J Korean Ophthalmol Soc.
2018 Apr;59(4):307-313. 10.3341/jkos.2018.59.4.307.
The Clinical Effects of Triamcinolone-soaked Nasal Packing on Endonasal Dacryocystorhinostomy
- Affiliations
-
- 1Department of Ophthalmology, Konyang University College of Medicine, Daejeon, Korea. chullan@kyuh.ac.kr
- 2Myunggok Medical Research Institute, Konyang University, Daejeon, Korea.
- KMID: 2409677
- DOI: http://doi.org/10.3341/jkos.2018.59.4.307
Abstract
- PURPOSE
To evaluate the clinical effects of triamcinolone-soaked nasal packing on endonasal dacryocystorhinostomy (DCR).
METHODS
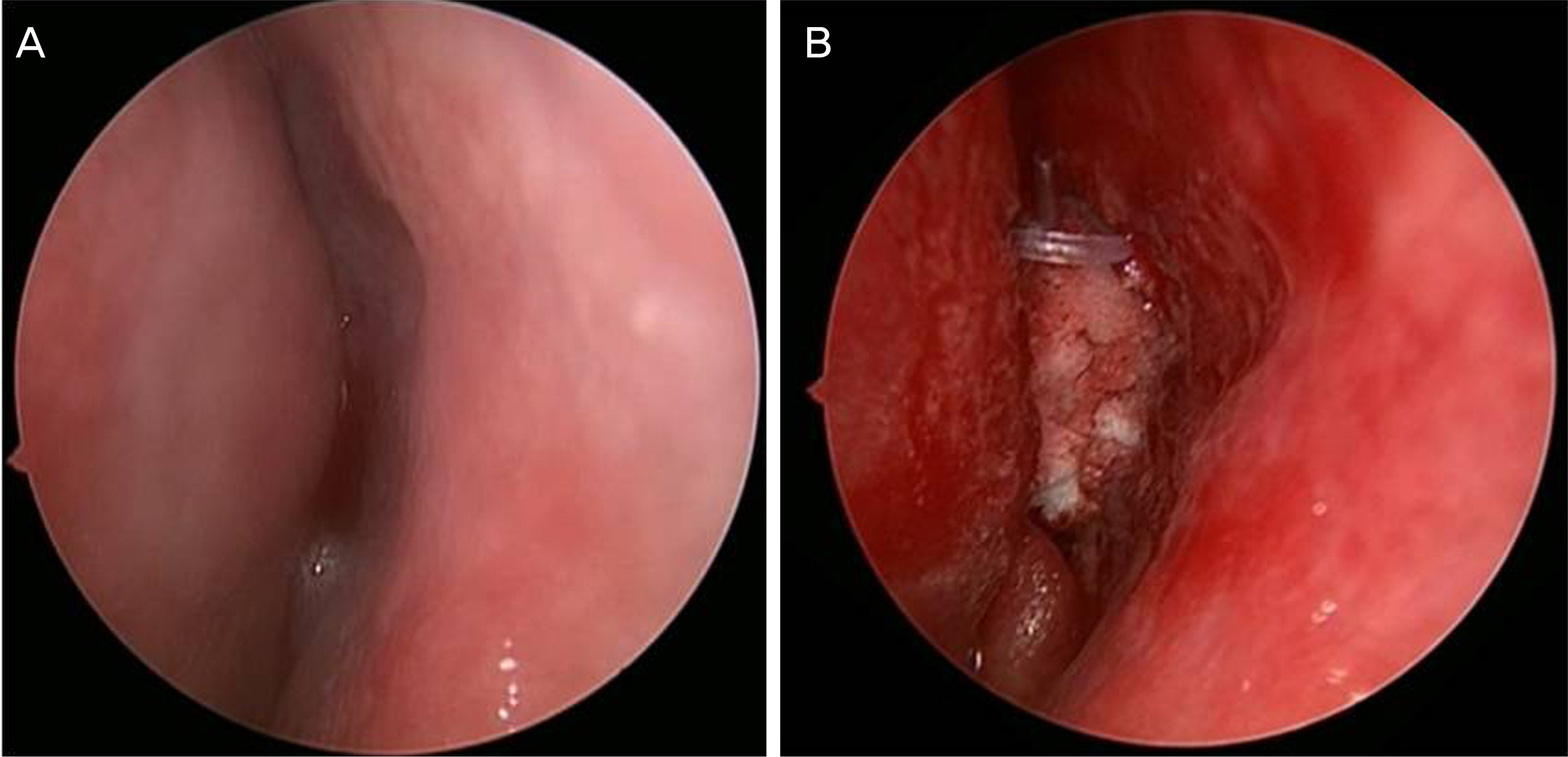
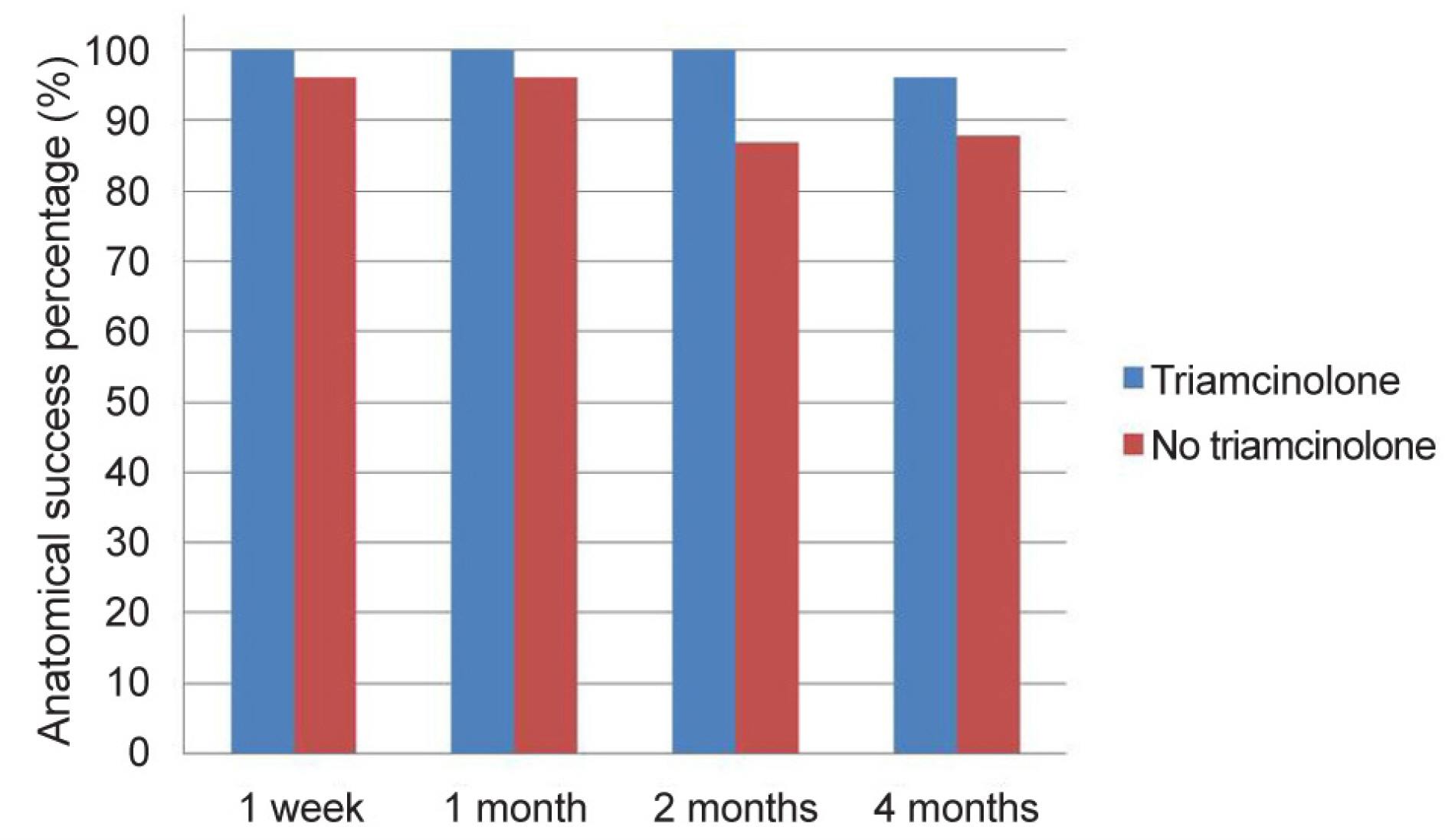
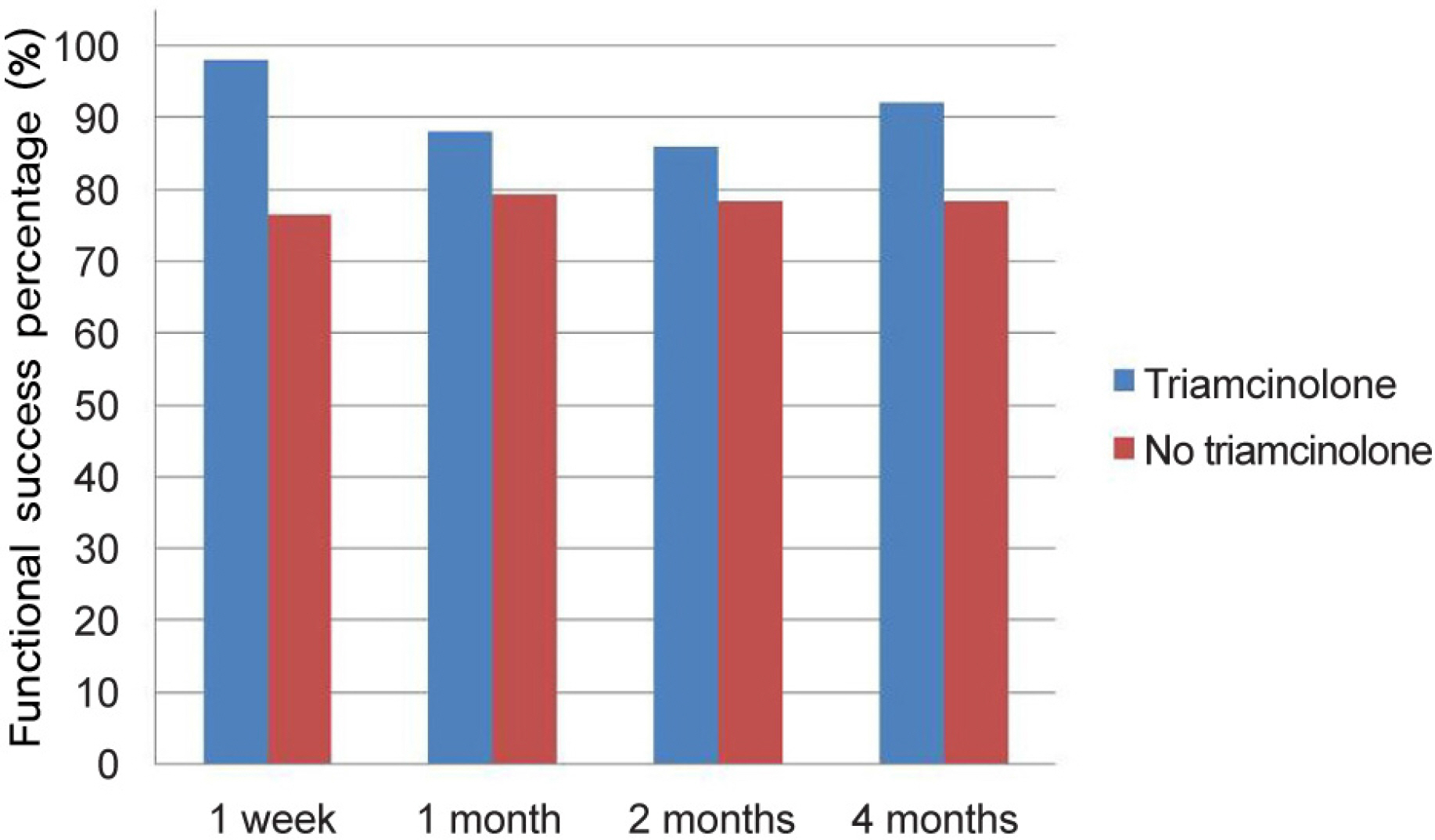
The study included 91 patients (156 eyes) with primary acquired nasolacrimal duct obstruction who underwent endonasal DCR from March 2015 to February 2017. A total of 50 eyes were packed with triamcinolone-soaked Nasopore® and 106 eyes were packed with Nasopore® without triamcinolone (control group). The anatomical and functional success percentage, revision percentage, and postoperative complications such as granulation, synechiae, and membrane formation were compared between the groups at 1 week, 1 month, 2 months, and 4 months postoperatively.
RESULTS
At postoperative 2 months, there was a statistically significant difference in the anatomical success percentage in the triamcinolone-soaked group (100%) compared to the control group (86.8%; p = 0.007). There were no statistically significant differences between the two groups in anatomical success percentage at postoperative 4 months (p > 0.05). However, there was a statistically significant difference in the functional success percentage in the triamcinolone-soaked group (92.0%) compared to the control group (78.3%; p = 0.035). When comparing postoperative complications, the triamcinolone-soaked group (4.0%) had a lower incidence of granulation than the control group (16.0%) (p = 0.032), but there were no differences in synechiae and membrane formation (p > 0.05). There was a statistically significant difference in the revision percentage in the triamcinolone-soaked group (4.0%) compared to the control group (16.0%) (p = 0.032).
CONCLUSIONS
Triamcinolone-soaked nasal packing for endonasal DCR is an effective method for increasing the success percentage and lowering the incidence of granuloma and revision percentages.
MeSH Terms
Figure
Reference
-
1). McDonogh M, Meiring JH. Endoscopic transnasal dacryocystorhinostomy. J Laryngol Otol. 1989; 103:585–7.
Article2). Park JW, Park HY, Yoon KC. Clinical effect of the mixed solution of sodium hyaluronate and sodium carboxymethylcellulose after endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2010; 51:795–801.
Article3). Choi YJ, Hwang SJ, Lee TS. Short-term clinical results of amniotic membrane application to endonasal dacryocystorhinostomy. J Korean Ophthalmol Soc. 2008; 49:384–9.
Article4). Kim JH, Shin JC. Clinical evaluation of endoscopic transnasal dacryocyocystorhinostomy. J Korean Ophthalmol Soc. 1997; 38:1706–11.5). Metson R. Endoscopic surgery for lacrimal obstruction. Otolaryngol Head Neck Surg. 1991; 104:473–9.
Article6). Goldberg RA. Endonasal dacryocystorhinostomy: is it really less successful? Arch Ophthalmol. 2004; 122:108–10.7). Mannor GE, Millman AL. The prognostic value of preoperative dacryocystography in endoscopic intranasal dacryocystorhinostomy. Am J Ophthalmol. 1992; 113:134–7.
Article8). Ali MJ, Wormald PJ, Psaltis AJ. The dacryocystorhinostomy ostium granulomas: classification, indications for treatment, management modalities and outcomes. Orbit. 2015; 34:146–51.
Article9). Li EY, Cheng AC, Wong AC, et al. Safety and efficacy of adjunctive intranasal mitomycin C and triamcinolone in endonasal endoscopic dacryocystorhinostomy. Int Ophthalmol. 2016; 36:105–10.
Article10). Sabarinath V, Harish MR, Divakaran S. Triamcinolone impregnated nasal pack in endoscopic sinus surgery: our experience. Indian J Otolaryngol Head Neck Surg. 2017; 69:88–92.
Article11). Côté DW, Wright ED. Triamcinolone-impregnated nasal dressing following endoscopic sinus surgery: a randomized, double-blind, placebo-controlled study. Laryngoscope. 2010; 120:1269–73.
Article12). Cheng AC, Wong AC, Sze AM, Yuen HK. Limited nasal septoplasty by ophthalmologists during endonasal dacryocystorhinostomy: is it safe? Ophthalmic Plast Reconstr Surg. 2009; 25:293–5.
Article13). Hellebrekers BW, Trimbos-Kemper TC, Trimbos JB, et al. Use of fibrinolytic agents in the prevention of postoperative adhesion formation. Fertil Steril. 2000; 74:203–12.
Article14). Lee TS, Kim SW, Park BW. The relationship between rate of wound healing and success rate after endonasal laser-drill assisted dacryocystorhinostomy. J Korean Ophthalmol Soc. 1999; 40:2969–74.15). Leong M, Phillips LG. Wound healing. Townsend CM, editor. Sabiston Textbook of Surgery. 17th. Philadelphia: WB Saunders;2004. chap. 18.
Article16). Dolmetsch AM. Nonlaser endoscopic endonasal dacryocystorhinostomy with adjunctive mitomycin C in nasolacrimal duct obstruction in adults. Ophthalmology. 2010; 117:1037–40.
Article17). Leibovitch I, Prabhakaran VC, Davis G, Selva D. Intraorbital injection of triamcinolone acetonide in patients with idiopathic orbital inflammation. Arch Ophthalmol. 2007; 125:1647–51.
Article18). Ebner R, Devoto MH, Weil D, et al. Treatment of thyroid associated ophthalmopathy with periocular injections of triamcinolone. Br J Ophthalmol. 2004; 88:1380–6.
Article19). Zeldovich A, Ghabrial R. Revision endoscopic dacryocystorhinostomy with betamethasone injection underassisted local anaesthetic. Orbit. 2009; 28:328–31.20). Xu J, Park SH, Park HS, et al. Effects of triamcinolone-impregnated nasal dressing on subjective and objective outcomes following endoscopic sinus surgery. Eur Arch Otorhinolaryngol. 2016; 273:4351–7.
Article21). Hong SD, Kim JH, Dhong HJ, et al. Systemic effects and safety of triamcinolone-impregnated nasal packing after endoscopic sinus surgery: a randomized, double-blinded, placebo-controlled study. Am J Rhinol Allergy. 2013; 27:407–10.
Article22). Kang IG, Yoon BK, Jung JH, et al. The effect of high-dose topical corticosteroid therapy on prevention of recurrent nasal polyps after revision endoscopic sinus surgery. Am J Rhinol. 2008; 22:497–501.
Article23). More Y, Willen S, Catalano P. Management of early nasal polyposis using a steroid-impregnated nasal dressing. Int Forum Allergy Rhinol. 2011; 1:401–4.
Article24). Jung YH, Lee KH. Effects of triamcinolone-soaked packing for endonasal revision in patients with failed endoscopic dacryocystorhinostomy. J Korean Ophthalmol Soc. 2017; 58:586–90.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effects of Triamcinolone-soaked Packing for Endonasal Revision in Patients with Failed Endoscopic Dacryocystorhinostomy
- Clinical Effects of Guardcel® Nasal Packing on Endonasal Dacryocystorhinostomy
- The Clinical Efficacy of Cutanplast(R) Nasal Packing after Endonasal Dacryocystorhinostomy
- Analysis of the Results Endonasal Dacryocystorhinostomy Related to Nasal Cavity State
- The Effect of Triamcinolone-Soaked Gelfoam in Patients with Polypoid Mucosal Change after Endoscopic Sinus Surgery