J Rhinol.
2018 May;25(1):7-13. 10.18787/jr.2018.25.1.7.
Recent Trends of Prevalence in Unilateral Sinusitis and Useful Factors in Differential Diagnosis
- Affiliations
-
- 1Department of Otorhinolaryngology-Head and Neck Surgery, Dankook University, College of Medicine, Cheonan, Korea. entdocjung@hanmail.net
- KMID: 2412914
- DOI: http://doi.org/10.18787/jr.2018.25.1.7
Abstract
- BACKGROUND AND OBJECTIVES
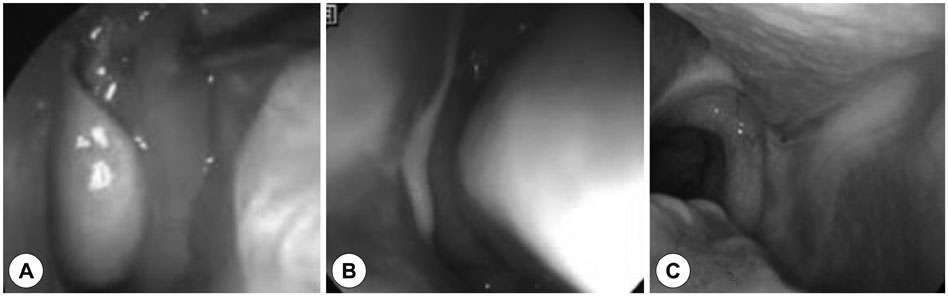
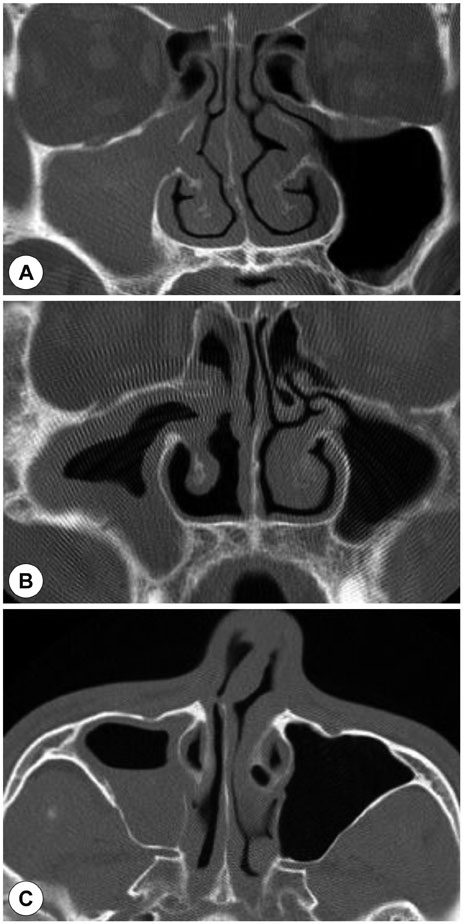
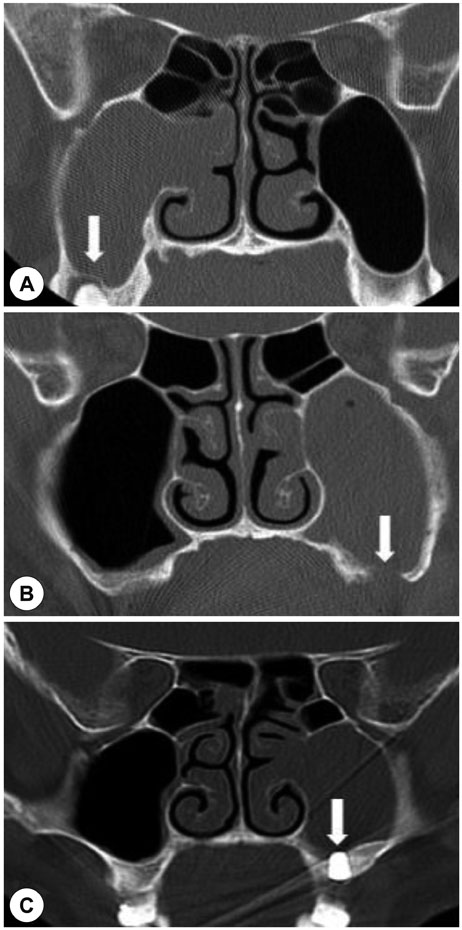
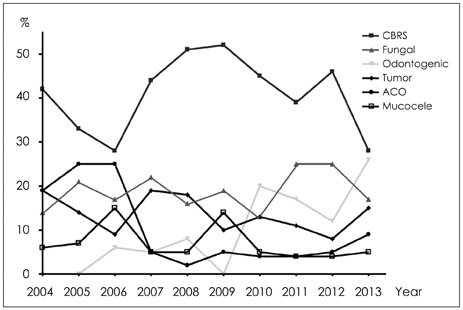
Unilateral sinus lesions can be caused by many diseases and exact preoperative diagnosis is often difficult to make. The aims of this study were to evaluate the recent trends for prevalence of unilateral sinus lesions and find useful factors in differential diagnosis. MATERIALS AND METHOD: Preoperative clinical diagnosis including computed tomography (CT) images, endoscopic findings and postoperative diagnosis based on pathology were assessed retrospectively in 384 consecutive patients who underwent unilateral sinus surgery from 2004 to 2013.
RESULTS
Chronic bacterial rhinosinusitis (40%) was the most common cause of unilateral sinus lesions, followed by fungal sinusitis (21%), benign and malignant tumors (14%), and odontogenic sinusitis (11%). The incidence of odontogenic sinusitis has recently increased and mismatches of pre- and post-operative diagnosis were commonly found among patients with chronic bacterial rhinosinusitis, fungal sinusitis, or odontogenic sinusitis. Microcalcification in fungal sinusitis and dental lesions in odontogenic sinusitis were confirmed as critical factors by logistic regression analysis.
CONCLUSION
The incidence of odontogenic sinusitis has been increasing steadily over the last 10 years. The findings of microcalcification and dental lesions on CT could provide crucial information to make a precise preoperative diagnosis among chronic bacterial rhinosinusitis, fungal sinusitis and odontogenic sinusitis.
Keyword
MeSH Terms
Figure
Reference
-
1. Chen HJ, Chen HS, Chang YL, Huang YC. Complete unilateral maxillary sinus opacity in computed tomography. J Formos Med Assoc. 2010; 109(10):709–715.
Article2. Ikeda K, Tanno N, Suzuki H, Oshima T, Kano S, Takasaka T. Unilateral sinonasal disease without bone destruction. Differential diagnosis using diagnostic imaging and endonasal endoscopic biopsy. Arch Otolaryngol Head Neck Surg. 1997; 123(2):198–200.
Article3. Joshua BZ, Sachs O, Shelef I, Vardy-Sion N, Novack L, Vaiman M, et al. Comparison of clinical data, CT, and bone histopathology in unilateral chronic maxillary sinusitis. Otolaryngol Head Neck Surg. 2013; 148(1):145–150.
Article4. Patel NA, Ferguson BJ. Odontogenic sinusitis: an ancient but under-appreciated cause of maxillary sinusitis. Curr Opin Otolaryngol Head Neck Surg. 2012; 20(1):24–28.5. Wang ZM, Kanoh N, Dai CF, Kutler DI, Xu R, Chi FL, et al. Isolated sphenoid sinus disease: an analysis of 122 cases. Ann Otol Rhinol Laryngol. 2002; 111(4):323–327.
Article6. Lee TJ, Huang SF, Chang PH. Characteristics of isolated sphenoid sinus aspergilloma: report of twelve cases and literature review. Ann Otol Rhinol Laryngol. 2009; 118(3):211–217.
Article7. Lee JY, Byun JY, Shim SS, Lee SW. Outcomes after endoscopic sinus surgery for unilateral versus bilateral chronic rhinosinusitis with nasal polyposis. Am J Rhinol Allergy. 2010; 24(3):83–86.
Article8. Grosjean P, Weber R. Fungus balls of the paranasal sinuses: a review. Eur Arch Otorhinolaryngol. 2007; 264(5):461–470.
Article9. Jeong JH, Kim KT, Chung SK. The Role of Otolaryngology in Dental Implantation. J Rhinol. 2008; 15(2):83–91.10. Ma Z, Yang X. Research on misdiagnosis of space occupying lesions in unilateral nasal sinus. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2012; 26(2):59–61.11. Ugincius P, Kubilius R, Gervickas A, Vaitkus S. Chronic odontogenic maxillary sinusitis. Stomatologija. 2006; 8(2):44–48.12. Mehra P, Murad H. Maxillary sinus disease of odontogenic origin. Otolaryngol Clin North Am. 2004; 37(2):347–364.
Article13. Lee JS, Shin SY, Lee KH, Kim SW, Cho JS. Change of prevalence and clinical aspects of fungal ball according to temporal difference. Eur Arch Otorhinolaryngol. 2013; 270(5):1673–1677.
Article14. Yeo CK, Ahn BH, Kim JS, Kim YD, Shin SH, Ye MK. Fungal Ball in Sinus: Multi-Center Study in Daegu. J Rhinol. 2005; 12(2):105–107.15. Milonski J, Zielinska-Blizniewska H, Pietkiewicz P, Olszewski J. Analysis of histopathological evaluation of pathological lesions removed by endoscopic surgery of the nose and paranasal sinuses in the own material. Otolaryngol Pol. 2011; 65(6):447–450.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical significance of unilateral sinusitis
- Anatomical Factors Influencing Unilateral Chronic Sinusitis
- Analysis of Treatment Outcome Associated with Pre-Operative Diagnostic Accuracy Changes and Dental Treatment Timing in Odontogenic Sinusitis Involving Unilateral Maxillary Sinus
- Differential Diagnosis of Fungal and Nonfungal Infection of the Pa ranasal Sinuses Using CT: Value of Intralesional Expansile Ball-like High Density
- The management of sinusitis in children