and parathyroid surgery: international standards guideline statement. Laryngoscope. 2011; 121:Suppl 1. S1–16.
Article4. Dionigi G, Barczynski M, Chiang FY, Dralle H, Duran-Poveda M, Iacobone M, et al. Why monitor the recurrent laryngeal nerve in thyroid surgery? J Endocrinol Invest. 2010; 33:819–822.
Article5. Dralle H, Sekulla C, Lorenz K, Brauckhoff M, Machens A; German IONM Study Group. Intraoperative monitoring of the recurrent laryngeal nerve in thyroid surgery. World J Surg. 2008; 32:1358–1366.
Article6. Sanabria A, Silver CE, Suárez C, Shaha A, Khafif A, Owen RP, et al. Neuromonitoring of the laryngeal nerves in thyroid surgery: a critical appraisal of the literature. Eur Arch Otorhinolaryngol. 2013; 270:2383–2395.
Article7. Johnson S, Goldenberg D. Intraoperative monitoring of the recurrent laryngeal nerve during revision thyroid surgery. Otolaryngol Clin North Am. 2008; 41:1147–1154.
Article8. Hermann M, Hellebart C, Freissmuth M. Neuromonitoring in thyroid surgery: prospective evaluation of intraoperative electrophysiological responses for the prediction of recurrent laryngeal nerve injury. Ann Surg. 2004; 240:9–17.9. Chan WF, Lo CY. Pitfalls of intraoperative neuromonitoring for predicting postoperative recurrent laryngeal nerve function during thyroidectomy. World J Surg. 2006; 30:806–812.
Article10. Domosławski P, Lukieńczuk T, Kaliszewski K, Sutkowski K, Wojczys R, Wojtczak B. Safety and current achievements in thyroid surgery with neuromonitoring. Adv Clin Exp Med. 2013; 22:125–130.11. Thomusch O, Sekulla C, Machens A, Neumann HJ, Timmermann W, Dralle H. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg. 2004; 389:499–503.
Article12. Oysu C, Demir K. Life-threatening complication of recurrent laryngeal nerve monitoring with EMG reinforced silicone ETT. J Craniofac Surg. 2011; 22:2419–2421.
Article13. Yap SJ, Morris RW, Pybus DA. Alterations in endotracheal tube position during general anaesthesia. Anaesth Intensive Care. 1994; 22:586–588.
Article14. Paulsen FP, Rudert HH, Tillmann BN. New insights into the pathomechanism of postintubation arytenoid subluxation. Anesthesiology. 1999; 91:659–666.
Article15. Echternach M, Maurer CA, Mencke T, Schilling M, Verse T, Richter B. Laryngeal complications after thyroidectomy: is it always the surgeon? Arch Surg. 2009; 144:149–153.16. Sneyd JR, O’Sullivan E. Tracheal intubation without neuromuscular blocking agents: is there any point? Br J Anaesth. 2010; 104:535–537.
Article17. Shaikh SI, Bellagali VP. Tracheal intubation without neuromuscular block in children. Indian J Anaesth. 2010; 54:29–34.
Article18. Erhan E, Ugur G, Alper I, Gunusen I, Ozyar B. Tracheal intubation without muscle relaxants: remifentanil or alfentanil in combination with propofol. Eur J Anaesthesiol. 2003; 20:37–43.
Article19. Birkholz T, Irouschek A, Saalfrank-Schardt C, Klein P, Schmidt J. Laryngeal morbidity after intubation with or without neuromuscular block in thyroid surgery using recurrent laryngeal nerve monitoring. Auris Nasus Larynx. 2012; 39:288–293.
Article20. Wu CW, Dionigi G, Sun H, Liu X, Kim HY, Hsiao PJ, et al. Intraoperative neuromonitoring for the early detection and prevention of RLN traction injury in thyroid surgery: a porcine model. Surgery. 2014; 155:329–339.
Article21. Choby G, Hollenbeak CS, Johnson S, Goldenberg D. Surface electrode recurrent laryngeal nerve monitoring during thyroid surgery: normative values. J Clin Neurophysiol. 2010; 27:34–37.
Article22. Marcus B, Edwards B, Yoo S, Byrne A, Gupta A, Kandrevas J, et al. Recurrent laryngeal nerve monitoring in thyroid and parathyroid surgery: the University of Michigan experience. Laryngoscope. 2003; 113:356–361.
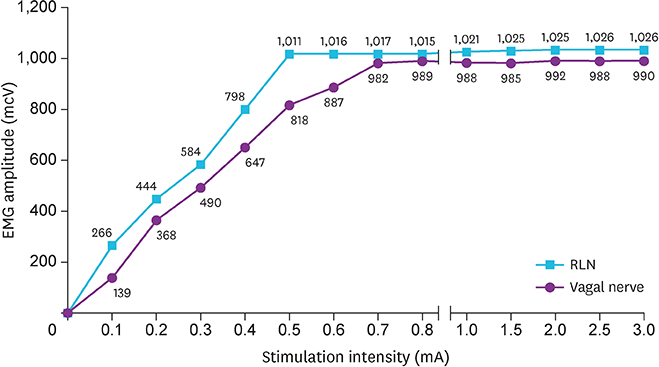
Article23. Wu CW, Lu IC, Randolph GW, Kuo WR, Lee KW, Chen CL, et al. Investigation of optimal intensity and safety of electrical nerve stimulation during intraoperative neuromonitoring of the recurrent laryngeal nerve: a prospective porcine model. Head Neck. 2010; 32:1295–1301.
Article24. Wheless JW, Baumgartner J. Vagus nerve stimulation therapy. Drugs Today (Barc). 2004; 40:501–515.
Article25. Schachter SC, Wheless JW. The evolving place of vagus nerve stimulation therapy. Neurology. 2002; 59:S1–S2.
Article26. Rychlicki F, Zamponi N, Trignani R, Ricciuti RA, Iacoangeli M, Scerrati M. Vagus nerve stimulation: clinical experience in drug-resistant pediatric epileptic patients. Seizure. 2006; 15:483–490.
Article27. Ben-Menachem E. Vagus nerve stimulation, side effects, and long-term safety. J Clin Neurophysiol. 2001; 18:415–418.
Article28. Annegers JF, Coan SP, Hauser WA, Leestma J. Epilepsy, vagal nerve stimulation by the NCP system, all-cause mortality, and sudden, unexpected, unexplained death. Epilepsia. 2000; 41:549–553.
Article29. Ali II, Pirzada NA, Kanjwal Y, Wannamaker B, Medhkour A, Koltz MT, et al. Complete heart block with ventricular asystole during left vagus nerve stimulation for epilepsy. Epilepsy Behav. 2004; 5:768–771.
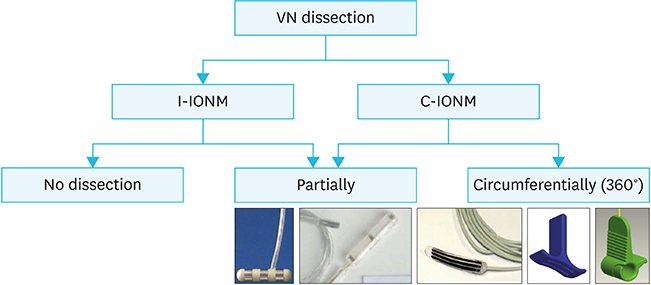
Article30. Friedrich C, Ulmer C, Rieber F, Kern E, Kohler A, Schymik K, et al. Safety analysis of vagal nerve stimulation for continuous nerve monitoring during thyroid surgery. Laryngoscope. 2012; 122:1979–1987.
Article31. Xiaoli L, Wu CW, Kim HY, Tian W, Chiang FY, Liu R, et al. Gastric acid secretion and gastrin release during continuous vagal neuromonitoring in thyroid surgery. Langenbecks Arch Surg. 2017; 402:265–272.
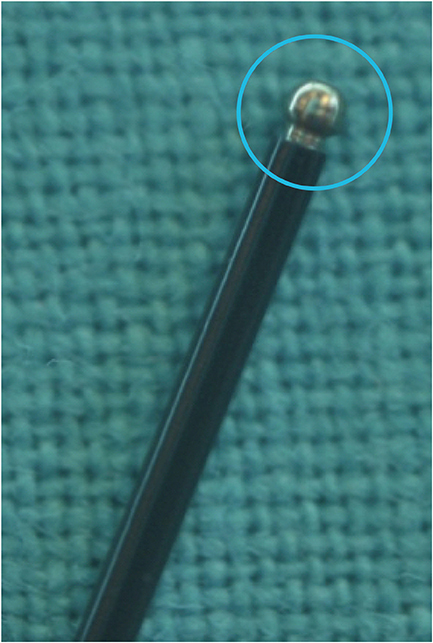
Article32. Mangano A, Kim HY, Wu CW, Rausei S, Hui S, Xiaoli L, et al. Continuous intraoperative neuromonitoring in thyroid surgery: Safety analysis of 400 consecutive electrode probe placements with standardized procedures. Head Neck. 2016; 38:Suppl 1. E1568–E1574.
Article33. Bacuzzi A, Dralle H, Randolph GW, Chiang FY, Kim HY, Barczyński M, et al. Safety of continuous intraoperative neuromonitoring (C-IONM) in thyroid surgery. World J Surg. 2016; 40:768–769.
Article34. Dionigi G, Chiang FY, Dralle H, Boni L, Rausei S, Rovera F, et al. Safety of neural monitoring in thyroid surgery. Int J Surg. 2013; 11:Suppl 1. S120–S126.
Article35. Schneider R, Machens A, Bucher M, Raspé C, Heinroth K, Dralle H. Continuous intraoperative monitoring of vagus and recurrent laryngeal nerve function in patients with advanced atrioventricular block. Langenbecks Arch Surg. 2016; 401:551–556.
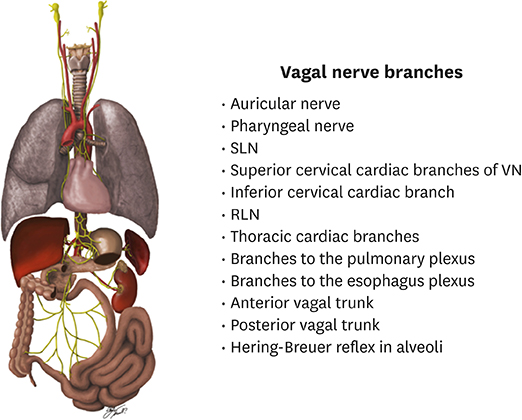
Article36. Dionigi G, Chiang FY, Rausei S, Wu CW, Boni L, Lee KW, et al. Surgical anatomy and neurophysiology of the vagus nerve (VN) for standardised intraoperative neuromonitoring (IONM) of the inferior laryngeal nerve (ILN) during thyroidectomy. Langenbecks Arch Surg. 2010; 395:893–899.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Efficacy of Intraoperative Neural Monitoring (IONM) in Thyroid Surgery: the Learning Curve
- A Case of Papillary Thyroid Carcinoma Accompanied by Zenker’s Diverticulum: Considerations for Surgery
- Novice and Advanced Beginner Nurses’ Patient Safety Management Activities: Mediating Effects of Informal Learning
- Deep Learning in Thyroid Ultrasonography to Predict Tumor Recurrence in Thyroid Cancers
- Vision of Thyroid Surgery: Past, Present and Future