J Dent Anesth Pain Med.
2018 Apr;18(2):97-103. 10.17245/jdapm.2018.18.2.97.
The effect of dental scaling noise during intravenous sedation on acoustic respiration rate (RRaâ„¢)
- Affiliations
-
- 1Department of Dental Anesthesiology, Seoul National University Dental Hospital, Seoul, South Korea. stone90@snu.ac.kr
- 2Department of Pediatric Dentistry, Dankook University Sejong Dental Hospital, Sejong, South Korea.
- KMID: 2410142
- DOI: http://doi.org/10.17245/jdapm.2018.18.2.97
Abstract
- BACKGROUND
Respiration monitoring is necessary during sedation for dental treatment. Recently, acoustic respiration rate (RRaâ„¢), an acoustics-based respiration monitoring method, has been used in addition to auscultation or capnography. The accuracy of this method may be compromised in an environment with excessive noise. This study evaluated whether noise from the ultrasonic scaler affects the performance of RRa in respiratory rate measurement.
METHODS
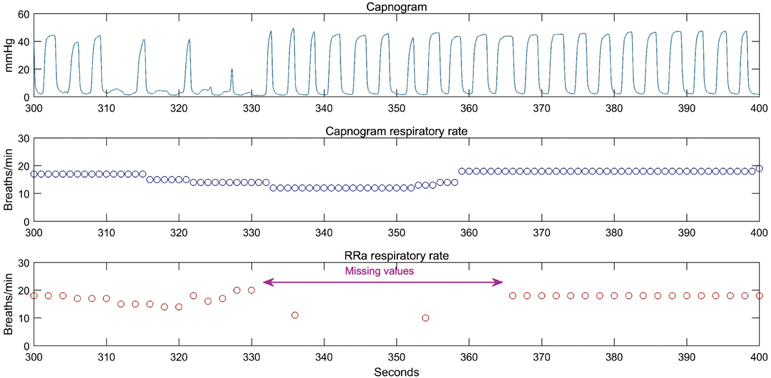
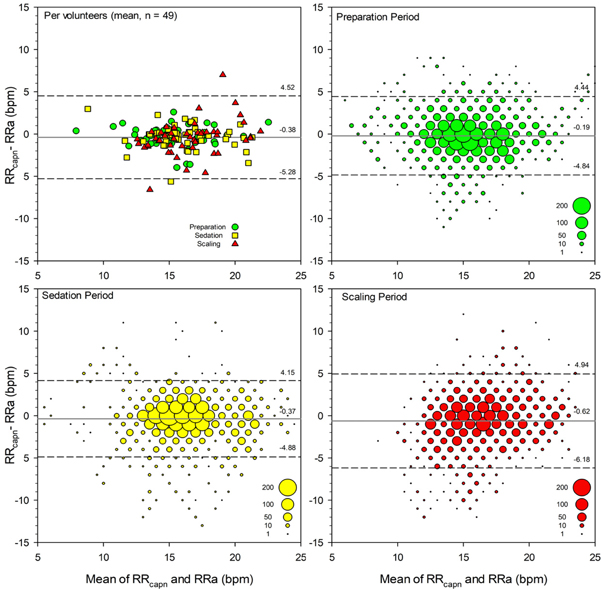
We analyzed data from 49 volunteers who underwent scaling under intravenous sedation. Clinical tests were divided into preparation, sedation, and scaling periods; respiratory rate was measured at 2-s intervals for 3 min in each period. Missing values ratios of the RRa during each period were measuerd; correlation analysis and Bland-Altman analysis were performed on respiratory rates measured by RRa and capnogram.
RESULTS
Respective missing values ratio from RRa were 5.62%, 8.03%, and 23.95% in the preparation, sedation, and scaling periods, indicating an increased missing values ratio in the scaling period (P < 0.001). Correlation coefficients of the respiratory rate, measured with two different methods, were 0.692, 0.677, and 0.562 in each respective period. Mean capnography-RRa biases in Bland-Altman analyses were −0.03, −0.27, and −0.61 in each respective period (P < 0.001); limits of agreement were −4.84-4.45, −4.89-4.15, and −6.18-4.95 (P < 0.001).
CONCLUSIONS
The probability of missing respiratory rate values was higher during scaling when RRa was used for measurement. Therefore, the use of RRa alone for respiration monitoring during ultrasonic scaling may not be safe.
MeSH Terms
Figure
Cited by 1 articles
-
Letter to the Editor - Response to: The effect of dental scaling noise during intravenous sedation on acoustic respiration rate
Steven J. Barker
J Dent Anesth Pain Med. 2018;18(3):195-196. doi: 10.17245/jdapm.2018.18.3.195.
Reference
-
1. Saiso K, Adnonla P, Munsil J, Apipan B, Rummasak D, Wongsirichat N. Complications associated with intravenous midazolam and fentanyl sedation in patients undergoing minor oral surgery. J Dent Anesth Pain Med. 2017; 17:199–204.
Article2. Tiret L, Nivoche Y, Hatton F, Desmonts JM, Vourc'h G. Complications related to anaesthesia in infants and children. A prospective survey of 40240 anaesthetics. Br J Anaesth. 1988; 61:263–269.3. Moller JT, Johannessen NW, Berg H, Espersen K, Larsen LE. Hypoxaemia during anaesthesia--an observer study. Br J Anaesth. 1991; 66:437–444.
Article4. An SY, Seo KS, Kim S, Kim J, Lee DW, Hwang KG, et al. Developmental procedures for the clinical practice guidelines for conscious sedation in dentistry for the korean academy of dental sciences. J Dent Anesth Pain Med. 2016; 16:253–261.
Article5. Practice guidelines for moderate procedural sedation and analgesia 2018: A report by the american society of anesthesiologists task force on moderate procedural sedation and analgesia, the american association of oral and maxillofacial surgeons, american college of radiology, american dental association, american society of dentist anesthesiologists, and society of interventional radiology. Anesthesiology. 2018; 128:437–479.6. Krauss B, Hess DR. Capnography for procedural sedation and analgesia in the emergency department. Ann Emerg Med. 2007; 50:172–181.
Article7. Ouchi K, Fujiwara S, Sugiyama K. Acoustic method respiratory rate monitoring is useful in patients under intravenous anesthesia. J Clin Monit Comput. 2017; 31:59–65.
Article8. Chi SI. Analysis on safety of and eeg change in various patient-controlled sedation methods during dental scaling (Doctoral dissertation). Seoul: Seoul National University;2017.9. Itoh A, Ishida A, Kikuchi N, Okazaki N, Kuratomi Y, Ishihara T, et al. Microcomputer-based respiratory function monitoring system using impedence pneumography. Med Biol Eng Comput. 1982; 20:620–624.
Article10. Dash S, Shelley KH, Silverman DG, Chon KH. Estimation of respiratory rate from ecg, photoplethysmogram, and piezoelectric pulse transducer signals: A comparative study of time-frequency methods. IEEE Trans Biomed Eng. 2010; 57:1099–1107.
Article11. Parker W, Estrich CG, Abt E, Carrasco-Labra A, Waugh JB, Conway A, et al. Benefits and harms of capnography during procedures involving moderate sedation: A rapid review and meta-analysis. J Am Dent Assoc. 2018; 149:38–50.e2.12. Mimoz O, Benard T, Gaucher A, Frasca D, Debaene B. Accuracy of respiratory rate monitoring using a non-invasive acoustic method after general anaesthesia. Br J Anaesth. 2012; 108:872–875.
Article13. Fukada T, Iwakiri H, Nomura M, Ozaki M. Clinical evaluation of acoustic respiration rate monitoring compared with conventional systems in the postanaesthesia care unit. Eur J Anaesthesiol. 2015; 32:61–63.
Article14. Autet LM, Frasca D, Pinsard M, Cancel A, Rousseau L, Debaene B, et al. Evaluation of acoustic respiration rate monitoring after extubation in intensive care unit patients. Br J Anaesth. 2014; 113:195–197.
Article15. Guechi Y, Pichot A, Frasca D, Rayeh-Pelardy F, Lardeur JY, Mimoz O. Assessment of noninvasive acoustic respiration rate monitoring in patients admitted to an emergency department for drug or alcoholic poisoning. J Clin Monit Comput. 2015; 29:721–726.
Article16. Frasca D, Geraud L, Charriere JM, Debaene B, Mimoz O. Comparison of acoustic and impedance methods with mask capnometry to assess respiration rate in obese patients recovering from general anaesthesia. Anaesthesia. 2015; 70:26–31.
Article17. Yang S, Menne A, Hu P, Stansbury L, Gao C, Dorsey N, et al. Acoustic sensor versus electrocardiographically derived respiratory rate in unstable trauma patients. J Clin Monit Comput. 2017; 31:765–772.
Article18. Patino M, Redford DT, Quigley TW, Mahmoud M, Kurth CD, Szmuk P. Accuracy of acoustic respiration rate monitoring in pediatric patients. Paediatr Anaesth. 2013; 23:1166–1173.
Article19. Yabuki S, Toyama H, Takei Y, Wagatsuma T, Yabuki H, Yamauchi M. Influences of environmental noise level and respiration rate on the accuracy of acoustic respiration rate monitoring. J Clin Monit Comput. 2018; 32:127–132.
Article20. Trenter SC, Walmsley AD. Ultrasonic dental scaler: Associated hazards. J Clin Periodontol. 2003; 30:95–101.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter to the Editor - Response to: The effect of dental scaling noise during intravenous sedation on acoustic respiration rate
- Current trends in intravenous sedative drugs for dental procedures
- Efficacy of active noise-canceling headphones in patients undergoing ultrasonic scaling
- Sedation at Sedation Clinic of Department of Dentistry in Hanyang University Medical Center (II)
- Introduction of Sedation Clinic at Department of Dentistry in Hanyang University Medical Center (I)