Korean J Ophthalmol.
2018 Jun;32(3):182-189. 10.3341/kjo.2017.0072.
Time Series Changes in Cataract Surgery in Korea
- Affiliations
-
- 1The Bom Eye Clinic, Busan, Korea.
- 2Department of Ophthalmology, Kosin University College of Medicine, Busan, Korea. hhiatus@gmail.com
- 3Institute for Medicine, Kosin University, Busan, Korea.
- KMID: 2412796
- DOI: http://doi.org/10.3341/kjo.2017.0072
Abstract
- PURPOSE
We analyzed time series changes in cataract surgeries in Korea, and provide basic data to enhance the efficiency of medical services for cataract surgery.
METHODS
Among cataract surgery statistics registered in the Korean National Health Insurance Cooperation from 2006 to 2012, we used data regarding the number of patients and operations and the number of patients and operations per 100,000 people. We analyzed various time series changes, including differences by sex and age.
RESULTS
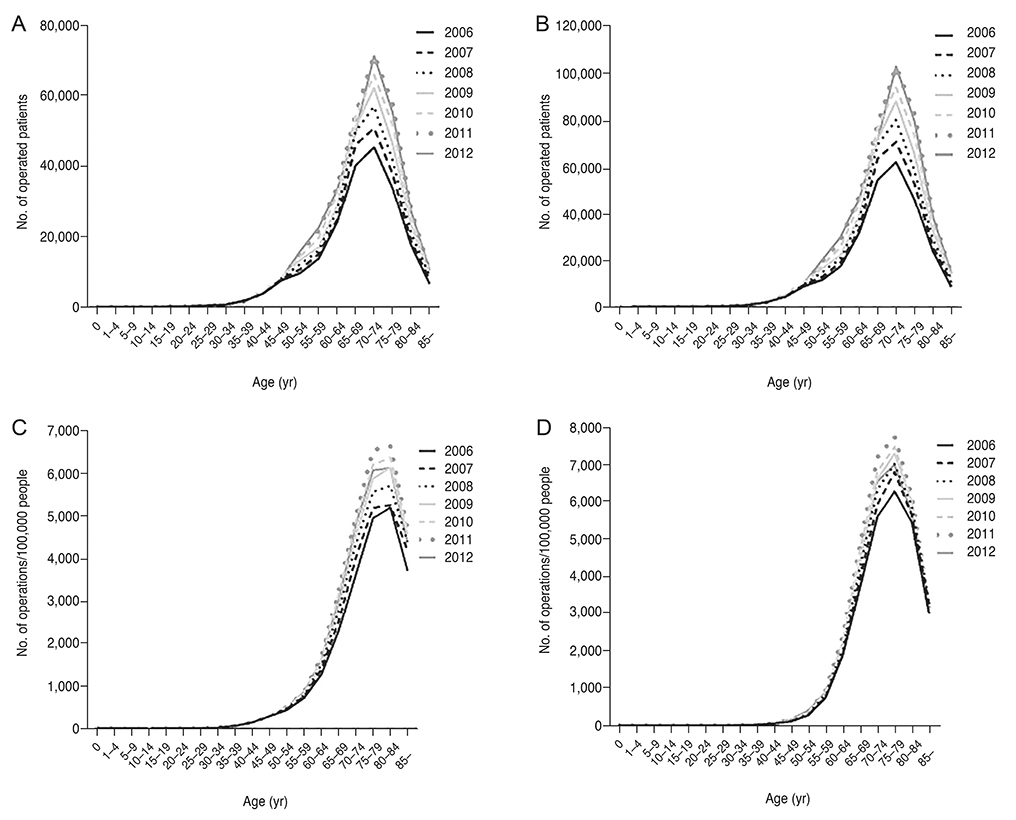
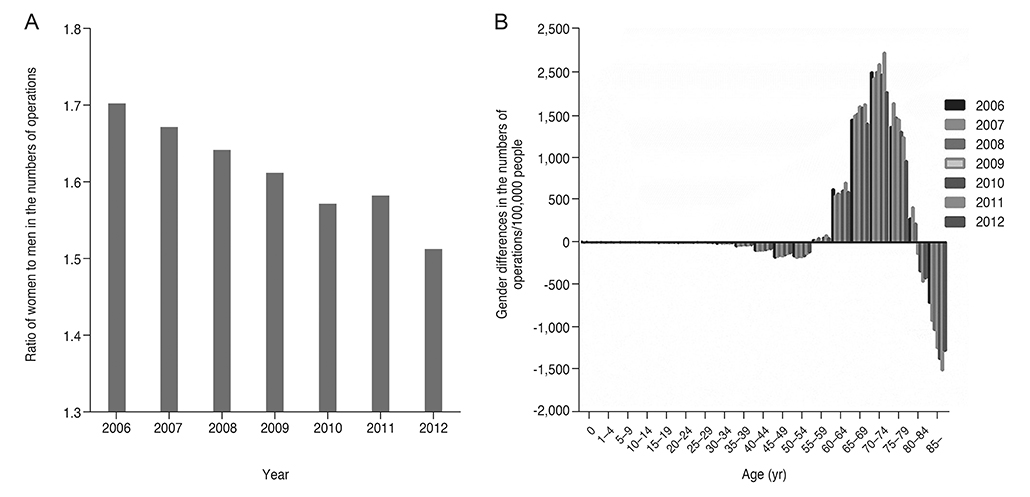
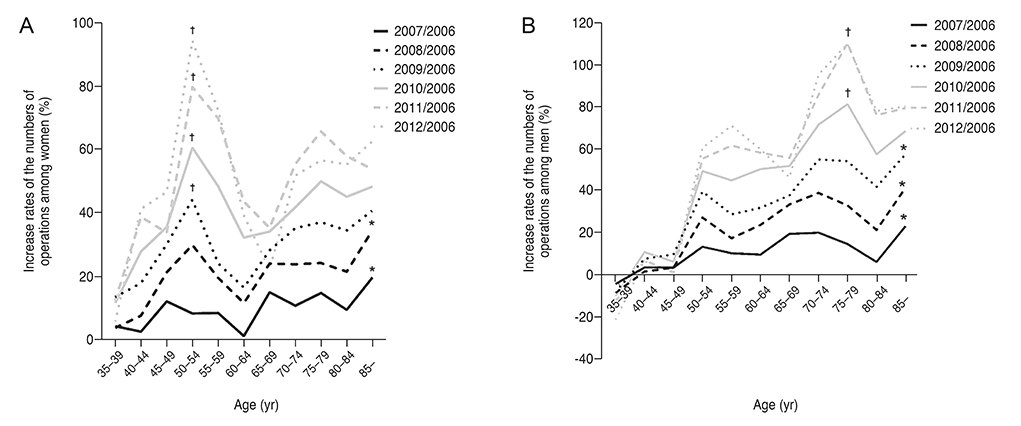
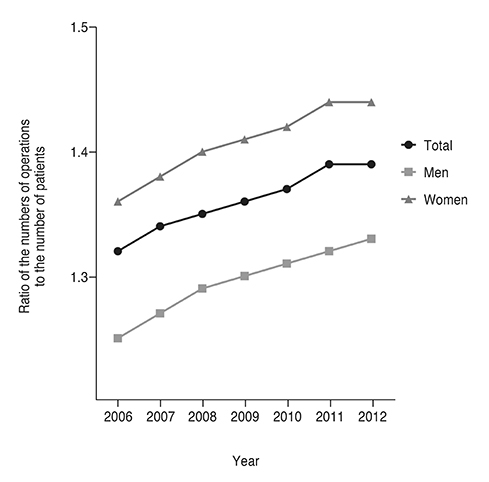
The total numbers of patients from 2006 to 2012 by year were 207,370; 228,170; 250,289; 268,548; 289,867; 308,111; and 302,182, respectively. The total numbers of operations from 2006 to 2012 by year were 272,920; 305,807; 338,332; 365,874; 398,338; 428,158; and 420,905, respectively. The number of patients and operations per 100,000 people were highest in men 80 to 84 years old and women 75 to 79 years old. Comparing the number of operations in 2006 and after, the patient age group with the highest increase rate changed from over 85 years old to 75-79 years old since 2010 in men and from over 85 years old to 50-54 years old since 2009 in women. For each year investigated, the number of operations performed was higher than the number of patients who received operations.
CONCLUSIONS
Over the study period, the number of cataract surgeries increased, while the age of cataract patients decreased. Additionally, the number of cataract-related surgeries increased in relation to the number of patients.
Keyword
Figure
Reference
-
1. Resnikoff S, Pascolini D, Etya'ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004; 82:844–851.2. World Health Organization. Prevention of blindness and deafness: global initiative for the elimination of avoidable blindness [Internet]. Geneva: World Health Organization;2000. cited 2017 Jun 9. Available from: http://apps.who.int/iris/bitstream/10665/63748/1/WHO_PBL_97.61_Rev.2.pdf.3. Taylor HR, Vu HT, Keeffe JE. Visual acuity thresholds for cataract surgery and the changing Australian population. Arch Ophthalmol. 2006; 124:1750–1753.
Article4. Behndig A, Montan P, Stenevi U, et al. One million cataract surgeries: Swedish National Cataract Register 1992–2009. J Cataract Refract Surg. 2011; 37:1539–1545.
Article5. Gollogly HE, Hodge DO, St Sauver JL, Erie JC. Increasing incidence of cataract surgery: population-based study. J Cataract Refract Surg. 2013; 39:1383–1389.
Article6. Murthy GV, Gupta S, Ellwein LB, et al. A population-based eye survey of older adults in a rural district of Rajasthan. I. Central vision impairment, blindness, and cataract surgery. Ophthalmology. 2001; 108:679–685.7. Dandona L, Dandona R, Naduvilath TJ, et al. Population-based assessment of the outcome of cataract surgery in an urban population in southern India. Am J Ophthalmol. 1999; 127:650–658.
Article8. Zhang JS, Xu L, Wang YX, et al. Five-year incidence of age-related cataract and cataract surgery in the adult population of greater Beijing: the Beijing Eye Study. Ophthalmology. 2011; 118:711–718.9. Keenan T, Rosen P, Yeates D, Goldacre M. Time trends and geographical variation in cataract surgery rates in England: study of surgical workload. Br J Ophthalmol. 2007; 91:901–904.
Article10. Lundstrom M, Stenevi U, Thorburn W. Quality of life after first- and second-eye cataract surgery: five-year data collected by the Swedish National Cataract Register. J Cataract Refract Surg. 2001; 27:1553–1559.11. Tan AC, Tay WT, Zheng YF, et al. The impact of bilateral or unilateral cataract surgery on visual functioning: when does second eye cataract surgery benefit patients? Br J Ophthalmol. 2012; 96:846–851.
Article12. Erie JC, Baratz KH, Hodge DO, et al. Incidence of cataract surgery from 1980 through 2004: 25-year population-based study. J Cataract Refract Surg. 2007; 33:1273–1277.
Article13. Rachmiel R, Trope GE, Chipman ML, Buys YM. Cataract surgery rates in Ontario, Canada, from 1992 to 2004: more surgeries with fewer ophthalmologists. Can J Ophthalmol. 2007; 42:539–542.
Article14. Rim TH, Lee DM, Chung EJ. Visual acuity and quality of life: KNHANES IV. J Korean Ophthalmol Soc. 2013; 54:46–52.
Article15. Song MH, Kim JW, Chung SK. The statistical observation of ocular injury. J Korean Ophthalmol Soc. 2009; 50:580–587.
Article16. Lee JE, Kim SY, Lee SU, Lee SJ. Epidemiological profiles of industrial ocular injuries. J Korean Ophthalmol Soc. 2013; 54:136–142.
Article17. Kim HJ, Park JW, Joo CK. An epidemiological study of the risk factors associated with anterior polar cataract. J Korean Ophthalmol Soc. 2003; 44:606–614.18. Kim H, Joo CK. The prevalence and demographic characteristics of anterior polar cataract in a hospital-based study in Korea. Korean J Ophthalmol. 2008; 22:77–80.
Article19. Rim TH, Park SY, Kim TI. Epidemiological survey regarding cataract awareness in Korea: KNHANES IV. J Korean Ophthalmol Soc. 2013; 54:72–77.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Evaluation of Traumatic Cataract with Corneal Laceration
- The Change of Astigmatism After Cataract Extraction with Double Horizontal Suture
- Comparison of Effective Phacoemulsification Time between Femtosecond Laser-Assisted Cataract Surgery and Conventional Cataract Surgery
- Iatrogenic Blepharoptosis after Cataract Surgery
- Cataract Operation: procedure and technique