Perinatology.
2017 Dec;28(4):146-150. 10.14734/PN.2017.28.4.146.
Neonatal Outcome according to Birth Order in Triplets: A Comparative Study with Twins and Singletons
- Affiliations
-
- 1Department of Pediatrics, Cheil General Hospital & Women's Health Care Center, Dankook University College of Medicine, Seoul, Korea. ykleeped@hanmail.net
- KMID: 2409122
- DOI: http://doi.org/10.14734/PN.2017.28.4.146
Abstract
OBJECTIVE
To evaluate the neonatal outcome of triplets and compare the results of twins and singletons with those of triplets.
METHODS
From 2004 to 2015, we reviewed medical records of triplets who were delivered in a single center. We investigated clinical characteristics and neonatal outcome according to the birth order in triplets, and compared those of twins and singletons who were gestational age-matched and born preceding and following the birth of each triplet.
RESULTS
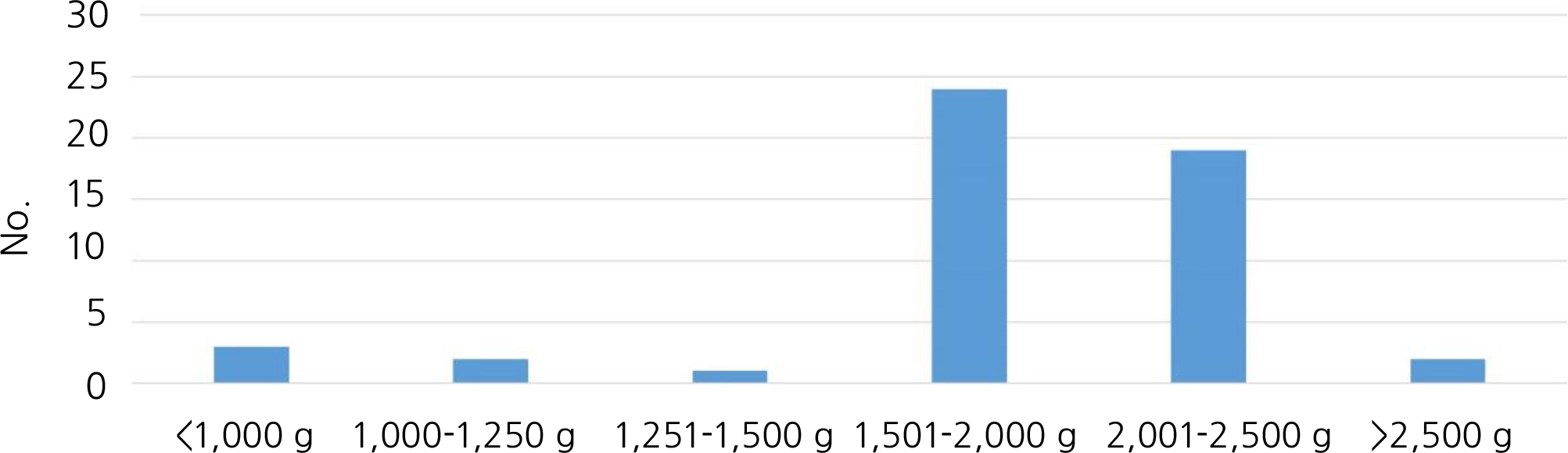
Seventeen sets of triplet (51 neonates) were born during the reviewed 12-year period and the incidence of triplets was 0.06%. All triplets were born between 26+5 weeks and 35+2 weeks, the mean gestational age was 33.1±2.6 weeks, and the mean birth weight was 1,805.4±409.0 g. According to the birth order, the mean birth weight of first, second, and third babies was 1,862.6± 298.1 g, 1,788.7±277.7 g, and 1,765.3±273.5 g respectively, although there was no significant difference. Also there was no difference in respiratory distress syndrome, bronchopulmonary dysplasia, apnea, patent ductus arteriosus, intraventricular hemorrhage, periventricular leukomalacia and retinopathy of prematurity among the three groups. In a comparative study of triplets to twins and singletons, there was no difference in neonatal outcome except birth weight (triplets vs. twins: 1,805.4 ±409.0 g vs. 1,960.3±441.0 g, P=0.068, triplets vs. singletons: 1,805.4±409.0 g vs. 2,087.8± 522.1 g, P < 0.001).
CONCLUSION
There was no influence of the birth order on birth weight and neonatal outcome of triplets. Neonatal outcome of triplets was not different to that of twins and singletons except birth weight of triplets to singletons in a gestational age-matched study.
MeSH Terms
Figure
Reference
-
1). Korean Statistical Information Service. Annual report on live births and deaths statistics. [accessed on 1 July 2017]. Available at. http://kosis.kr/ups/ups_01List.jsp?pubcode=CC.2). Centers for Disease Control and Prevention. QuickStats: Mean Gestational Age, by Plurality. [accessed on 1 July 2017]. Available at. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5709a9.htm.3). Stahlman M., Hedvall G., Dolanski E., Faxelius G., Burko H., Kirk V. A six-year follow-up of clinical hyaline membrane disease. Pediatr Clin North Am. 1973. 20:433–46.
Article4). Jobe AH., Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001. 163:1723–9.
Article5). Papile LA., Burstein J., Burstein R., Koffler H. Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr. 1978. 92:529–34.
Article6). Aabera T., Ben-Sira I., Charled S., Clarkson J., Cohen BZ., Flynn J, et al. An international classification of retinopathy of prematurity: II. The classification of retinal detachment. Arch Ophthalmol. 1987. 105:906–12.7). Cassell KA., O'connell CM., Baskett TF. The origins and outcomes of triplet and quadruplet pregnancies in Nova Scotia: 1980 to 2001. Am J Perinatol. 2004. 21:439–45.
Article8). Centers for Disease Control and Prevention. Final Data for 2015. National Vital Statistics Reports. [accessed on 1 July 2017]. Available at. http://www.cdc.gov/nchs/births.htm.9). Ballabh P., Kumari J., AlKouatly HB., Yih M., Arevalo R., Rosenwaks Z, et al. Neonatal outcome of triplet versus twin and singleton pregnancies: a matched case control study. Eur J Obstet Gynecol Reprod Biol. 2003. 107:28–36.
Article10). Chae SJ., Yoo WJ., Kang KH., Kim BJ., Lee SE., Sohn YK, et al. Perinatal outcomes of triplet pregnancies. Korean J Obstet Gynecol. 2006. 49:1051–9.11). Orlebeke JF., Boomsma DI., Eriksson AW. Epidemiological and birth weight characteristics of triplets: a study from the Dutch twin register. Eur J Obstet Gynecol Reprod Biol. 1993. 50:87–93.
Article12). Ho ML., Chen JY., Ling UP., Chen JH., Huang CM., Chang CC, et al. Changing epidemiology of triplet pregnancy: etiology and outcome over twelve years. Am J Perinatol. 1996. 13:269–75.
Article13). Loucopoulos A., Jewelewicz R. Management of multifetal pregnancies: sixteen years' experience at the Sloane Hospital for Women. Am J Obstet Gynecol. 1982. 143:902–5.
Article14). Alran S., Sibony O., Luton D., Touitou S., Fourchotte V., Féraud O, et al. Maternal and neonatal outcome of 93 consecutive triplet pregnancies with 71% vaginal delivery. Acta Obstet Gynecol Scand. 2004. 83:554–9.
Article15). Güngör ES., Tapısız ÖL., Aytan H., Danışman N., Kalyoncu Ş., Mollamahmutoğlu L. Maternal and neonatal outcome of triplet versus twin and singleton pregnancies. Gazi Med J. 2006. 17:45–48.16). Choi CI., Chung IB., Oh GY., Choi KD., Choi HI., Han HD, et al. Maternal and perinatal outcomes in triplet versus twin pregnancies with the result of Assisted Reproductive Technology. Korean J Obstet Gynecol. 1999. 42:2013–8.