Ann Surg Treat Res.
2018 Jun;94(6):291-297. 10.4174/astr.2018.94.6.291.
Single-incision laparoscopic cholecystectomy using instrumental alignment in robotic single-site cholecystectomy
- Affiliations
-
- 1Division of Hepatobiliary and Pancreas, Department of Surgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea. feel415@cha.ac.kr
- KMID: 2412398
- DOI: http://doi.org/10.4174/astr.2018.94.6.291
Abstract
- PURPOSE
There is no standardized single-incision laparoscopic cholecystectomy (SILC) technique in contrast to robot single-site cholecystectomy (RSSC). We tried to implement the array of instruments used in RSSC to SILC.
METHODS
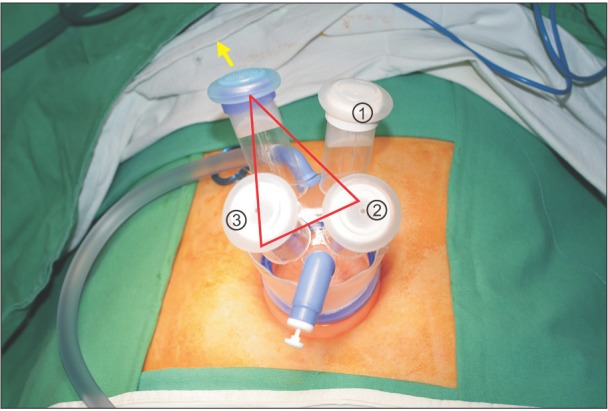
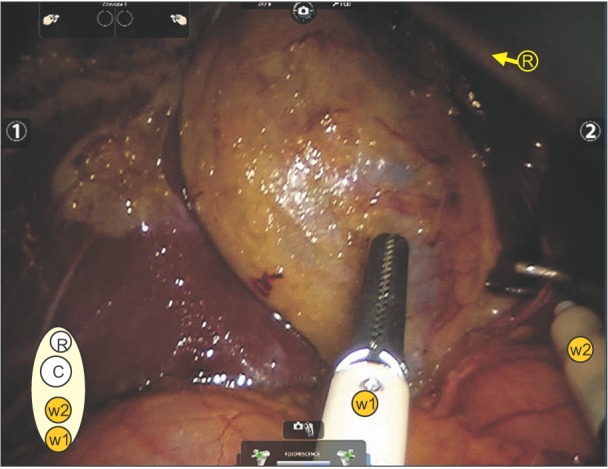
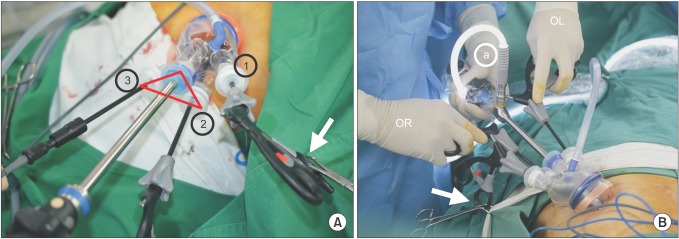
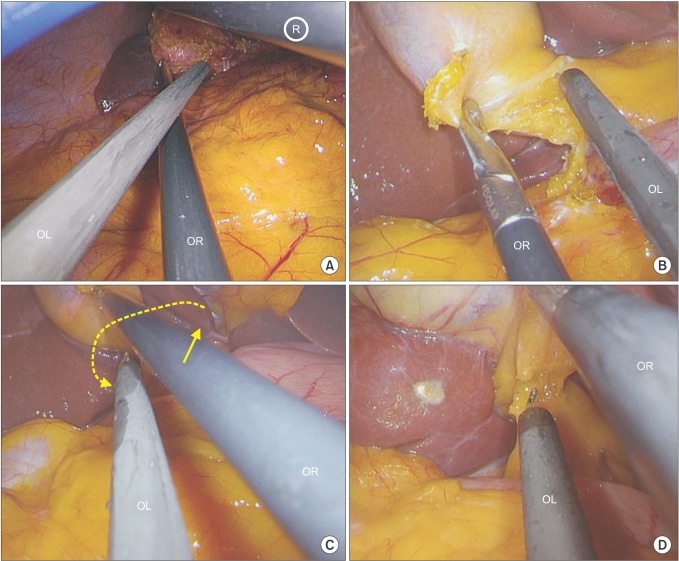
A series of 108 consecutive patients underwent SILC between September 2014 and July 2017 by 2 surgeons. The indication was benign disease of the gallbladder. The perioperative outcomes were reviewed. We used the 4-channel Glove port and conventional laparoscopic instruments.
RESULTS
The study subjects consisted of 29 males and 79 females, and the mean age was 44.4 years (range, 16-70 years). Mean body mass index was 24.1 kg/m2. The mean working time was 25.0 ± 10.7 minutes and total operation time was 44.4 ± 12.4 minutes. There were 7 cases of conversion (additional 1 port in 4 patients, additional 2 ports in 2, and conventional 4 port technique in 1). Bile spillage from the gallbladder during the procedure occurred in 17 (15.7%). There were no postoperative complications. Postoperative hospital stay was 2.0 ± 0.6 days.
CONCLUSION
The alignment of the instruments in a RSSC was successfully implemented into a SILC, so that an equally effective operation was possible.
MeSH Terms
Figure
Reference
-
1. Evers L, Bouvy N, Branje D, Peeters A. Single-incision laparoscopic cholecystectomy versus conventional four-port laparoscopic cholecystectomy: a systematic review and meta-analysis. Surg Endosc. 2017; 31:3437–3448. PMID: 28039641.
Article2. Sajid MS, Ladwa N, Kalra L, Hutson KK, Singh KK, Sayegh M. Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: meta-analysis and systematic review of randomized controlled trials. World J Surg. 2012; 36:2644–2653. PMID: 22855214.
Article3. Haueter R, Schutz T, Raptis DA, Clavien PA, Zuber M. Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg. 2017; 104:1141–1159. PMID: 28569406.
Article4. Bucher P, Pugin F, Buchs N, Ostermann S, Charara F, Morel P. Single port access laparoscopic cholecystectomy (with video). World J Surg. 2009; 33:1015–1019. PMID: 19116734.
Article5. Choi SH, Hwang HK, Kang CM, Lee WJ. Single-fulcrum laparoscopic cholecystectomy: a single-incision and multi-port technique. ANZ J Surg. 2012; 82:529–534. PMID: 22776541.
Article6. Duron VP, Nicastri GR, Gill PS. Novel technique for a single-incision laparoscopic surgery (SILS) approach to cholecystectomy: single-institution case series. Surg Endosc. 2011; 25:1666–1671. PMID: 21057963.
Article7. Wakasugi M, Tei M, Omori T, Anno K, Mikami T, Tsukada R, et al. Single-incision laparoscopic surgery as a teaching procedure: a single-center experience of more than 2100 procedures. Surg Today. 2016; 46:1318–1324. PMID: 26922213.
Article8. Vyas D, Weiner C, Vyas AK. Current status of single-site robotic cholecystectomy, its feasibility, economic and overall impact. Am J Robot Surg. 2014; 1:1–64.
Article9. Ko JW, Lee JW, Kwon SW, Choi SH. Advantages of the glove port docking technique in robotic single-site cholecystectomy: comparison with the conventional silicone port. J Robot Surg. 2017; 9. 21. DOI: 10.1007/s11701-017-0754-5. [Epub].
Article10. Yokoe M, Takada T, Strasberg SM, Solomkin JS, Mayumi T, Gomi H, et al. TG13 diagnostic criteria and severity grading of acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. 2013; 20:35–46. PMID: 23340953.
Article11. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009; 250:187–196. PMID: 19638912.12. Strasberg SM, Linehan DC, Hawkins WG. The accordion severity grading system of surgical complications. Ann Surg. 2009; 250:177–186. PMID: 19638919.
Article13. Choi SH, Hwang HK, Kang CM, Lee WJ. Transumbilical single port laparoscopic adrenalectomy: a technical report on right and left adrenalectomy using the glove port. Yonsei Med J. 2012; 53:442–445. PMID: 22318837.
Article14. Abe N, Takeuchi H, Ohki A, Aoki H, Masaki T, Mori T, et al. Single-incision multiport laparoendoscopic surgery using a newly developed short-type flexible endoscope: a combined procedure of flexible endoscopic and laparoscopic surgery. J Hepatobiliary Pancreat Sci. 2012; 19:426–430. PMID: 21927879.
Article15. Allemann P, Schafer M, Demartines N. Critical appraisal of single port access cholecystectomy. Br J Surg. 2010; 97:1476–1480. PMID: 20641051.
Article16. Bhandarkar D, Mittal G, Shah R, Katara A, Udwadia TE. Single-incision laparoscopic cholecystectomy: How I do it? J Minim Access Surg. 2011; 7:17–23. PMID: 21197237.
Article17. Kuon Lee S, You YK, Park JH, Kim HJ, Lee KK, Kim DG. Single-port transumbilical laparoscopic cholecystectomy: a preliminary study in 37 patients with gallbladder disease. J Laparoendosc Adv Surg Tech A. 2009; 19:495–499. PMID: 19630589.
Article18. Ryu YB, Lee JW, Park YH, Lim MS, Cho JW, Jeon JY. One-year experience with single incision laparoscopic cholecystectomy in a single center: without the use of inverse triangulation. Ann Surg Treat Res. 2016; 90:72–78. PMID: 26878014.
Article19. Angus AA, Sahi SL, McIntosh BB. Learning curve and early clinical outcomes for a robotic surgery novice performing robotic single site cholecystectomy. Int J Med Robot. 2014; 10:203–207. PMID: 24030910.
Article20. Buzad FA, Corne LM, Brown TC, Fagin RS, Hebert AE, Kaczmarek CA, et al. Single-site robotic cholecystectomy: efficiency and cost analysis. Int J Med Robot. 2013; 9:365–370. PMID: 23640914.
Article21. Lee H, Lee DH, Kim H, Han Y, Kim SW, Jang JY. Single-incision robotic cholecystectomy: a special emphasis on utilization of transparent glove ports to overcome limitations of single-site port. Int J Med Robot. 2017; 13.
Article22. Konstantinidis KM, Hirides P, Hirides S, Chrysocheris P, Georgiou M. Cholecystectomy using a novel Single-Site(®) robotic platform: early experience from 45 consecutive cases. Surg Endosc. 2012; 26:2687–2694. PMID: 22476831.
Article23. Kiriyama S, Takada T, Hwang TL, Akazawa K, Miura F, Gomi H, et al. Clinical application and verification of the TG13 diagnostic and severity grading criteria for acute cholangitis: an international multicenter observational study. J Hepatobiliary Pancreat Sci. 2017; 24:329–337. PMID: 28419764.
Article24. Romanelli JR, Earle DB. Single-port laparoscopic surgery: an overview. Surg Endosc. 2009; 23:1419–1427. PMID: 19347400.
Article25. Erbella J Jr, Bunch GM. Single-incision laparoscopic cholecystectomy: the first 100 outpatients. Surg Endosc. 2010; 24:1958–1961. PMID: 20112110.
Article26. Rivas H, Varela E, Scott D. Single-incision laparoscopic cholecystectomy: initial evaluation of a large series of patients. Surg Endosc. 2010; 24:1403–1412. PMID: 20035355.
Article27. Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endosc. 2015; 29:3074–3085. PMID: 25669635.
Article28. Hall TC, Dennison AR, Bilku DK, Metcalfe MS, Garcea G. Single-incision laparoscopic cholecystectomy: a systematic review. Arch Surg. 2012; 147:657–666. PMID: 22802063.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Single-Incision Robotic Cholecystectomy, Single-Incision Laparoscopic Cholecystectomy and 3-Port Laparoscopic Cholecystectomy -Postoperative Pain, Cosmetic Outcome and Surgeon's Workload
- Single incision laparoscopic cholecystectomy for patients with Mirizzi syndrome
- Comparison of outcomes of single incision robotic cholecystectomy and single incision laparoscopic cholecystectomy
- Single-incision Robotic Cholecystectomy: Initial Experience and Results
- Minimally Invasive Single-Site Cholecystectomy in Obese Patients: Laparoscopic vs. Robotic