Ann Surg Treat Res.
2018 May;94(5):240-246. 10.4174/astr.2018.94.5.240.
Bile duct segmental resection versus pancreatoduodenectomy for middle and distal common bile duct cancer
- Affiliations
-
- 1Department of Surgery, Ewha Womans University Mokdong Hospital, Ewha Womans University School of Medicine, Seoul, Korea. huisong.lee@ewha.ac.kr
- KMID: 2410267
- DOI: http://doi.org/10.4174/astr.2018.94.5.240
Abstract
- PURPOSE
To compare survival outcomes between bile duct segmental resection (BDR) and pancreatoduodenectomy (PD) for the treatment of middle and distal bile duct cancer.
METHODS
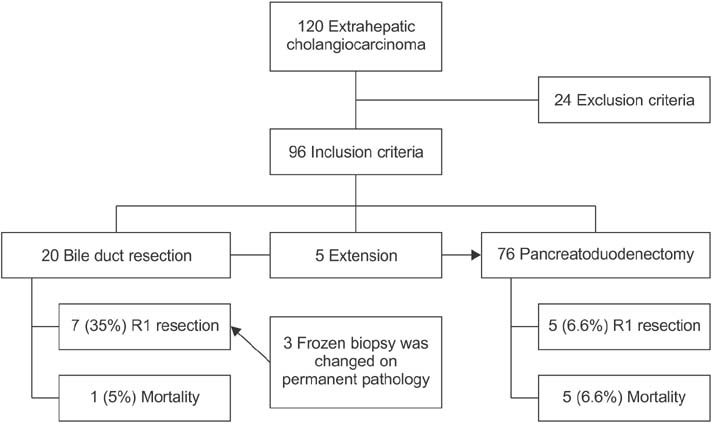
From 1997 to 2013, a total of 96 patients who underwent curative intent surgery for middle and distal bile duct cancer were identified. The patients were divided into 2 groups based on the type of operation; 20 patients were included in the BDR group and 76 patients were in the PD group. We retrospectively reviewed the clinical outcomes.
RESULTS
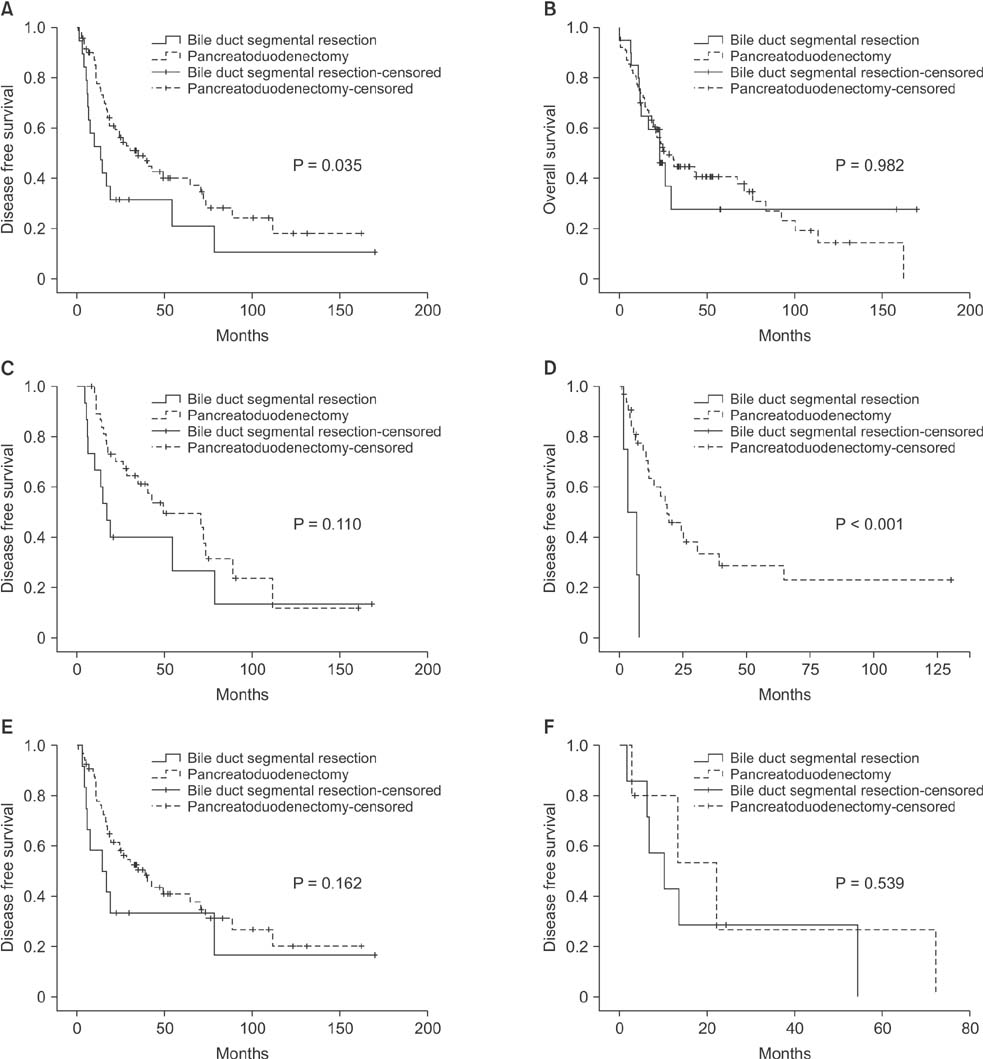
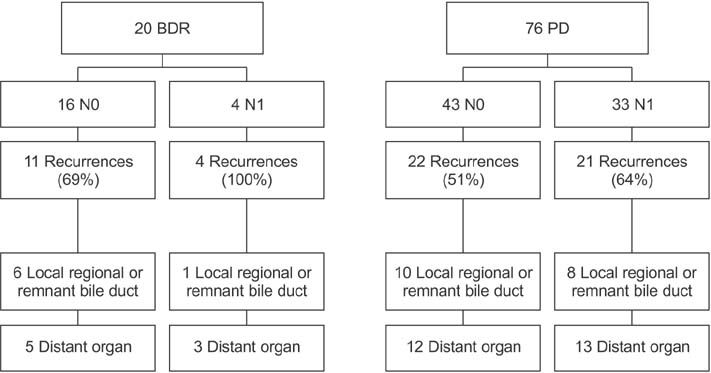
The number of lymph nodes (LNs) was significantly greater in patients within the PD group compared to the BDR group. The total number of LNs was 6.5 ± 8.2 vs. 11.2 ± 8.2 (P = 0.017) and the number of metastatic LNs was 0.4 ± 0.9 vs. 1.0 ± 1.5 (P = 0.021), respectively. After a median follow-up period of 24 months (range, 4-169 months), the recurrence-free survival of the PD group was superior to that of the BDR group (P = 0.035). In the patients with LN metastases, the patients undergoing PD had significantly better survival than the BDR group (P < 0.001).
CONCLUSION
Surgeons should be cautious in deciding to perform BDR for middle and distal common bile duct cancer. PD is recommended if LN metastases are suspected.
Keyword
MeSH Terms
Figure
Reference
-
1. Nakeeb A, Pitt HA, Sohn TA, Coleman J, Abrams RA, Piantadosi S, et al. Cholangiocarcinoma. A spectrum of intrahepatic, perihilar, and distal tumors. Ann Surg. 1996; 224:463–473.2. Kondo S, Takada T, Miyazaki M, Miyakawa S, Tsukada K, Nagino M, et al. Guidelines for the management of biliary tract and ampullary carcinomas: surgical treatment. J Hepatobiliary Pancreat Surg. 2008; 15:41–54.3. Skipworth JR, Keane MG, Pereira SP. Update on the management of cholangiocarcinoma. Dig Dis. 2014; 32:570–578.
Article4. Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Shimizu Y, et al. Aggressive surgical approaches to hilar cholangiocarcinoma: hepatic or local resection? Surgery. 1998; 123:131–136.
Article5. Seyama Y, Makuuchi M. Current surgical treatment for bile duct cancer. World J Gastroenterol. 2007; 13:1505–1515.
Article6. Lee HG, Lee SH, Yoo DD, Paik KY, Heo JS, Choi SH, et al. Carcinoma of the middle bile duct: is bile duct segmental resection appropriate? World J Gastroenterol. 2009; 15:5966–5971.7. Adam U, Makowiec F, Riediger H, Schareck WD, Benz S, Hopt UT. Risk factors for complications after pancreatic head resection. Am J Surg. 2004; 187:201–208.
Article8. Chang YR, Kang MJ, Kim H, Jang JY, Kim SW. The natural course of pancreatic fistula and fluid collection after distal pancreatectomy: is drain insertion needed? Ann Surg Treat Res. 2016; 91:247–253.
Article9. Sukharamwala P, Thoens J, Szuchmacher M, Smith J, DeVito P. Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB (Oxford). 2012; 14:649–657.10. Kapoor VK. Complications of pancreatoduodenectomy. Rozhl Chir. 2016; 95:53–59.11. Bock EA, Hurtuk MG, Shoup M, Aranha GV. Late complications after pancreaticoduodenectomy with pancreaticogastrostomy. J Gastrointest Surg. 2012; 16:914–919.
Article12. Todoroki T, Kawamoto T, Koike N, Fukao K, Shoda J, Takahashi H. Treatment strategy for patients with middle and lower third bile duct cancer. Br J Surg. 2001; 88:364–370.
Article13. Sasaki R, Takahashi M, Funato O, Nitta H, Murakami M, Kawamura H, et al. Prognostic significance of lymph node involvement in middle and distal bile duct cancer. Surgery. 2001; 129:677–683.
Article14. Jang JY, Kim SW, Park DJ, Ahn YJ, Yoon YS, Choi MG, et al. Actual long-term outcome of extrahepatic bile duct cancer after surgical resection. Ann Surg. 2005; 241:77–84.
Article15. Kiriyama M, Ebata T, Aoba T, Kaneoka Y, Arai T, Shimizu Y, et al. Prognostic impact of lymph node metastasis in distal cholangiocarcinoma. Br J Surg. 2015; 102:399–406.16. Konishi M, Iwasaki M, Ochiai A, Hasebe T, Ojima H, Yanagisawa A. Clinical impact of intraoperative histological examination of the ductal resection margin in extrahepatic cholangiocarcinoma. Br J Surg. 2010; 97:1363–1368.
Article17. Bahra M, Jacob D, Langrehr JM, Neumann UP, Neuhaus P. Carcinoma of the distal and middle bile duct: surgical results, prognostic factors, and long-term follow-up. J Hepatobiliary Pancreat Surg. 2008; 15:501–507.
Article18. Hernandez J, Cowgill SM, Al-Saadi S, Villadolid D, Ross S, Kraemer E, et al. An aggressive approach to extrahepatic cholangiocarcinomas is warranted: margin status does not impact survival after resection. Ann Surg Oncol. 2008; 15:807–814.
Article19. Murakami Y, Uemura K, Hayashidani Y, Sudo T, Hashimoto Y, Ohge H, et al. Prognostic significance of lymph node metastasis and surgical margin status for distal cholangiocarcinoma. J Surg Oncol. 2007; 95:207–212.
Article20. Sakamoto Y, Kosuge T, Shimada K, Sano T, Ojima H, Yamamoto J, et al. Prognostic factors of surgical resection in middle and distal bile duct cancer: an analysis of 55 patients concerning the significance of ductal and radial margins. Surgery. 2005; 137:396–402.
Article21. Kwon HJ, Kim SG, Chun JM, Lee WK, Hwang YJ. Prognostic factors in patients with middle and distal bile duct cancers. World J Gastroenterol. 2014; 20:6658–6665.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cutaneous Metastasis of Distal Common Bile Duct Carcinoma
- The Results of Curative Reoperation for Recurrent Cancer of the Extrahepatic Biliary Tract
- Comparison of Survival Outcomes following Segmental Bile Duct Resection versus Pancreatoduodenectomy for Mid Bile Duct Cancer
- 4 Cases of Web of Common Bile Duct
- Bile Duct Cystadenocarcinoma