J Korean Soc Echocardiogr.
1994 Dec;2(2):115-128. 10.4250/jkse.1994.2.2.115.
A Study on the Delayed Percutaneous Transluminal Coronary Angioplasty in Acute Myocardial Infarction
- Affiliations
-
- 1Department of Internal Medicine, Chonnam University Medical School, Kwangju, Korea.
- KMID: 2410439
- DOI: http://doi.org/10.4250/jkse.1994.2.2.115
Abstract
- BACKGROUND
Early reperfusion after acute myocardial infarction is known to be effective in salvaging myocardium and hence improving early and late mortality and morbidity. The late reperfusion by percutaneous transluminal coronary angioplasty(PTCA) is also reported to be helpful in improving mortality and morbidity also, however the exact mechanism is not kmown when the salvage of myocardium is not expected.
METHODS
In this study, 24 acute myocardial infarction patients who had not been undergone reperfusion therapy within 6 hours or those who had been failed to be recanalized were subjected to study. The patients were divided into two groups, group I, those who had little ischemic myocardium around the infarct(11 patients, all male, 59.1±9.8years) and group II, those who had considerable ischemic area around the infarct zone(13 patients, M : F=3.3 : 1, 60.9±9.7years) revealed by myocardial perfusion scanning with 201TI of 99mTC-MIBI. The area of ischemia and infarction, defect volume ratio and left ventricular dimensions global functions were measured before and after PTCA. The mortality and morbidity were also abserved.
RESULTS
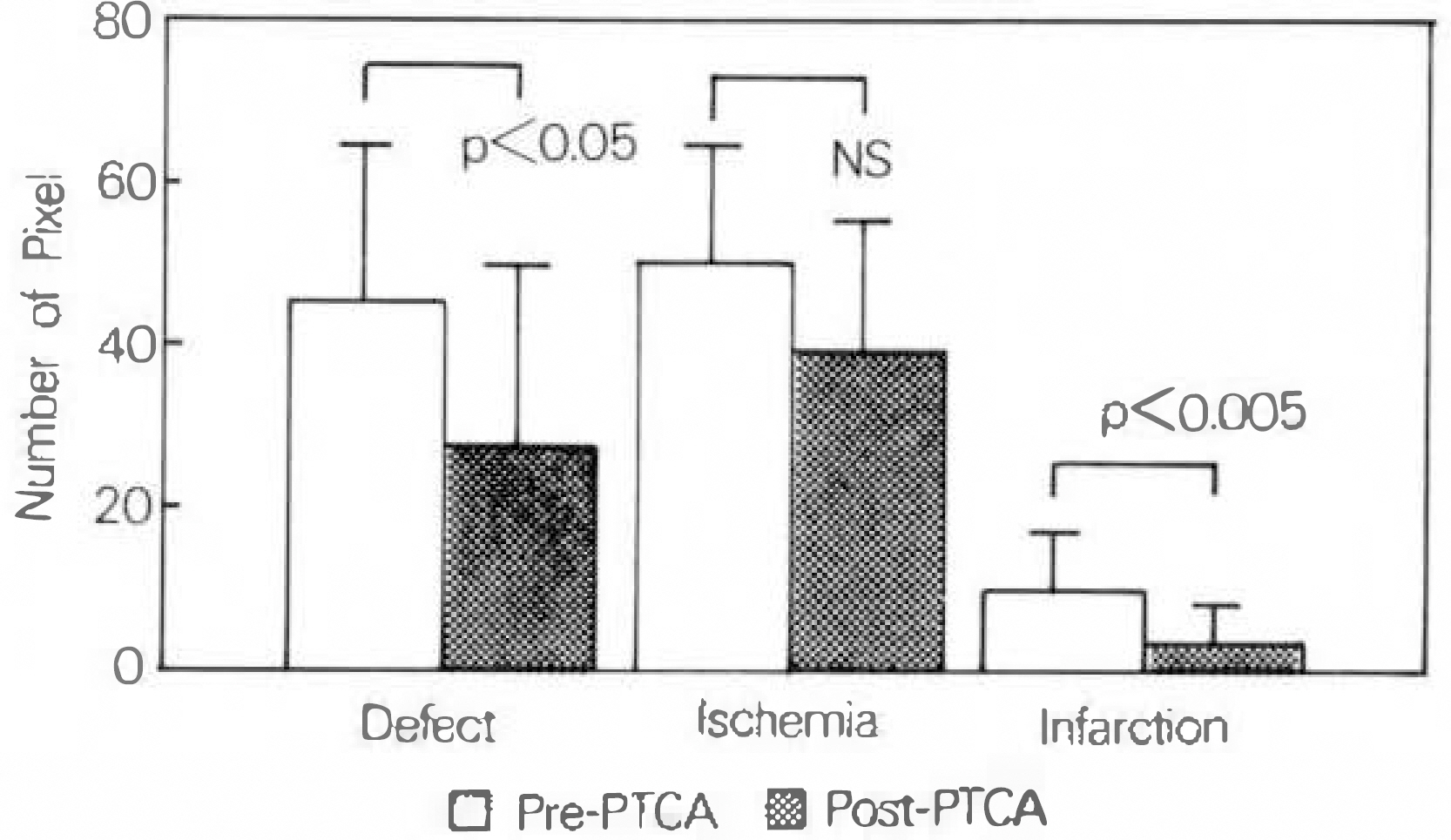
In group I the associated risk factors were hypertension in 5, hypercholesterolemia, 2 and smoking, 5 patients and in group II hypertension in 5, hypercholesterolemia, 4, smoking, 7 and diabetes mellitus, 2 patients. The PTCA was peformed 10.2±4.9days in proup I and 10.5±6.6days in group II after the admission. The infarct related arteries were left anterior descending artery in 12, left circumflex artery in 2 and right coronary artery in 10. Echocardiographic variables, i.e. left ventricular end-diastolic volume, left ventricular end-systolic volume, ejection fraction of the left ventricle and the E to A ratio of mitral flow measured by doppler echocardiography were compared before and after PTCA in each group. The variables were not differnt between two groups and were not changed after PTCA. Myocardial perfusion scanning revealed significantly decreased defect area(p < 0.05), infarct area(p < 0.005) and defect volume ratio(p < 0.05)after PTCA in group II. In group I, 6 patients out of 11 showed improved infarct area and defect volume ratio, but the mean of the group was not different before and after PTCA. There was neither mortality nor nonfatal infarction during follow up period of 15.9±3.8months in group I and 13.8±3.8months in group II.
CONCLUSION
Above results suggested that the delayed PTCA was efficacious in reducing perfusion defect area, infarct area and defect volume ratio in group II and in some patients of group I also and that the delayed PTCA might be effective in preventing further dilation of the left ventricle and further deterioration of the left ventricular functions in either group of the patients.
MeSH Terms
-
Angioplasty, Balloon, Coronary*
Arteries
Coronary Vessels
Diabetes Mellitus
Echocardiography
Echocardiography, Doppler
Follow-Up Studies
Heart Ventricles
Humans
Hypercholesterolemia
Hypertension
Infarction
Ischemia
Male
Mortality
Myocardial Infarction*
Myocardium
Perfusion
Reperfusion
Risk Factors
Smoke
Smoking
Stroke Volume
Ventricular Function, Left
Smoke
Figure
Reference
-
References
1). Gruppo Italiano per lo Studio della Streptochinasi nell'Infarto Miocardico(GISSI). Effectiveness of intravenous thrombolytic treatment in acute myocardial infarction. Lancet. 397:8478. 1986.2). Second International Study of Infarct Survival Collaborative Group. Randomized trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected myocardial infarction: ISIS-2. Lancet. 349:8607. 1988.3). Koshal A, Beanlands DS, Davies RA, Nair RC, Keon WJ. Urgent surgical reperfusion in acute evolving myocardial infarction. A randomized controlled study. Circulation. 78(suppl I):1–171. 1988.4). Kander NH, O'Neill WW, Topol EJ, Gallison L, Mileski R, Ellis SG. Longterm follow-up of patients treated with coronary angioplasty for acute myocardial infarction. Am Heart J. 118:228. 1989.
Article5). Braunwald E. Thrombolytic reperfusion of acute myocardial infarction: Resolved and unresolved issues. J Am Coll Cardiol. 12:85A. 1988.
Article6). Braunwald E. Myocardial reperfusion, limitation of infarct size, reduction of left ventricular dysfunction and improved survival: Should the paradigm be expanded ? Circulation. 79:441. 1989.7). Van de Werf F. Discrepancies between the effects of coronary reperfusion on survival and left ventricular function. Lancet. 1:1357. 1989.
Article8). Califf RM, Topol EJ, Gersh BJ. From myocardial salvage to patient salvage in acute myocardial infarction: The role of reperfusion therapy. J Am Coll Cariol. 14:1382. 1989.
Article9). TIMI study group. The throbolysis in myocardial infarction (TIMI) trial, Phase I findings. N Engl J Med. 312:932. 1985.10). Cohen M, Rentrop P. Limitation of myocardial ischemia by collateral circulation during sudden controlled coronary artery occlusion in human subjects: A prospective study. Circulation. 74:469. 1986.
Article11). Ryan TJ, Faxon DP, Gunnar RM, Kennedy JW, King SB, Loop FD, Peterson KL, Reeves TJ, Williams DO, Winters WL. Guidelines for percutaneous transluminal coronary angioplasty: A report of the American College of Cardiology/American Heart Association Task Force on assessment of diagnostic and therapeutic cardiovascular procedures. Circulation. 78:486. 1988.12). Eisner RI, Tamas MJ, Colinger K. Normal SPECT thallium-201 bull's eye display: Gender differences. J Nucl Med. 29:1901. 1988.13). Klein JL, Garcia EV, Depuey G. Reversibility of bulls-eye: A new polar bulls-eye map to quantify reversibility of stress-induced SPECT thallium-201 myocardial perfusion defects. J Nucl Med. 31:1240. 1990.14). Meinertz T, Kasper W, Schumacher M, Just H. The German multicenter trial of anisoylated plasminogen streptokinase activator complex versus heparin for acute myocardial infarciton. Am J Cardiol. 62:347. 1988.15). Dennedy JW, Ritchie JL, Davis KB, Fritz JK. Western Washington randomized trial of intracoronary streptokinase in myocardial infarction trial. Circulation. 70:867. 1984.16). Fortin DF, Califf RM. Long term survival from acute myocardial infarction: Salutary effect of an open coronary vessel. Am J Med. 88(suppl I):1N. 1990.17). Zaret BL, Walkers FJ, Treein M, Ross R, Knatterud G, Braunwald E. The TIMI Investigators Does left ventricular ejection fraction following thrombolytic therapy have the same prognostic impact described in the prethrombolytic era ? Results of the TIMI II Trial. J Am Coll Cardiol. 17:214A. (Abstract). 1991.18). Pizada FA, Weiner JM, Hood WB Jr. Experimehntal myocardial infarciton, 14: accelerated myocardial stiffening related to coronary reperfusion following ischemia. Chest. 74:190. 1978.19). Hochman JS, Choo H. Limitation of myocardial infarct expansion by reperfusion independent of myocardial salvage. Circulation. 75:299. 1987.
Article20). Althaus U, Gunther HP, Baur H, Hamburger S, Roos B. Consequences of myocardial reperfusion following temporary coronary occlusion in pigs: Effects on morphlogic, biochemical and haemodynamic findings. Eur J Clin Invest. 7:437. 1977.21). Meizlish JL, Berger HJ, Plankey M, Entrico D, Levy W, Zaret BL. Functional left ventricular aneurysm formation after acute anterior transmural myocardial infarction: Incidence, natural history and prognostic implications. N Engl J Med. 311:1001. 1984.22). Forman MB, Collins HW, Kopelman HA, Vaughan WK, Perry JM, Virmani R, Friesinger GC. Determinants of left ventricular aneurysm formation after acute anterior myocardial infarction: A clinical and angiographic study. J Am Coll Cariol. 8:1256. 1986.23). Touchstone DA, Beller GA, Nygaard TW, Tedesco C, Kaul S. Effects of successful intravenous reperfusion therapy on regional myocardial function and geometry in humans: A tomographic assessment using two-dimensional echocardiography. J Am Coll Cardiol. 13:1506. 1989.
Article24). Hirai T, Fujita M, Nakajima H, Asanoi H, Yamanishi K, Ohno A, Sasayama S. Importance of collateral circulation for prevention of left ventricular aneurysm formation in acute myocardial infarction. Ciuculation. 79:791. 1989.
Article25). Leung WH, Lau CP. Effects of severity of the residual stenosis of the infarct-related coronary artery on left ventricular dilation and function after acute myocardial infarction. J Am Coll Cardiol. 20:307. 1992.
Article26). Lavie CJ, O'Keefe JH, Chesebro JH, CLements IP, Gibbons RJ. Prevention of late ventricular dilation after acute myocardial infarction by successful thrombolytic reperfusion. Am J Cardiol. 66:31. 1990.27). Topol EJ, Califf RM, Vandormael M, Grines CL, George BS, Sanz ML, Wall T, O'Brien M, Schwaiger M, Aguirre FV, Young S, Popma JJ, Sigmon KN, Lee KL, Ellis SG. The Thrombolysis and Angioplasty in Myocardial Infarction-6 Study Group. A randomized trial of late reperfusion for acute myocardial infarction. Circulation. 85:2090. 1992.28). Hirayama A, Nishidi K, Kodama K. Prevention of left ventricular dilation without infarct size limitation by late reperfusion in patients with acute myocardial infarction. Jpn Circ J. 56(suppl 5):1438. 1992.29). Schröder R, Neuhaus K-L, Linderer T, Bruggemann T, Tebbe U, Wegscheider K. Impact of late coronary artery reperfusion on left ventricular function one month after acute myocardial infarction (results from the ISAM study). Am J Cardiol. 64:878. 1989.
Article30). Jeremy RW, Hackworthy RA, Bautovich G, Hutton BF, Harris PJ. Infarct artery perfusion and changes in left ventricular volume in the month after acute myocardial infarction. J Am Coll Cardiol. 9:989. 1987.
Article31). Pfeffer MA, Lamas GA, Vaughan DE, Parisi AF. Braunwald EyEffects of captopril on progressive ventricular dilatation after anterior myocardial infarction. N Engl J Med. 319:80. 1988.32). Hirayama A, Mishima M, Nishida K. Limitatiom of infarct expansion by late reperfusion independent of myocardial salvage in patients with acute myocardial infarction. Circulation. 84(suppl II):11–232. (Abstract). 1991.33). Montalescot G, Faraggi M, Drobinski G, Messian O, Evans J, Grosgoeat Y, Thomas D. Myocardial viability in patients with Q wave myocardial infarction and no residual ischemia. Circulation. 86:47. 1992.
Article34). Sabia PJ, Powers ER, Ragosta M, Sarembock KJ, Burwell LR, Kaul S. An association between collateral blood flow and myocardial viability in patients with recent myocardial infarction. N Engl J med. 327:1825. 1992.
Article35). Vermeer F, Simoons ML, Lubsen J. Reduced frequency of ventricular fibrillation after early thrombolysis in muyocardial infarction. Lancet. 1:1147. 1986.36). Schröder R. Ventricular fibrillation complicating myocardial infarction. N Engl J Med. 318:381. (Letter). 1988.
Article37). Arnold JMO, Antman EM, Przydlenk K, Braunwald E, Sando T, Vivaldi MT, Schoen FJ, Kloner RA. Differential effects of reperfusion on incidence of ventricular arrhythmias and recovery of ventricular function at 4 days following coronary occlusion. Am Heart J. 113:1055. 1987.
Article38). LATE Study Group. Late assessment of thrombolytic efficacy (LATE) study with alteplase 6–24 hours after onset of acute myocardial infarction. Lancet. 342:759. 1993.39). EMERAS(Estudio Multicéntrico Estreptoquinasa Repúlicas de America del Sur) Collabartive Group. Randomised trial of late thrombolysis in patients with suspected acute myocardial infarction. Lancet. 342:767. 1993.40). Bernardi MM, Whitlow PL. Reperfusion later than five days after acute myocardial infarction improves three-year survival. Circulation. 84(suppl II):11–232. (Abstract). 1991.41). Fay WP, Schawartz RS, Holmes DR, Owen WG. High concentrations of plasminogen activator inhibitor-1 within coronary artery thrombi. Circulation. 82(suppl III):III–601. (Abstract). 1991.42). Sabovic M, Lijen HR, Keber D, Collen D. Correlation between progressive absorption of plasminogen to blood clots and their sensitivity to lysis. Thromb Haemost. 64:450. 1990.43). Davies MJ. Successful and unsuccessful coronary thrombolysis. Br Heart J. 61:381. 1989.
Article44). Kim CB, Braunwald E. Potential benefits on late reperfusion of infarcted myocardium, the open artery hypothesis. Circulation. 88:2426. 1993.45). Marshall RC, Tillisch JH, Phelps ME, Huang SC, Carson R, Henez E, Cshelbert HR. Indetification and differentiation of resting myocardial ischemia and infarction in man with positron computed tomography, 18F-labeled fluorodeoxyglucose and N-13 ammonia. Circulation. 67:766. 1983.46). Dilsizian V, Bonow RO. Current diagnostic techniques of assessing myocardial viability in patient with hibernating and stunned myocardium. Circulation. 87:1. 1993.47). Schaefer S, Gober J, Valenza M, Karczmar GS, Matson GB, Camacho SA, Botvinick EH, Massie B, Weiner MW. Nuclear magnetic resonance imaging-guided phosphorous-31 spectroscopy of the human heart. J Am Coll Cardiol. 12:1449. 1988.48). Simoons ML, Wijns W, Balakumaran K, Serruys PW, van den Brand M, Fioretti P, Reiber JHC, Lie P, Hugenholtz PG. The effect of intracoronary thrombolysis with streptokinase on myocardial thallium distribution and left ventricular function by blood pool scintigraphy. Eur Heart J. 3:433. 1982.49). De Coster PM, Melin JA, Detry JMR, Brasseur LA, Beckers C, Col J. Coronary artery reperfusion in acute myocardial infarction: Assessment by pre- and postintervention thallium-201 myocardial perfusion imaging. Am J Cardiol. 55:889. 1985.
Article50). Verani MS, Jeroudi MO, Mahmarian JJ, Boyce TM, Neto SB, Patel B, Bolli R. Quantification of myocardial infarction during coronary occlusion and myocardial salvage after reperfusion using cardiac imaging with techetium-99m hexakis 2-methylisobutyl isonitrile. J Am Coll Cardiol. 12:1573. 1988.51). Ruduto LA, Freund GC, Gaeta JM, Samlling RW, Lewis B, Gould KL. Coronary artery reperfusion in acute myocardial inafarction: Beneficial effects of intracoronary streptokinase on left ventricular salvage and performance. Am Heart J. 102:1168. 1981.52). Wakers FJ, Gibbons RJ, Verani MS, Kayden DS, Pellikka PA, Beherendek T, Mahmarian JJ. Serial quantitative planar technetium-99m-isonitrile imaging in acute myocardial infraction: Efficacy for noninvassive assessment of thrombolytic therapy. J Am Coll Cardiol. 14:861. 1989.53). Parisi AF, Moynihan PF, Folland ED. Echocardiographic evaluation of left ventricular function. Med Clin North Am. 64:61. 1980.
Article54). Gueret P, Meerbaum S, Wyatt HL, Uchiyama T, Lang TW, Corday E. Two-dimensional echocardiographic quantitation of left ventricular volumes and ejection fraction. Circulation. 62:1308. 1980.55). Gehrke J, Leeman S, Raphael M, Pridie RB. Non-invasive left ventricular volume determination by two-dimensional echocardigraphy. Br Heart J. 37:911. 1975.56). Gordon EP, Schnittger I, Fitzerald PJ, Williams P, Popp RL. Reproducibity of left ventricular volumes by two-dimensional echocardiography. J Am Coll Cardiol. 2:506. 1983.57). Dzavik V, Beanlands DS, Human DP, Davies RF, Leddy D, Marquis JF, Teo KK, Ruddy TD, Burton JR. Effect of late percutaneous transluminal coronary angioplasty of an occluded infarct-related coronary artery on left ventricular function in patients with a recent (<6 weeks) Q-wave acute myocardial infarction (Total Occlusion Post-Myocardial Infarction Interventional Study [TOMIIS]-a pilot study). Am J Cardiol. 73:856. 1994.58). Sabri MN, DiSciascio G, Cowley M, Goudreau E, Warner M, Kohli R, Bajaj S, Kelley M, Vetrovec G. Immediate and long-term results of delayed recanalization of occluded acute myocardial infarction-related arteries using coronary angioplasty. Am J Cardiol. 69:575. 1992.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Percutaneous Transluminal Coronary Angioplasty with Stent in a Patient of Acute Myocardial Infarction with Situs Inversus Totalis
- A Case of Acute Myocardial Infraction in Patients with Dextrocardia with Situs Inversus Treated by Percutaneous Translumnal Coronary Angioplasty
- Acute myocardial infarction in young patient probably due to Kawasaki disease
- Percutaneous transluminal coronary angioplasty for ostial stenosis of the left coronary artery
- Effect of Percutaneous Transluminal Coronary Angioplasty in Treatment of Cardiogenic Shock Complicating Acute Myocardial Infarction