Blood Res.
2018 Mar;53(1):18-24. 10.5045/br.2018.53.1.18.
Reference values for serum ferritin and percentage of transferrin saturation in Korean children and adolescents
- Affiliations
-
- 1Department of Pediatrics, Korea Cancer Center Hospital, Seoul, Korea. limjs@kcch.re.kr
- KMID: 2414360
- DOI: http://doi.org/10.5045/br.2018.53.1.18
Abstract
- BACKGROUND
Ferritin reference values vary by age, gender, and ethnicity. We aimed to determine reference values of serum ferritin (SF) and the percentage of transferrin saturation (TSAT) for Korean children and adolescents.
METHODS
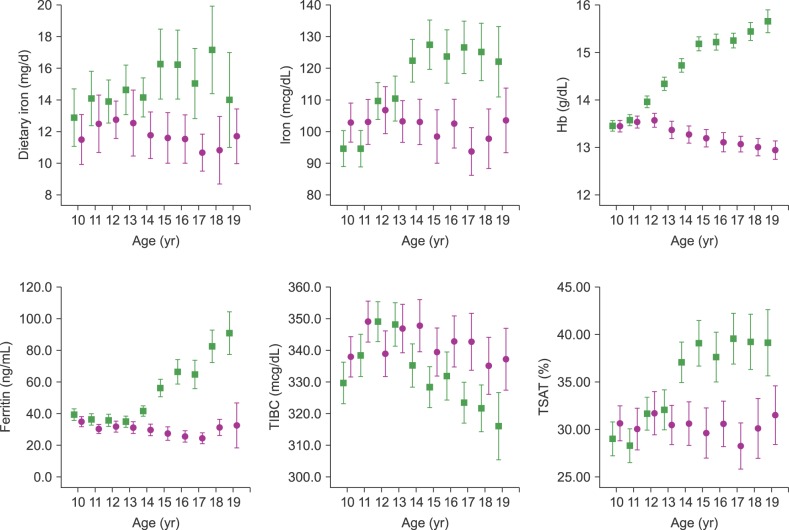
We analyzed data from 2,487 participants (1,311 males and 1,176 females) aged 10-20 years from the Korea National Health and Nutrition Examination Survey (2010-2012). We calculated age- and gender-stratified means and percentile values for SF and TSAT.
RESULTS
We first plotted mean SF and TSAT by gender and according to age. In males, mean SF tended to be relatively constant among participants aged 10 to 14 years, with an upward trend thereafter. Mean SF trended downward among female participants until the age of 15 years and remained constant thereafter. Thus, significant gender differences in ferritin exist from the age of 14 years. High levels of SF were associated with obesity, and lower SF levels were associated with anemia and menarche status.
CONCLUSION
We established reference values of SF and TSAT according to age and gender. The reference values for SF calculated in this study can be used to test the association between SF values and other defined diseases in Korean children and adolescents.
Keyword
MeSH Terms
Figure
Reference
-
1. Wang W, Knovich MA, Coffman LG, Torti FM, Torti SV. Serum ferritin: Past, present and future. Biochim Biophys Acta. 2010; 1800:760–769. PMID: 20304033.
Article2. Arosio P, Elia L, Poli M. Ferritin, cellular iron storage and regulation. IUBMB Life. 2017; 69:414–422. PMID: 28349628.
Article3. Shi J, Long T, Ying R, Wang L, Zhu X, Lin Y. Chemical oxidation of bis(2-chloroethyl) ether in the Fenton process: Kinetics, pathways and toxicity assessment. Chemosphere. 2017; 180:117–124. PMID: 28395149.
Article4. Yi KH, Hwang JS, Lim SW, Lee JA, Kim DH, Lim JS. Ferritin level is associated with metabolic syndrome and elevated alanine aminotransferase in children and adolescents. J Pediatr Endocrinol Metab. 2016; 29:1337–1344. PMID: 27390880.
Article5. Kim YE, Kim DH, Roh YK, et al. Relationship between serum ferritin levels and dyslipidemia in Korean adolescents. PLoS One. 2016; 11:e0153167. PMID: 27070153.
Article6. Na JH, Park SW, Kang Y, Koh H, Kim S. The clinical significance of serum ferritin in pediatric non-alcoholic fatty liver disease. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:248–256. PMID: 25587525.
Article7. Chen L, Li Y, Zhang F, Zhang S, Zhou X, Ji L. Association of serum ferritin levels with metabolic syndrome and insulin resistance in a Chinese population. J Diabetes Complications. 2017; 31:364–368. PMID: 27426616.
Article8. Chakraborty B, Vishnoi G, Goswami B, Gowda SH, Chowdhury D, Agarwal S. Lipoprotein(a), ferritin, and albumin in acute phase reaction predicts severity and mortality of acute ischemic stroke in North Indian patients. J Stroke Cerebrovasc Dis. 2013; 22:e159–e167. PMID: 23253530.
Article9. Shim YS, Kang MJ, Oh YJ, Baek JW, Yang S, Hwang IT. Association of serum ferritin with insulin resistance, abdominal obesity, and metabolic syndrome in Korean adolescent and adults: The Korean National Health and Nutrition Examination Survey, 2008 to 2011. Medicine (Baltimore). 2017; 96:e6179. PMID: 28225503.10. Ryoo JH, Kim SY, Oh CM, et al. The incidental relationship between serum ferritin levels and hypertension. Int J Cardiol. 2015; 15:258–262.
Article11. Akter S, Nanri A, Kuwahara K, et al. Circulating ferritin concentrations and risk of type 2 diabetes in Japanese individuals. J Diabetes Investig. 2017; 8:462–470.
Article12. Williams MJ, Poulton R, Williams S. Relationship of serum ferritin with cardiovascular risk factors and inflammation in young men and women. Atherosclerosis. 2002; 165:179–184. PMID: 12208485.
Article13. Lim JS, Seo JH, Kim DH, Lee JA. The hemoglobin values of Korean adolescents show distinctive characteristics in comparison to those of Caucasians and African Americans. Pediatr Blood Cancer. 2015; 62:409–413. PMID: 25464505.
Article14. Zacharski LR, Ornstein DL, Woloshin S, Schwartz LM. Association of age, sex, and race with body iron stores in adults: analysis of NHANES III data. Am Heart J. 2000; 140:98–104. PMID: 10874269.
Article15. Ueno Y, Fujita K, Takashina N, et al. Studies on the change in the levels of serum ferritin, serum iron and total iron binding capacity caused by aging and sex difference. Rinsho Byori. 1991; 39:523–530. PMID: 2072576.16. Chełchowska M, Laskowska-Klita T, Leibschang J. Concentration of ferritin, transferrin and iron as a markers of iron deficiency in healthy women in reproductive age. Pol Merkur Lekarski. 2007; 22:25–27. PMID: 17477085.17. Custer EM, Finch CA, Sobel RE, Zettner A. Population norms for serum ferritin. J Lab Clin Med. 1995; 126:88–94. PMID: 7602240.18. Milman N, Clausen J, Byg KE. Iron status in 268 Danish women aged 18-30 years: influence of menstruation, contraceptive method, and iron supplementation. Ann Hematol. 1998; 77:13–19. PMID: 9760147.
Article19. Hughes K. Serum ferritin and iron status in the general population of Singapore, 1993 to 1995. Ann Acad Med Singapore. 1998; 27:507–511. PMID: 9791655.20. Milman N, Backer V, Laursen EM, Graudal N, Ibsen KK, Jordal R. Serum ferritin in children and adolescents. Results from population surveys in 1979 and 1986 comprising 1312 individuals. Eur J Haematol. 1994; 53:16–20. PMID: 8062893.
Article21. Rushton DH, Barth JH. What is the evidence for gender differences in ferritin and haemoglobin? Crit Rev Oncol Hematol. 2010; 73:1–9. PMID: 19394859.
Article22. Wang L, Huang J, Li H, et al. Distribution of iron status among urban Chinese women. Asia Pac J Clin Nutr. 2016; 25:150–157. PMID: 26965774.23. Milman N. Serum ferritin in Danes: studies of iron status from infancy to old age, during blood donation and pregnancy. Int J Hematol. 1996; 63:103–135. PMID: 8867722.24. Lee JA, Hwang JS, Hwang IT, Kim DH, Seo JH, Lim JS. Low vitamin D levels are associated with both iron deficiency and anemia in children and adolescents. Pediatr Hematol Oncol. 2015; 32:99–108. PMID: 25551430.
Article25. Nemeth E, Tuttle MS, Powelson J, et al. Hepcidin regulates cellular iron efflux by binding to ferroportin and inducing its internalization. Science. 2004; 306:2090–2093. PMID: 15514116.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Long-Term Plasmapheresis on the Iron Status of the Donors
- Variables in the Whole Cow's Milk Intake, that Impact upon the Iron Status in Early Childhood
- A Study on the Serologic Parameters in Petients with Anemia of Chronic Renal Failure-According to Erythropoietin Treatment
- The usefulness of soluble transferrin receptor in the diagnosis and treatment of iron deficiency anemia in children
- Evaluation of the Iron Status in the Adolescents in Seoul