Investig Clin Urol.
2018 May;59(3):166-176. 10.4111/icu.2018.59.3.166.
The prevalence of lower urinary tract symptoms in population aged 40 years or over, in South Korea
- Affiliations
-
- 1Department of Urology, Nowon Eulji Medical Center, Eulji University School of Medicine, Seoul, Korea.
- 2Department of Urology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. ksleedr@skku.edu
- 3Astellas Pharma Singapore Pte Ltd., Singapore, Singapore.
- 4Astellas Pharma Korea, Inc., Seoul, Korea.
- KMID: 2410589
- DOI: http://doi.org/10.4111/icu.2018.59.3.166
Abstract
- PURPOSE
Lower urinary tract symptoms (LUTS) can be distressing and socially isolating, and the economic impact can be substantial. Further data to characterize the epidemiology and effects of LUTS in South Korea would be beneficial.
MATERIALS AND METHODS
In an international, internet-based survey, the prevalence and impact of LUTS was evaluated in adults aged ≥40 years. Questions related to International Continence Society (ICS) symptom definitions and the bother associated with each symptom. The international prostate symptom score (IPSS) and the overactive bladder symptom score (OABSS) were assessed.
RESULTS
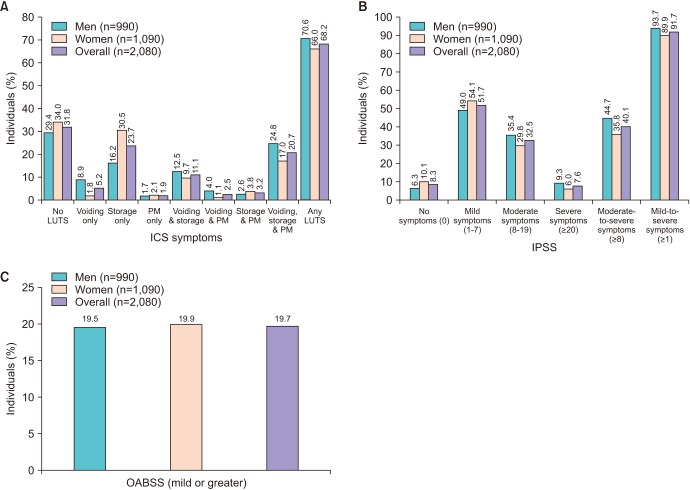
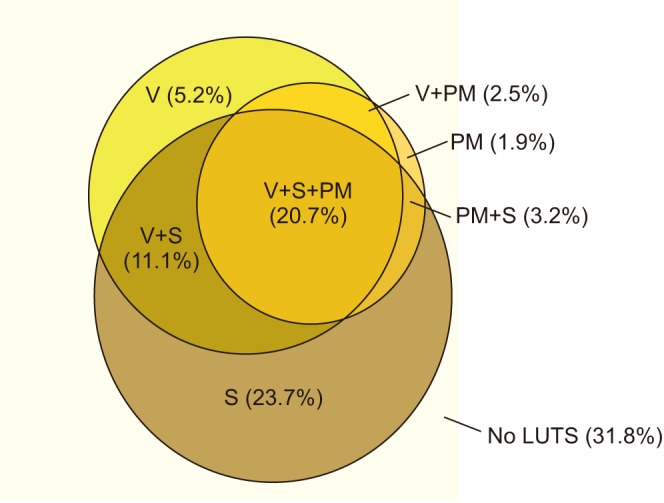
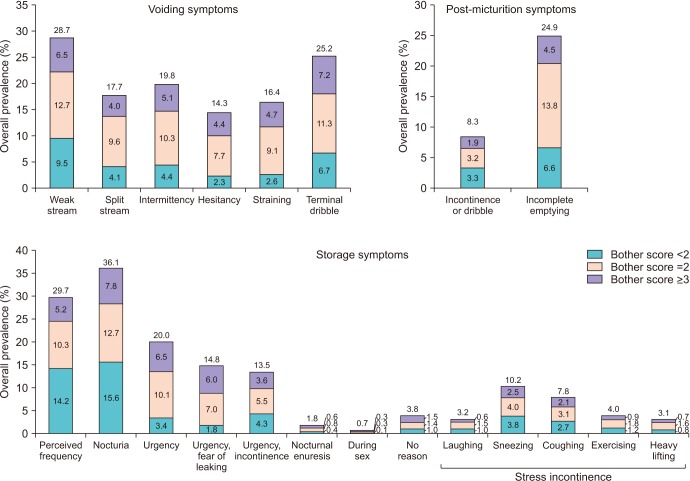
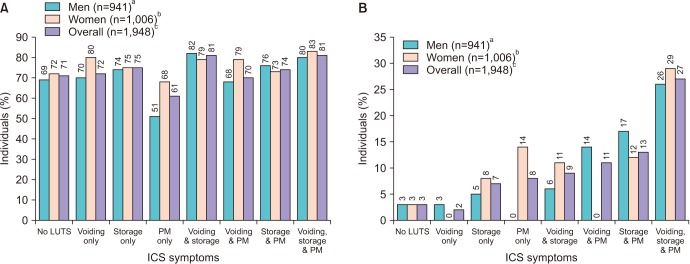
Of the 2,080 participants from South Korea, 1,090 (52.4%) were women and 740 (35.6%) were aged ≥60 years. The prevalence of LUTS according to ICS criteria was 68.2% (men, 70.6%; women, 66.0%). LUTS prevalence increased significantly with age (p=0.01 in men and women). Storage symptoms only were reported in 16.2% of men and 30.5% of women, making this the most common ICS symptom group overall. Individual symptoms with the highest prevalence in the overall population were nocturia, frequency, and weak stream (36%, 30%, and 29%, respectively). IPSS results showed that 40.1% of participants had at least moderate symptoms. The prevalence of OABSS-defined overactive bladder was 19.7% (men, 19.5%; women, 19.9%). Fourteen percent of individuals with any LUTS visited healthcare professionals regarding urinary symptoms.
CONCLUSIONS
LUTS affect the majority of adults aged ≥40 years in South Korea. The low percentage of individuals with LUTS consulting healthcare professionals regarding urinary symptoms indicates a need to improve rates of diagnosis and treatment.
MeSH Terms
Figure
Reference
-
1. Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the standardisation sub-committee of the International Continence Society. Neurourol Urodyn. 2002; 21:167–178. PMID: 11857671.
Article2. Coyne KS, Sexton CC, Thompson CL, Milsom I, Irwin D, Kopp ZS, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009; 104:352–360. PMID: 19281467.
Article3. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006; 50:1306–1314. PMID: 17049716.
Article4. Choi H, Bae JH. Overview of the epidemiology of lower urinary tract dysfunction in South Korea. Int Neurourol J. 2016; 20:91–100. PMID: 27377940.
Article5. Choo MS, Han JH, Shin TY, Ko K, Lee WK, Cho ST, et al. Alcohol, smoking, physical activity, protein, and Lower Urinary Tract Symptoms: prospective longitudinal cohort. Int Neurourol J. 2015; 19:197–206. PMID: 26620903.
Article6. Kim TH, Han DH, Lee KS. The prevalence of lower urinary tract symptoms in Korean men aged 40 years or older: a population-based survey. Int Neurourol J. 2014; 18:126–132. PMID: 25279239.
Article7. Lee E, Yoo KY, Kim Y, Shin Y, Lee C. Prevalence of lower urinary tract symptoms in Korean men in a community-based study. Eur Urol. 1998; 33:17–21. PMID: 9471036.
Article8. Lee YS, Lee KS, Jung JH, Han DH, Oh SJ, Seo JT, et al. Prevalence of overactive bladder, urinary incontinence, and lower urinary tract symptoms: results of Korean EPIC study. World J Urol. 2011; 29:185–190. PMID: 19898824.
Article9. Kwon CS, Lee JH. Prevalence, risk factors, Quality of Life, and health-care seeking behaviors of female urinary incontinence: results from the 4th Korean National Health and Nutrition Examination Survey VI (2007–2009). Int Neurourol J. 2014; 18:31–36. PMID: 24729925.
Article10. Coyne KS, Kaplan SA, Chapple CR, Sexton CC, Kopp ZS, Bush EN, et al. Risk factors and comorbid conditions associated with lower urinary tract symptoms: EpiLUTS. BJU Int. 2009; 103(Suppl 3):24–32.
Article11. Hwang EC, Kim SO, Nam DH, Yu HS, Hwang I, Jung SI, et al. Men with hypertension are more likely to have severe Lower Urinary Tract Symptoms and large prostate volume. Low Urin Tract Symptoms. 2015; 7:32–36. PMID: 26663649.
Article12. Jeong WS, Choi HY, Nam JW, Kim SA, Choi BY, Moon HS, et al. Men with severe Lower Urinary Tract Symptoms are at increased risk of depression. Int Neurourol J. 2015; 19:286–292. PMID: 26739184.
Article13. Lee KS, Choo MS, Seo JT, Oh SJ, Kim HG, Ng K, et al. Impact of overactive bladder on quality of life and resource use: results from Korean Burden of Incontinence Study (KOBIS). Health Qual Life Outcomes. 2015; 13:89. PMID: 26113125.
Article14. Kim TH, Han DH, Ryu DS, Lee KS. The impact of lower urinary tract symptoms on quality of life, work productivity, depressive symptoms, and sexuality in Korean men aged 40 years and older: a population-based survey. Int Neurourol J. 2015; 19:120–129. PMID: 26126442.
Article15. Martin S, Vincent A, Taylor AW, Atlantis E, Jenkins A, Januszewski A, et al. Lower Urinary Tract Symptoms, depression, anxiety and systemic inflammatory factors in men: a population-based cohort study. PLoS One. 2015; 10:e0137903. PMID: 26445118.
Article16. Park WH. Urinary incontinence and physician's attitude. J Korean Med Sci. 2013; 28:1559–1560. PMID: 24265515.
Article17. Chapple C, Castro-Diaz D, Chuang YC, Lee KS, Liao L, Liu SP, et al. Prevalence of Lower Urinary Tract Symptoms in China, Taiwan and South Korea: results from a cross-sectional, population-based study. Adv Ther. 2017; 34:1953–1965. PMID: 28687936.
Article18. Chuang YC, Liu SP, Lee KS, Liao L, Wang J, Yoo TK, et al. Prevalence of overactive bladder in China, Taiwan and South Korea: results from a cross-sectional, population-based study. Low Urin Tract Symptoms. 2017; 10. 02. [Epub]. DOI: 10.1111/luts.12193.
Article19. Barry MJ, Fowler FJ Jr, O'Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The measurement committee of the American Urological Association. J Urol. 1992; 148:1549–1557. PMID: 1279218.20. Homma Y, Uemura S. Use of the short form of King's Health Questionnaire to measure quality of life in patients with an overactive bladder. BJU Int. 2004; 93:1009–1013. PMID: 15142153.
Article21. Irwin DE, Milsom I, Kopp Z, Abrams P, Artibani W, Herschorn S. Prevalence, severity, and symptom bother of lower urinary tract symptoms among men in the EPIC study: impact of overactive bladder. Eur Urol. 2009; 56:14–20. PMID: 19278775.
Article22. Willis-Gray MG, Dieter AA, Geller EJ. Evaluation and management of overactive bladder: strategies for optimizing care. Res Rep Urol. 2016; 8:113–122. PMID: 27556018.23. Ikeda M, Nozawa K. Prevalence of overactive bladder and its related factors in Japanese patients with diabetes mellitus. Endocr J. 2015; 62:847–854. PMID: 26166691.
Article24. Wang Y, Xu K, Hu H, Zhang X, Wang X, Na Y, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn. 2011; 30:1448–1455. PMID: 21826714.
Article25. Luber KM. The definition, prevalence, and risk factors for stress urinary incontinence. Rev Urol. 2004; 6(Suppl 3):S3–S9.26. Shin YS, On JW, Kim MK. Clinical significance of diabetes mellitus on detrusor functionality on stress urinary incontinent women without bladder outlet obstruction. Int Urogynecol J. 2016; 27:1557–1561. PMID: 26992723.
Article27. Sadik CD, Ajay D, Le NP. Evaluation and management of neurogenic stress urinary incontinence. Curr Bladder Dysfunct Rep. 2014; 9:108–113.
Article28. Organisation for Economic Co-operation and Development. OECD data: daily smokers [Internet]. OECD;cited 2018 Mar 23. Available from: https://data.oecd.org/healthrisk/daily-smokers.htm.29. Jo JK, Lee S, Kim YT, Choi HY, Kim SA, Choi BY, et al. Analysis of the risk factors for overactive bladder on the basis of a survey in the community. Korean J Urol. 2012; 53:541–546. PMID: 22949998.
Article30. Irwin DE, Milsom I, Kopp Z, Abrams P, Group ES. Symptom bother and health care-seeking behavior among individuals with overactive bladder. Eur Urol. 2008; 53:1029–1037. PMID: 18243515.
Article31. Xu D, Zhao M, Huang L, Wang K. Overactive bladder symptom severity, bother, help-seeking behavior, and quality of life in patients with type 2 diabetes: a path analysis. Health Qual Life Outcomes. 2018; 16:1. PMID: 29291738.
Article32. Pan-Pacific Continence Society (PPCS). Korean Continence Society [Internet]. PPCS;cited 2018 Mar 23. Available from: https://www.ppcsoffice.org/local-societies-1.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prevalence of Lower Urinary Tract Symptoms in Korean Men Aged 40 Years or Older: A Population-Based Survey
- Overview of the Epidemiology of Lower Urinary Tract Dysfunction in South Korea
- The Prevalence of Lower Urinary Tract Symptoms and Overactive Bladder in South Korea: A Cross-Sectional, Population-Based Study
- Trends in Age-Specific Prevalence of Lower Urinary Tract Dysfunction: A Nationwide Population-Based Cohort Study
- The Impact of Lower Urinary Tract Symptoms on Quality of Life, Work Productivity, Depressive Symptoms, and Sexuality in Korean Men Aged 40 Years and Older: A Population-Based Survey