Korean J Radiol.
2018 Aug;19(4):724-732. 10.3348/kjr.2018.19.4.724.
Efficacy, Efficiency, and Safety of Magnetic Resonance-Guided High-Intensity Focused Ultrasound for Ablation of Uterine Fibroids: Comparison with Ultrasound-Guided Method
- Affiliations
-
- 1The Institute of Ultrasound Engineering in Medicine, Chongqing Medical University, Chongqing 400016, China. yhxu_paper@sina.cn
- 2Department of Imaging and Interventional Radiology, Zhongshan-Xuhui Hospital of Fudan University, Shanghai 200031, China.
- KMID: 2413701
- DOI: http://doi.org/10.3348/kjr.2018.19.4.724
Abstract
OBJECTIVE
The purpose of this study was to compare efficacy, sonication energy efficiency, treatment time and safety of magnetic resonance-guided high-intensity focused ultrasound (MRgHIFU) and those of ultrasound-guided high-intensity focused ultrasound (USgHIFU) for ablation of uterine fibroids.
MATERIALS AND METHODS
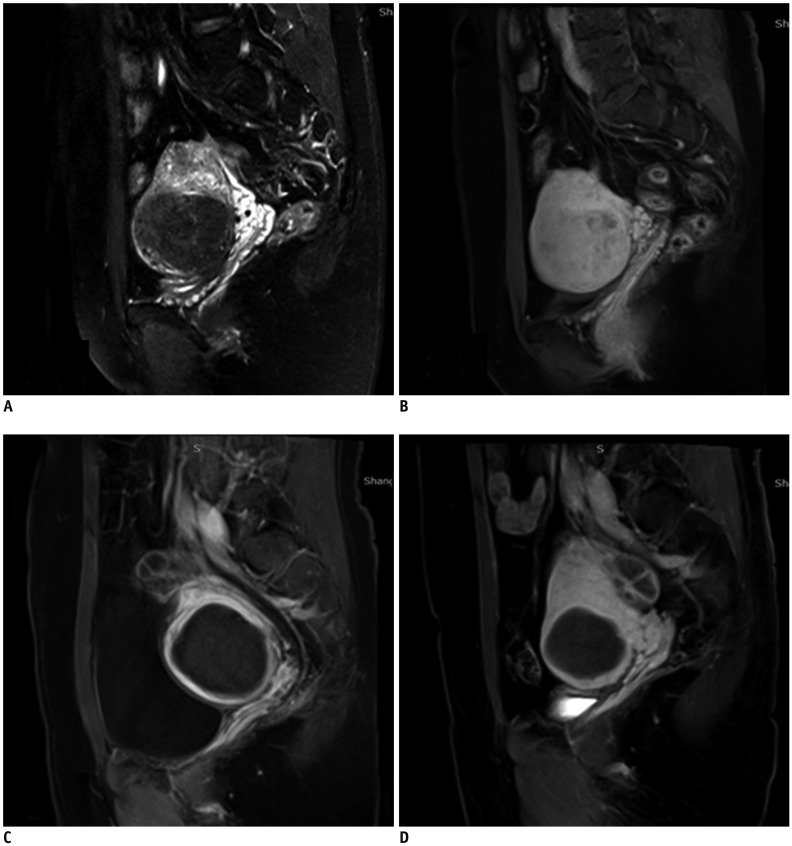
This study included 43 patients with 44 symptomatic uterine fibroids treated with MRgHIFU and 51 patients with 68 symptomatic uterine fibroids treated with USgHIFU. After therapy, contrast-enhanced MRI was conducted and complete ablation was defined as 100% non-perfused volume (NPV) of fibroids. Patients with completely ablated fibroids were selected for the comparison of the treatment data and sonication parameters between MRgHIFU and USgHIFU treated groups.
RESULTS
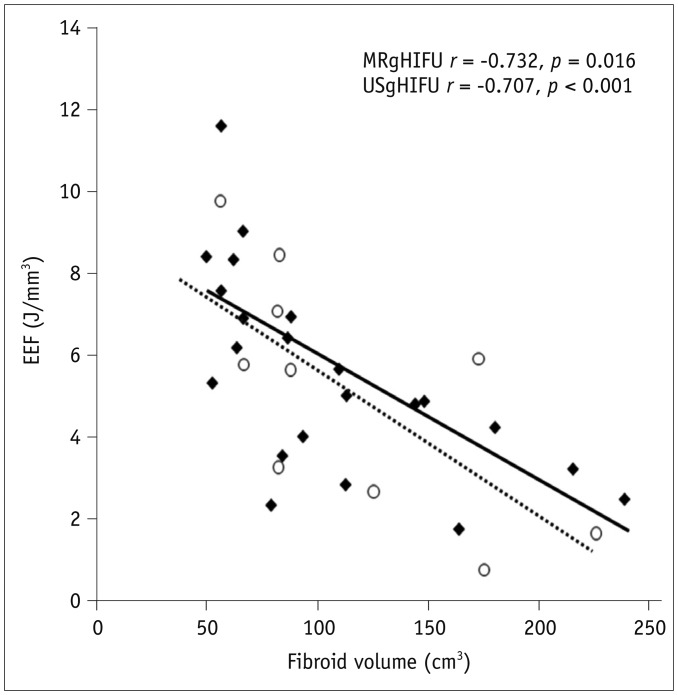
Thirteen completely ablated fibroids in 10 patients (23.3%, 10/43) were achieved with MRgHIFU and 28 completely ablated fibroids in 22 patients (43.1%, 22/51) were achieved with USgHIFU. In completely ablated fibroids, the energy-efficiency factor (EEF) was 5.1 ± 3.0 J/mm3 and 4.7 ± 2.5 J/mm3 in the MRgHIFU and USgHIFU, respectively (p = 0.165). There was a negative linear correlation between EEF and the NPV of fibroids for MRgHIFU (p = 0.016) and USgHIFU (p = 0.001). The mean treatment time was 174.5 ± 42.2 minutes and 114.4 ± 39.2 minutes in the MRgHIFU and USgHIFU procedures, respectively (p = 0.021). There were no severe adverse events and major complications after treatment.
CONCLUSION
MRgHIFU and USgHIFU are safe and effective with the equivalent energy efficiency for complete ablation of fibroids. USgHIFU has shorter treatment time than MRgHIFU.
MeSH Terms
Figure
Reference
-
1. Xu Y, Fu Z, Yang L, Huang Z, Chen WZ, Wang Z. Feasibility, safety, and efficacy of accurate uterine fibroid ablation using magnetic resonance imaging-guided high-intensity focused ultrasound with shot sonication. J Ultrasound Med. 2015; 34:2293–2303. PMID: 26518278.
Article2. Orsi F, Arnone P, Chen W, Zhang L. High intensity focused ultrasound ablation: a new therapeutic option for solid tumors. J Cancer Res Ther. 2010; 6:414–420. PMID: 21358073.3. Jolesz FA, Hynynen K, McDannold N, Freundlich D, Kopelman D. Noninvasive thermal ablation of hepatocellular carcinoma by using magnetic resonance imaging-guided focused ultrasound. Gastroenterology. 2004; 127(5 Suppl 1):S242–S247. PMID: 15508090.
Article4. Zhang L, Chen WZ, Liu YJ, Hu X, Zhou K, Chen L, et al. Feasibility of magnetic resonance imaging-guided high intensity focused ultrasound therapy for ablating uterine fibroids in patients with bowel lies anterior to uterus. Eur J Radiol. 2010; 73:396–403. PMID: 19108974.
Article5. Pron G. Magnetic resonance-guided high-intensity focused ultrasound (MRgHIFU) treatment of symptomatic uterine fibroids: an evidence-based analysis. Ont Health Technol Assess Ser. 2015; 15:1–86.6. Yu T, Luo J. Adverse events of extracorporeal ultrasound-guided high intensity focused ultrasound therapy. PLoS One. 2011; 6:e26110. PMID: 22194777.
Article7. McDannold N, Tempany CM, Fennessy FM, So MJ, Rybicki FJ, Stewart EA, et al. Uterine leiomyomas: MR imaging-based thermometry and thermal dosimetry during focused ultrasound thermal ablation. Radiology. 2006; 240:263–272. PMID: 16793983.
Article8. Stewart EA, Gedroyc WM, Tempany CM, Quade BJ, Inbar Y, Ehrenstein T, et al. Focused ultrasound treatment of uterine fibroid tumors: safety and feasibility of a noninvasive thermoablative technique. Am J Obstet Gynecol. 2003; 189:48–54. PMID: 12861137.
Article9. Li F, Wang Z, Du Y, Ma P, Bai J, Wu F, et al. [Study on therapeutic dosimetry of HIFU ablation tissue]. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi. 2006; 23:839–843. PMID: 17002121.10. Chen J, Li Y, Wang Z, McCulloch P, Hu L, Chen W, et al. Committee of the Clinical Trial of HIFU versus Surgical Treatment for Fibroids. Evaluation of high-intensity focused ultrasound ablation for uterine fibroids: an IDEAL prospective exploration study. BJOG. 2018; 125:354–364. PMID: 28421665.
Article11. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol. 2003; 14(9 Pt 2):S199–S202. PMID: 14514818.
Article12. Kajiyama K, Yoshinaka K, Takagi S, Matsumoto Y. Micro-bubble enhanced HIFU. Physics Procedia. 2010; 3:305–314.
Article13. Lynn JG, Zwemer RL, Chick AJ, Miller AE. A new method for the generation and use of focused ultrasound in experimental biology. J Gen Physiol. 1942; 26:179–193. PMID: 19873337.
Article14. Chen W, Zhu H, Zhang L, Li K, Su H, Jin C, et al. Primary bone malignancy: effective treatment with high-intensity focused ultrasound ablation. Radiology. 2010; 255:967–978. PMID: 20501734.
Article15. Venkatesan AM, Partanen A, Pulanic TK, Dreher MR, Fischer J, Zurawin RK, et al. Magnetic resonance imaging-guided volumetric ablation of symptomatic leiomyomata: correlation of imaging with histology. J Vasc Interv Radiol. 2012; 23:786–794.e4. PMID: 22626269.
Article16. Idée JM, Port M, Robic C, Medina C, Sabatou M, Corot C. Role of thermodynamic and kinetic parameters in gadolinium chelate stability. J Magn Reson Imaging. 2009; 30:1249–1258. PMID: 19938037.17. Aime S, Caravan P. Biodistribution of gadolinium-based contrast agents, including gadolinium deposition. J Magn Reson Imaging. 2009; 30:1259–1267. PMID: 19938038.
Article18. Trumm CG, Stahl R, Clevert DA, Herzog P, Mindjuk I, Kornprobst S, et al. Magnetic resonance imaging-guided focused ultrasound treatment of symptomatic uterine fibroids: impact of technology advancement on ablation volumes in 115 patients. Invest Radiol. 2013; 48:359–365. PMID: 23385396.19. Hindley J, Gedroyc WM, Regan L, Stewart E, Tempany C, Hynyen K, et al. MRI guidance of focused ultrasound therapy of uterine fibroids: early results. AJR Am J Roentgenol. 2004; 183:1713–1719. PMID: 15547216.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expulsion of Fibroids to the Endometrial Cavity after Magnetic Resonance Imaging-guided High Intensity Focused Ultrasound Surgery (MRgFUS) Treatment of Intramural Uterine Fibroids
- Clinical application of high-intensity focused ultrasound ablation for uterine fibroids
- Clinical Consideration of Treatment to Ablate Uterine Fibroids with Magnetic Resonance Imaging-guided High Intensity Focused Ultrasound (MRgFUS): Sonalleve
- Usefulness of modified BRB technique in treatment to ablate uterine fibroids with magnetic resonance image-guided high-intensity focused ultrasound
- Current status of high-intensity focused ultrasound for the management of uterine adenomyosis