Chonnam Med J.
2018 May;54(2):121-128. 10.4068/cmj.2018.54.2.121.
Effects of Bisoprolol Are Comparable with Carvedilol in Secondary Prevention of Acute Myocardial Infarction in Patients Undergoing Percutaneous Coronary Intervention
- Affiliations
-
- 1Department of Cardiology, Gunsan Medical Center, Gunsan, Korea.
- 2Department of Cardiology, Cheomdan Medical Center, Gwangju, Korea.
- 3Department of Cardiology, Chonnam National University Hospital, Gwangju, Korea. cecilyk@hanmail.net
- 4Department of Cardiology, Chungbuk National University Hospital, Cheongju, Korea.
- 5Department of Cardiology, Chunbuk National University Hospital, Jeonju, Korea.
- 6Department of Cardiology, Kyungpook National University Hospital, Daegu, Korea.
- 7Department of Cardiology, Yeungnam University Hospital, Daegu, Korea.
- KMID: 2411895
- DOI: http://doi.org/10.4068/cmj.2018.54.2.121
Abstract
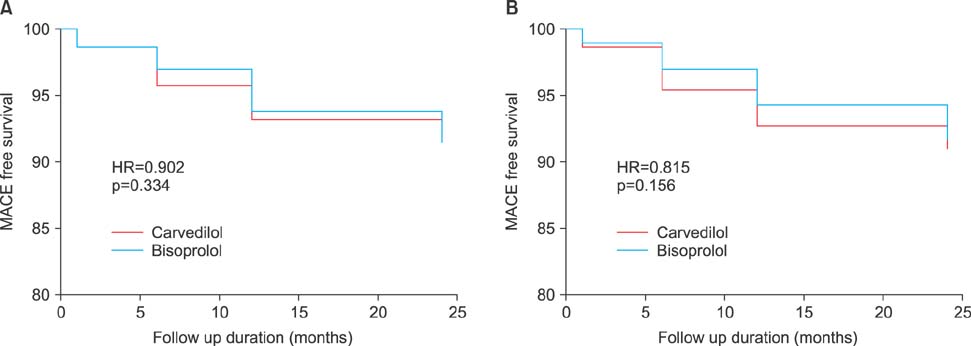
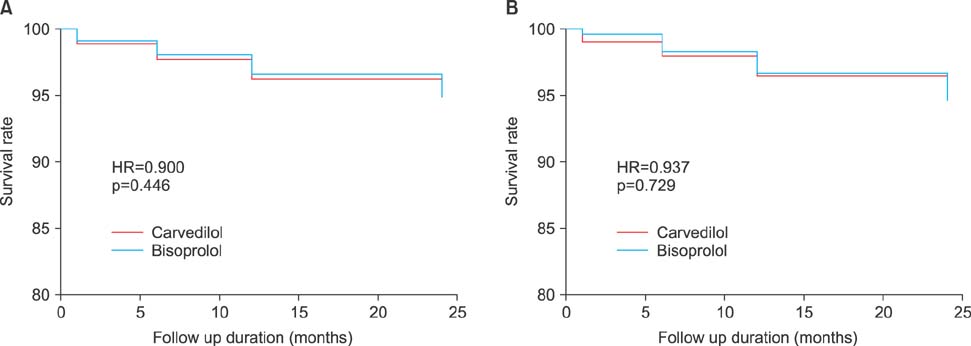
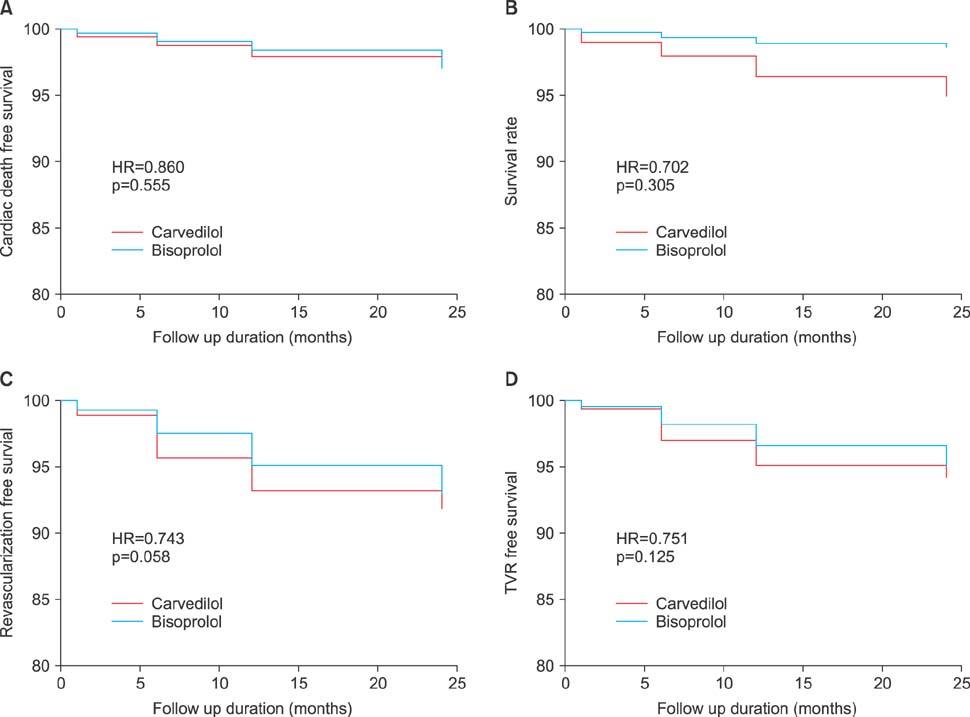
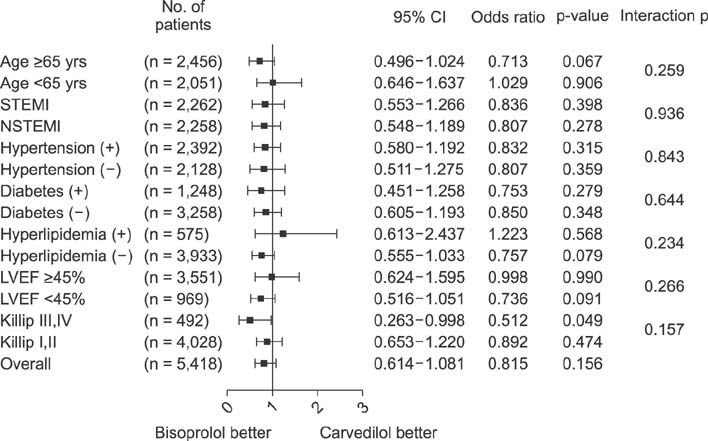
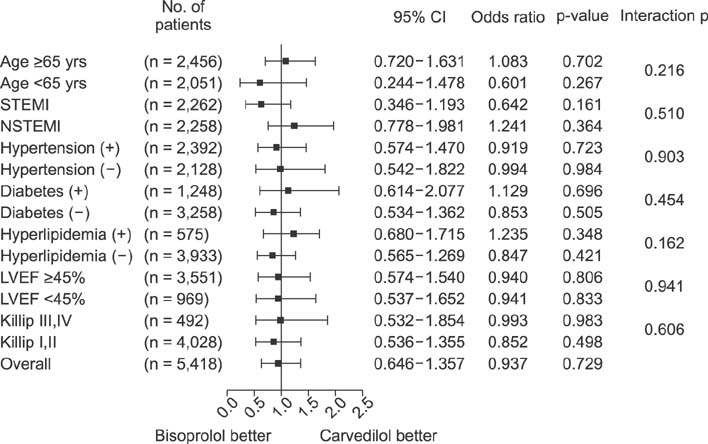
- Although the benefits of carvedilol have been demonstrated in the era of percutaneous coronary intervention (PCI), very few studies have evaluated the efficacy of bisoprolol in the secondary prevention of acute myocardial infarction (MI) in patients treated with PCI. We hypothesized that the effect of bisoprolol would not be different from carvedilol in post-MI patients. A total of 13,813 patients who underwent PCI were treated either with carvedilol or bisoprolol at the time of discharge. They were enrolled from the Korean Acute MI Registry (KAMIR). After 1:2 propensity score matching, 1,806 patients were enrolled in the bisoprolol group and 3,612 patients in the carvedilol group. The primary end point was the composite of major adverse cardiac events (MACEs), which was defined as cardiac death, nonfatal MI, target vessel revascularization, and coronary artery bypass surgery. The secondary end point was defined as all-cause mortality, cardiac death, nonfatal MI, any revascularization, or target vessel revascularization. After adjustment for differences in baseline characteristics by propensity score matching, the MACE-free survival rate was not different between the groups (HR=0.815, 95% CI:0.614-1.081, p=0.156). In the subgroup analysis, the cumulative incidence of MACEs was lower in the bisoprolol group in patients having a Killip class of III or IV than in the carvedilol group (HR=0.512, 95% CI: 0.263-0.998, p=0.049). The incidence of secondary end points was similar between the two beta-blocker groups. In conclusion, the benefits of bisoprolol were comparable with those of carvedilol in the secondary prevention of acute MI.
Keyword
MeSH Terms
Figure
Reference
-
1. A randomized trial of propranolol in patients with acute myocardial infarction. I. Mortality results. JAMA. 1982; 247:1707–1714.2. A randomized trial of propranolol in patients with acute myocardial infarction. II. Morbidity results. JAMA. 1983; 250:2814–2819.3. Norwegian Multicenter Study Group. Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction. N Engl J Med. 1981; 304:801–807.4. Choo EH, Chang K, Ahn Y, Jeon DS, Lee JM, Kim DB, et al. Benefit of β-blocker treatment for patients with acute myocardial infarction and preserved systolic function after percutaneous coronary intervention. Heart. 2014; 100:492–499.
Article5. Ellis K, Tcheng JE, Sapp S, Topol EJ, Lincoff AM. Mortality benefit of beta blockade in patients with acute coronary syndromes undergoing coronary intervention: pooled results from the Epic, Epilog, Epistent, Capture and Rapport Trials. J Interv Cardiol. 2003; 16:299–305.
Article6. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013; 127:e362–e425.7. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018; 39:119–177.8. Dargie HJ. Effect of carvedilol on outcome after myocardial infarction in patients with left-ventricular dysfunction: the CAPRICORN randomised trial. Lancet. 2001; 357:1385–1390.
Article9. Beddies G, Fox PR, Papich MD, Kanikanti VR, Krebber R, Keene BW. Comparison of the pharmacokinetic properties of bisoprolol and carvedilol in healthy dogs. Am J Vet Res. 2008; 69:1659–1663.
Article10. Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. Circulation. 2012; 126:2020–2035.
Article11. Kezerashvili A, Marzo K, De Leon J. Beta blocker use after acute myocardial infarction in the patient with normal systolic function: when is it “ok” to discontinue? Curr Cardiol Rev. 2012; 8:77–84.
Article12. Olsson G, Rehnqvist N, Sjögren A, Erhardt L, Lundman T. Long-term treatment with metoprolol after myocardial infarction: effect on 3 year mortality and morbidity. J Am Coll Cardiol. 1985; 5:1428–1437.
Article13. Kernis SJ, Harjai KJ, Stone GW, Grines LL, Boura JA, O'Neill WW, et al. Does beta-blocker therapy improve clinical outcomes of acute myocardial infarction after successful primary angioplasty? J Am Coll Cardiol. 2004; 43:1773–1779.
Article14. Nakatani D, Sakata Y, Suna S, Usami M, Matsumoto S, Shimizu M, et al. Impact of beta blockade therapy on long-term mortality after ST-segment elevation acute myocardial infarction in the percutaneous coronary intervention era. Am J Cardiol. 2013; 111:457–464.
Article15. Ozasa N, Kimura T, Morimoto T, Hou H, Tamura T, Shizuta S, et al. Lack of effect of oral beta-blocker therapy at discharge on long-term clinical outcomes of ST-segment elevation acute myocardial infarction after primary percutaneous coronary intervention. Am J Cardiol. 2010; 106:1225–1233.
Article16. Jonsson G, Abdelnoor M, Müller C, Kjeldsen SE, Os I, Westheim A. A comparison of the two beta-blockers carvedilol and atenolol on left ventricular ejection fraction and clinical endpoints after myocardial infarction. a single-centre, randomized study of 232 patients. Cardiology. 2005; 103:148–155.
Article17. Tölg R, Witt M, Schwarz B, Kurz T, Kurowski V, Hartmann F, et al. Comparison of carvedilol and metoprolol in patients with acute myocardial infarction undergoing primary coronary intervention--the PASSAT Study. Clin Res Cardiol. 2006; 95:31–41.
Article18. Mrdovic IB, Savic LZ, Perunicic JP, Asanin MR, Lasica RM, Jelena MM, et al. Randomized active-controlled study comparing effects of treatment with carvedilol versus metoprolol in patients with left ventricular dysfunction after acute myocardial infarction. Am Heart J. 2007; 154:116–122.
Article19. DiNicolantonio JJ, Lavie CJ, Fares H, Menezes AR, O'Keefe JH. Meta-analysis of carvedilol versus beta 1 selective beta-blockers (atenolol, bisoprolol, metoprolol, and nebivolol). Am J Cardiol. 2013; 111:765–769.
Article20. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet. 1999; 353:9–13.21. Poldermans D, Boersma E, Bax JJ, Thomson IR, Paelinck B, van de Ven LL, et al. Bisoprolol reduces cardiac death and myocardial infarction in high-risk patients as long as 2 years after successful major vascular surgery. Eur Heart J. 2001; 22:1353–1358.
Article22. Koshucharova G, Zweiker R, Maier R, Lercher P, Stepan V, Klein W, et al. Different beta-blocking effects of carvedilol and bisoprolol in human. J Clin Basic Cardiol. 2001; 4:53–56.23. Seo GW, Kim DK, Kim KH, Seol SH, Jin HY, Yang TH, et al. Impact of Carvedilol versus β1-selective β blockers (bisoprolol, metoprolol, and nebivolol) in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol. 2015; 116:1502–1508.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- No-Reflow Phoenomenon by Intracoronary Thrombus in Acute Myocardial Infarction
- Antiplate Agents
- Antiplatelet Agents in High-Risk Patients with Coronary Artery Disease
- Cardiac arrest due to an unexpected acute myocardial infarction during head and neck surgery: A case report
- Clinical outcome in elderly patients older than 70 years with acute myocardial infarction after use of platelet glycoprotein IIb/IIIa receptor blocker during percutaneous coronary intervention: Comparison with those younger than 70 years