Brain Tumor Res Treat.
2018 Apr;6(1):39-42. 10.14791/btrt.2018.6.e6.
Intermediate Pilomyxoid Astrocytoma in the Cerebellum of a 5-Year-Old Boy
- Affiliations
-
- 1Department of Neurosurgery, Wonkwang University Hospital, Iksan, Korea. tykim@wku.ac.kr
- 2Department of Pathology, Chunnam National University Hwasun Hospital, Hwasun, Korea.
- KMID: 2410236
- DOI: http://doi.org/10.14791/btrt.2018.6.e6
Abstract
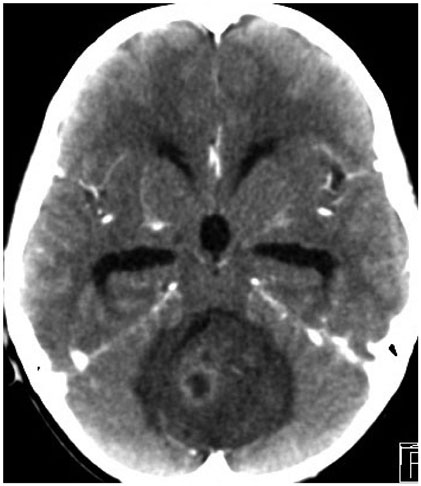
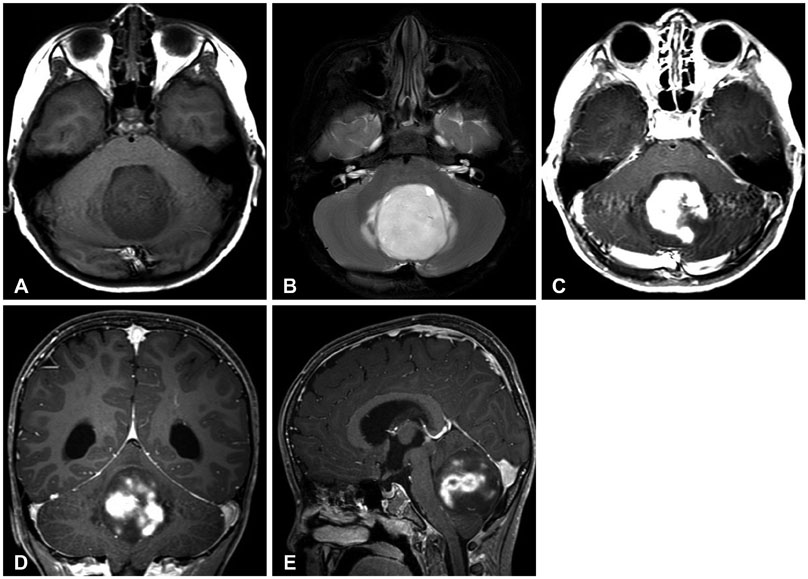
- Intermediate pilomyxoid tumors (IPTs) were defined by the presence of some features typical of pilomyxoid astrocytoma (PMA) in combination with features that could be considered more consistent with pilocytic astrocytoma (PA). PMA is rare in the cerebellum. And, IPT in the cerebellum is rarer than PMA. To our knowledge, only 2 reports have described IPT in the cerebellum. A 5-year-old boy had nausea and vomiting. Computed tomography revealed a large, round, low-density tumor in the cerebellar vermis area. On enhanced magnetic resonance imaging (MRI), the tumor showed inhomogeneous diffuse enhancement; the central portion showed homogenous enhancement, while the peripheral portion showed inhomogeneous enhancement. The patient underwent a midline suboccipital craniotomy, and gross total resection was performed. The tumor was gray-colored, rubbery hard, and severely hemorrhagic with a clear boundary. On pathologic examination, the combined features of both PA and PMA were retrospectively indicative of an IPT. The patient was symptom-free for 18 months, with no evidence of tumor recurrence on MRI. More observation and further studies on PMA and IPT are required to determine the most appropriate treatment for these tumors.
Keyword
MeSH Terms
Figure
Reference
-
1. Johnson MW, Eberhart CG, Perry A, et al. Spectrum of pilomyxoid astrocytomas: intermediate pilomyxoid tumors. Am J Surg Pathol. 2010; 34:1783–1791.2. Tihan T, Fisher PG, Kepner JL, et al. Pediatric astrocytomas with monomorphous pilomyxoid features and a less favorable outcome. J Neuropathol Exp Neurol. 1999; 58:1061–1068.
Article3. Komotar RJ, Burger PC, Carson BS, et al. Pilocytic and pilomyxoid hypothalamic/chiasmatic astrocytomas. Neurosurgery. 2004; 54:72–79. discussion 79-80.
Article4. Tsugu H, Oshiro S, Yanai F, et al. Management of pilomyxoid astrocytomas: our experience. Anticancer Res. 2009; 29:919–926.5. Okano A, Oya S, Fujisawa N, et al. Significance of radical resection for pilomyxoid astrocytoma of the cerebellum: a case report and review of the literature. Childs Nerv Syst. 2013; 29:1375–1379.
Article6. Forbes JA, Mobley BC, O'Lynnger TM, et al. Pediatric cerebellar pilomyxoid-spectrum astrocytomas. J Neurosurg Pediatr. 2011; 8:90–96.
Article7. Ajani OA, Al Sulaiti G, Al Bozom I. Pilomyxoid astrocytoma of the cerebellum. J Neurosurg Pediatr. 2011; 7:539–542.
Article8. Nagaishi M, Yokoo H, Hirato J, Yoshimoto Y, Nakazato Y. Clinico-pathological feature of pilomyxoid astrocytomas: three case reports. Neuropathology. 2011; 31:152–157.
Article9. El Beltagy MA, Atteya MM, El-Haddad A, et al. Surgical and clinical aspects of cerebellar pilomyxoid-spectrum astrocytomas in children. Childs Nerv Syst. 2014; 30:1045–1053.
Article10. Fernandez C, Figarella-Branger D, Girard N, et al. Pilocytic astrocytomas in children: prognostic factors--a retrospective study of 80 cases. Neurosurgery. 2003; 53:544–553. discussion 554-5.
Article11. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820.
Article12. Brat DJ, Scheithauer BW, Fuller GN, Tihan T. Newly codified glial neoplasms of the 2007 WHO Classification of Tumours of the Central Nervous System: angiocentric glioma, pilomyxoid astrocytoma and pituicytoma. Brain Pathol. 2007; 17:319–324.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Juvenile Pilomyxoid Astrocytoma in the Opticohypothalamus
- Adult Pilomyxoid Astrocytoma Mimicking a Cortical Brain Tumor: MR Imaging Findings
- Multiple Solid Pilocytic Astrocytomas in Cerebellum with Neurofibromatosis Type I: A Case Report
- Cerebellar Pleomorphic Xanthoastrocytoma: A Case Report
- Dysembryoplastic Neuroepithelial Tumor in the Cerebellum: Case Report