J Adv Prosthodont.
2018 Apr;10(2):113-121. 10.4047/jap.2018.10.2.113.
Effects of incorporation of 2.5 and 5 wt% TiOâ‚‚ nanotubes on fracture toughness, flexural strength, and microhardness of denture base poly methyl methacrylate (PMMA)
- Affiliations
-
- 1Foundation of Technical Education, College of Health & Medical Technology, Baghdad, Iraq.
- 2Department of Dental Biomaterials, School of Dentistry, International Campus, Tehran University of Medical Sciences (IC-TUMS), Tehran, Iran. jafarzat@sina.tums.ac.ir
- 3Department of Dental Biomaterials, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.
- 4Dental Research Center, Dentistry Research Institute, Tehran University of Medical Sciences, Tehran, Iran.
- 5Iranian Tissue Bank and Research Center, Tehran University of Medical Sciences, Tehran, Iran.
- 6Department of Biomedical Engineering, Haeri University of Meybod, Yazd, Iran.
- 7Department of Prosthodontics, School of Dentistry, Tehran University of Medical Sciences, Tehran, Iran.
- 8Marquette University School of Dentistry, Milwaukee, USA.
- 9Biomaterials Group, Faculty of Biomedical Engineering, Amirkabir University of Technology (Tehran Polytechnic), Tehran, Iran.
- 10Dentist In Private Practice, Tehran, Iran.
- KMID: 2409630
- DOI: http://doi.org/10.4047/jap.2018.10.2.113
Abstract
- PURPOSE
The aim of this preliminary study was to investigate, for the first time, the effects of addition of titania nanotubes (n-TiO2) to poly methyl methacrylate (PMMA) on mechanical properties of PMMA denture base.
MATERIALS AND METHODS
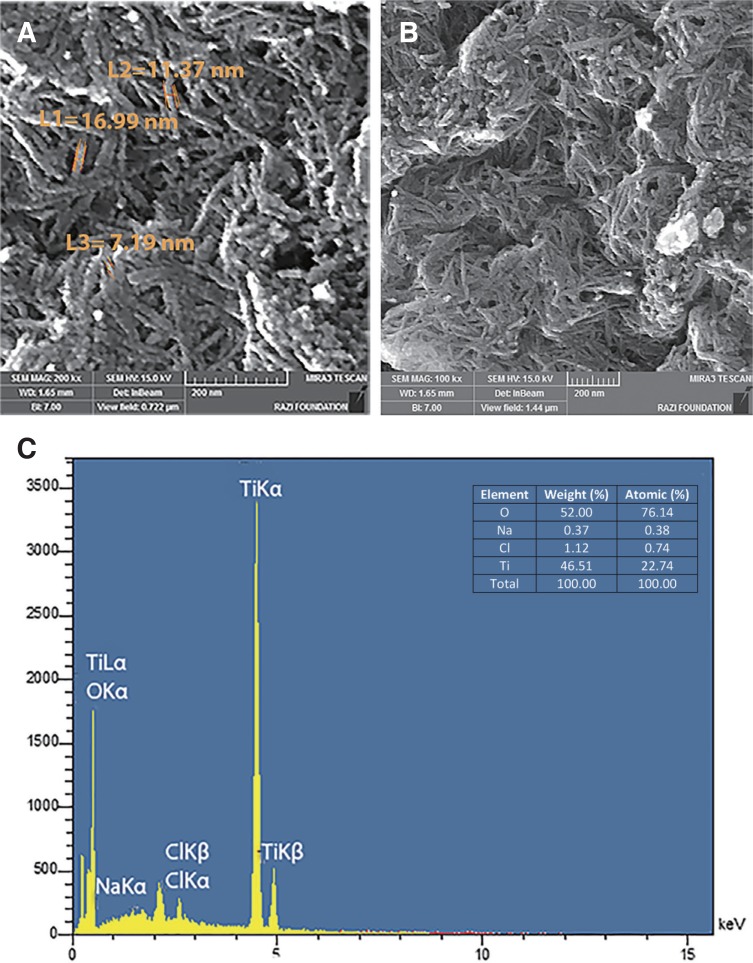
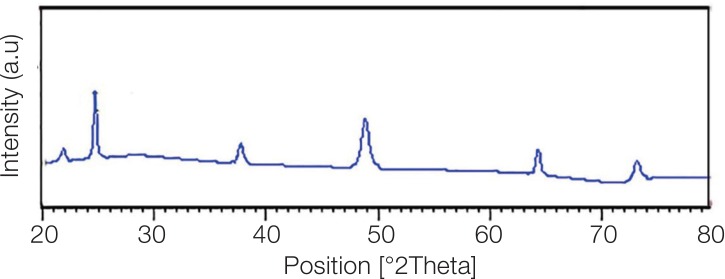
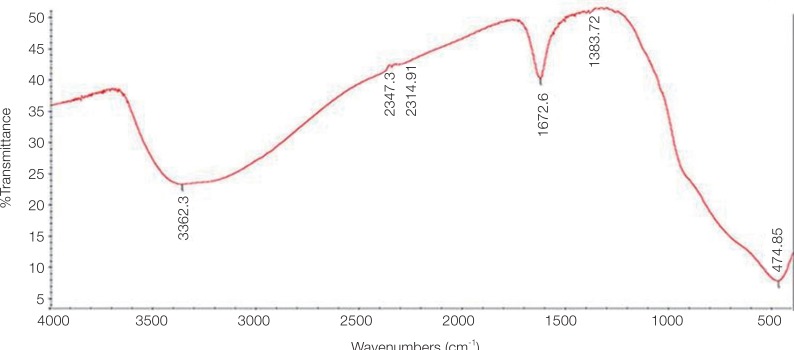
TiO2 nanotubes were prepared using alkaline hydrothermal process. Obtained nanotubes were assessed using FESEM-EDX, XRD, and FT-IR. For 3 experiments of this study (fracture toughness, three-point bending flexural strength, and Vickers microhardness), 135 specimens were prepared according to ISO 20795-1:2013 (n of each experiment=45). For each experiment, PMMA was mixed with 0% (control), 2.5 wt%, and 5 wt% nanotubes. From each TiO2:PMMA ratio, 15 specimens were fabricated for each experiment. Effects of n-TiO2 addition on 3 mechanical properties were assessed using Pearson, ANOVA, and Tukey tests.
RESULTS
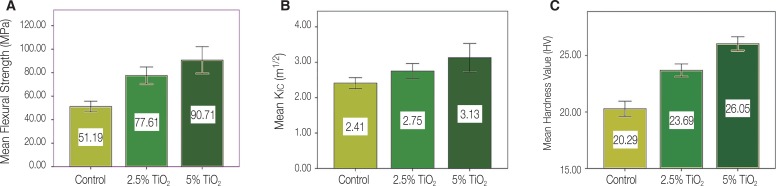
SEM images of n-TiO2 exhibited the presence of elongated tubular structures. The XRD pattern of synthesized n-TiO2 represented the anatase crystal phase of TiO2. Moderate to very strong significant positive correlations were observed between the concentration of n-TiO2 and each of the 3 physicomechanical properties of PMMA (Pearson's P value ≤.001, correlation coefficient ranging between 0.5 and 0.9). Flexural strength and hardness values of specimens modified with both 2.5 and 5 wt% n-TiO2 were significantly higher than those of control (P≤.001). Fracture toughness of samples reinforced with 5 wt% n-TiO2 (but not those of 2.5% n-TiO2) was higher than control (P=.002).
CONCLUSION
Titania nanotubes were successfully introduced for the first time as a means of enhancing the hardness, flexural strength, and fracture toughness of denture base PMMA.
Keyword
Figure
Reference
-
1. Peyton FA. History of resins in dentistry. Dent Clin North Am. 1975; 19:211–222. PMID: 1090459.2. Johnston EP, Nicholls JI, Smith DE. Flexure fatigue of 10 commonly used denture base resins. J Prosthet Dent. 1981; 46:478–483. PMID: 6946217.
Article3. Jagger DC, Harrison A, Jandt KD. The reinforcement of dentures. J Oral Rehabil. 1999; 26:185–194. PMID: 10194725.
Article4. Karacaer O, Dogan OM, Tinçer T, Dogan A. Reinforcement of maxillary dentures with silane-treated ultra high modulus polyethylene fibers. J Oral Sci. 2001; 43:103–107. PMID: 11515593.
Article5. Kim SH, Watts DC. The effect of reinforcement with woven E-glass fibers on the impact strength of complete dentures fabricated with high-impact acrylic resin. J Prosthet Dent. 2004; 91:274–280. PMID: 15060499.
Article6. Vallittu PK. Glass fiber reinforcement in repaired acrylic resin removable dentures: preliminary results of a clinical study. Quintessence Int. 1997; 28:39–44. PMID: 10332353.7. Vojdani M, Giti R. Polyamide as a denture base material: A literature review. J Dent (Shiraz). 2015; 16:1–9.8. John J, Gangadhar SA, Shah I. Flexural strength of heat-polymerized polymethyl methacrylate denture resin reinforced with glass, aramid, or nylon fibers. J Prosthet Dent. 2001; 86:424–427. PMID: 11677538.
Article9. Ruffino AR. Effect of steel strengtheners on fracture resistance of the acrylic resin complete denture base. J Prosthet Dent. 1985; 54:75–78. PMID: 3894643.
Article10. Vallittu PK. A review of methods used to reinforce polymethyl methacrylate resin. J Prosthodont. 1995; 4:183–187. PMID: 8603209.
Article11. Sehajpal SB, Sood VK. Effect of metal fillers on some physical properties of acrylic resin. J Prosthet Dent. 1989; 61:746–751. PMID: 2724170.
Article12. Asar NV, Albayrak H, Korkmaz T, Turkyilmaz I. Influence of various metal oxides on mechanical and physical properties of heat-cured polymethyl methacrylate denture base resins. J Adv Prosthodont. 2013; 5:241–247. PMID: 24049564.
Article13. Guo Z, Tan L. Fundamentals and applications of nanomaterials. Artech House;2009.14. Wang R, Kayacan R, Küçükeşmen C. Nanotubes/polymethyl methacrylate composite resins as denture base materials. Carbon Nanomater Biomed Appl. 2016; 227–240.
Article15. Wang R, Tao J, Yu B, Dai L. Characterization of multiwalled carbon nanotube-polymethyl methacrylate composite resins as denture base materials. J Prosthet Dent. 2014; 111:318–326. PMID: 24360009.
Article16. Yu W, Wang X, Tang Q, Guo M, Zhao J. Reinforcement of denture base PMMA with ZrO(2) nanotubes. J Mech Behav Biomed Mater. 2014; 32:192–197. PMID: 24487077.17. Abdallah RM. Evaluation of polymethyl methacrylate resin mechanical properties with incorporated halloysite nanotubes. J Adv Prosthodont. 2016; 8:167–171. PMID: 27350849.
Article18. Shirkavand S, Moslehifard E. Effect of TiO2 Nanoparticles on Tensile Strength of Dental Acrylic Resins. J Dent Res Dent Clin Dent Prospects. 2014; 8:197–203. PMID: 25587380.19. Ahmed MA, El-Shennawy M, Althomali YM, Omar A. Effect of titanium dioxide nano particles incorporation on mechanical and physical properties on two different types of acrylic resin denture base. World J Nano Sci Eng. 2016; 6:111–119.20. Li Z, Sun J, Lan J, Qi Q. Effect of a denture base acrylic resin containing silver nanoparticles on Candida albicans adhesion and biofilm formation. Gerodontology. 2016; 33:209–216. PMID: 25070079.21. Wady AF, Machado AL, Zucolotto V, Zamperini CA, Berni E, Vergani CE. Evaluation of Candida albicans adhesion and biofilm formation on a denture base acrylic resin containing silver nanoparticles. J Appl Microbiol. 2012; 112:1163–1172. PMID: 22452416.
Article22. Elshereksi NW, Ghazali MJ, Muchtar A, Azhari CH. Perspectives for titanium-derived fillers usage on denture base composite construction: A review article. Advances in Materials Science and Engineering [Internet]. Hindawi Limited;2014. 2014:p. 1–13. Available from: http://dx.doi.org/10.1155/2014/746252.23. Bavykin DV, Walsh FC. Titanate and titania nanotubes: Synthesis, properties and applications. 1st ed. Cambridge, UK: Royal Society of Chemistry, (RCS Nanoscience & Nanotechnology);2010.24. Kasuga T, Hiramatsu , Hoson A, Sekino T, Niihara K. Formation of titanium oxide nanotube. Langmuir. 1998; 14:3160–3163.
Article25. Indira K, Kamachi Mudali U, Nishimura T, Rajendran N. A review on TiO2 nanotubes: influence of anodization parameters, formation mechanism, properties, corrosion behavior, and biomedical applications. J Bio Tribo Corros. 2015; 1:28.
Article26. Jia Y, Kleinhammes A, Kulkarni H, McGuire K, McNeil LE, Wu Y. Synthesis and characterization of TiO2 nanotube/hydroquinone hybrid structure. J Nanosci Nanotechnol. 2007; 7:458–462. PMID: 17450779.27. Jia Y, Kleinhammes A, Kulkarni H, McGuire K, McNeil LE, Wu Y. Synthesis and characterization of TiO2 nanotube/hydroquinone hybrid structure. J Nanosci Nanotechnol. 2007; 7:458–462. PMID: 17450779.28. Michele TB, Joseph EM, Mathew B, Rowan B, Gun'ko YK, Horváth E, Zoltán K, Kukovecz A, Imre K, Jonathan NC. Chemical functionalisation of titania nanotubes and their utilisation for the fabrication of reinforced polystyrene composites. J Mater Chem. 2007; 17:2351–2358.29. Porras R, Bavykin DV, Zekonyte J, Walsh FC, Wood RJ. Titanate nanotubes for reinforcement of a poly(ethylene oxide)/ chitosan polymer matrix. Nanotechnology. 2016; 27:195706. PMID: 27039947.30. Khaled SM, Miron RJ, Hamilton DW, Charpentier PA, Rizkalla AS. Reinforcement of resin based cement with titania nanotubes. Dent Mater. 2010; 26:169–178. PMID: 19914706.
Article31. Dafar MO, Grol MW, Canham PB, Dixon SJ, Rizkalla AS. Reinforcement of flowable dental composites with titanium dioxide nanotubes. Dent Mater. 2016; 32:817–826. PMID: 27059772.
Article32. Khaled SM, Charpentier PA, Rizkalla AS. Synthesis and characterization of poly(methyl methacrylate)-based experimental bone cements reinforced with TiO2-SrO nanotubes. Acta Biomater. 2010; 6:3178–3186. PMID: 20170759.33. Hamouda IM, Beyari MM. Addition of glass fibers and titanium dioxide nanoparticles to the acrylic resin denture base material: comparative study with the conventional and high impact types. Oral Health Dent Manag. 2014; 13:107–112. PMID: 24603926.34. Sodagar A, Bahador A, Khalil S, Shahroudi AS, Kassaee MZ. The effect of TiO2 and SiO2 nanoparticles on flexural strength of poly (methyl methacrylate) acrylic resins. J Prosthodont Res. 2013; 57:15–19. PMID: 23200530.35. Eslami H, Moztarzadeh F, Jafarzadeh Kashi TS, Khoshroo K, Tahriri M. Hydrothermal synthesis and characterization of TiO2-derived nanotubes for biomedical applications. Synth Reactivity Inorg Met-Org Nano-Met Chem. 2016; 46:1149–1156.36. ISO 20795-1. Dentistry - Base polymers - Part 1: Denture base polymers. 2013.37. Gandhi N, Daniel S, Benjamin S, Kurian N, Varghese VS. Evaluation of surface microhardness following chemical and microwave disinfection of commercially available acrylic resin denture teeth. J Clin Diagn Res. 2017; 11:ZC87–ZC91.
Article38. Mathew M, Shenoy K, Ravishankar K. Vickers hardness and specific wear rate of poly propylene reinforced PMMA. Int J Sci Study. 2014; 2:71–75.39. Khoshroo K, Jafarzadeh Kashi TS, Moztarzadeh F, Eslami H, Tahriri M. The influence of calcination temperature on the structural and biological characteristics of hydrothermally synthesized TiO2 nanotube: In vitro study. Synth Reactivity Inorg Met-Org Nano-Met Chem. 2016; 46:1189–1194.40. Edwin TM, Reuben S, Vincent ON, Patrick GN. Multiwalled carbon nanotube-titania nanocomposites: Understanding nano-structural parameters and functionality in dye-sensitized solar cells. S Afr J Chem. 2015; 68:153–164.
Article41. Bagheri S, Shameli K, Abd Hamid SB. Synthesis and characterization of anatase titanium dioxide nanoparticles using egg white solution via Sol-Gel method. J Chem. 2013; 848205.
Article42. Yu JC, Zhang L, Zheng Z, Zhao J. Synthesis and characterization of phosphated mesoporous titanium dioxide with high photocatalytic activity. Chem Mater. 2003; 15:2280–2286.
Article43. Zhang S, Peng LM, Chen Q, Du GH, Dawson G, Zhou WZ. Formation mechanism of H2Ti3O7 nanotubes. Phys Rev Lett. 2003; 91:256103. PMID: 14754129.44. Zappini G, Kammann A, Wachter W. Comparison of fracture tests of denture base materials. J Prosthet Dent. 2003; 90:578–585. PMID: 14668759.
Article45. Hill RG, Bates JF, Lewis TT, Rees N. Fracture toughness of acrylic denture base. Biomaterials. 1983; 4:112–120. PMID: 6860751.
Article46. Al-Haddad A, Vahid Roudsari R, Satterthwaite JD. Fracture toughness of heat cured denture base acrylic resin modified with Chlorhexidine and Fluconazole as bioactive compounds. J Dent. 2014; 42:180–184. PMID: 24269832.
Article47. Mecholsky JJ Jr. Fractography: determining the sites of fracture initiation. Dent Mater. 1995; 11:113–116. PMID: 8621031.
Article48. Soderholm KJ. Review of the fracture toughness approach. Dent Mater. 2010; 26:e63–e77. PMID: 20045178.
Article49. Stafford GD, Huggett R, Causton BE. Fracture toughness of denture base acrylics. J Biomed Mater Res. 1980; 14:359–371. PMID: 7400192.
Article50. Feng P, Gao C, Shuai C, Peng S. Toughening and strengthening mechanisms of porous akermanite scaffolds reinforced with nano-titania. RSC Adv. 2015; 5:3498–3507.
Article51. Arash B, Wang Q, Varadan VK. Mechanical properties of carbon nanotube/polymer composites. Sci Rep. 2014; 4:1–8.
Article52. Salehian H, Jenabali Jahromi SH. Effect of titanium dioxide nanoparticles on mechanical properties of vinyl ester-based nanocomposites. J Compos Mater. 2015; 49:2365–2373.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of polymethyl methacrylate resin mechanical properties with incorporated halloysite nanotubes
- Comparison of flexural strength according to thickness between CAD/CAM denture base resins and conventional denture base resins
- A Study on The Flexural Bond Strength of The Gold and The Co-Cr Alloy To The Denture Base Resins
- The Effects Of Thermocycling On The Bond Strength Between Cobalt-Chromium Alloy And Denture Base Resin
- EFFECTS OF CHOPPED GLASS FIBER ON THE STRENGTH OF HEAT-CURED PMMA RESIN