Ann Hepatobiliary Pancreat Surg.
2018 Feb;22(1):75-78. 10.14701/ahbps.2018.22.1.75.
Right adrenal gland pseudocyst masquerading as a large symptomatic hepatic cyst: Single incision laparoscopic (SILS) resection and a review of current literature
- Affiliations
-
- 1Department of Surgery, University Surgical Cluster, National University Hospital, Singapore, Singapore.
- 2Department of Pathology, National University Hospital, Singapore, Singapore.
- 3Division of Hepatobiliary and Pancreatic Surgery and Liver Transplantation, Department of Surgery, University Surgical Cluster, National University Hospital, Singapore, Singapore. alfred_kow@nuhs.edu.sg
- KMID: 2409083
- DOI: http://doi.org/10.14701/ahbps.2018.22.1.75
Abstract
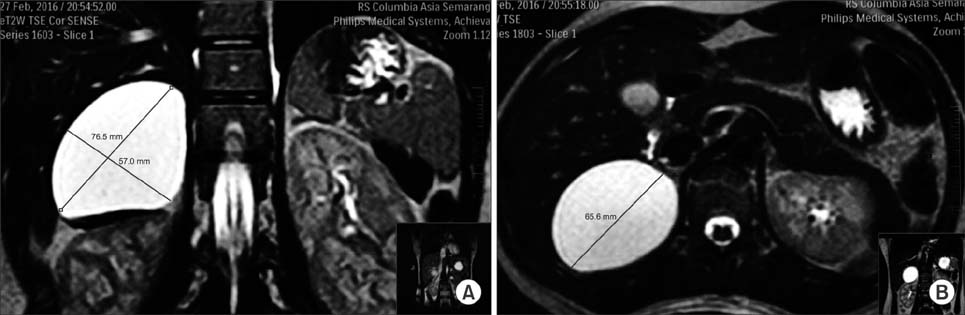
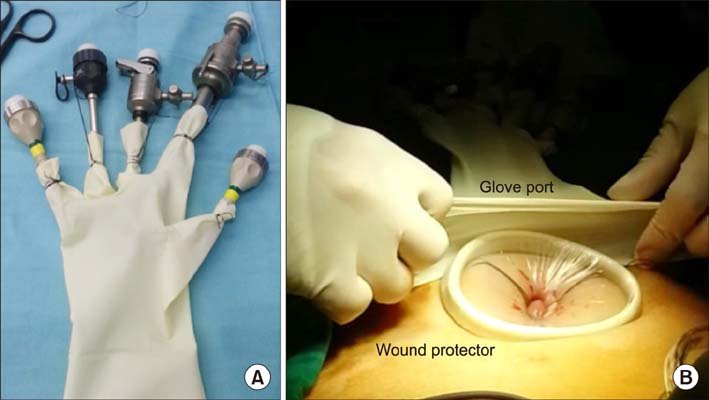
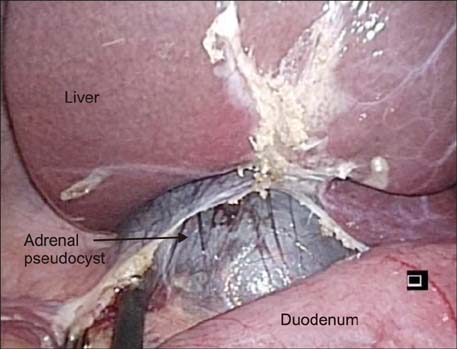
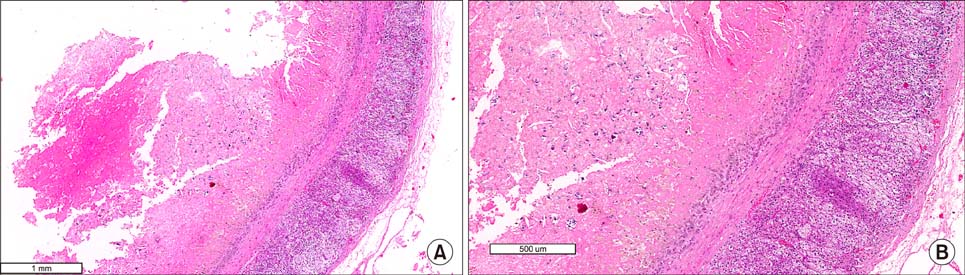
- Adrenal pseudocysts are rare entities, which are usually asymptomatic. Large symptomatic adrenal pseudocysts may cause compressive symptoms. The etiology of these cysts is unknown, although the cyst wall is all lined by fibrous tissue, without any epithelial or endothelial lining. We report a case of a 26-year-old lady who presented with a symptomatic right adrenal pseudocyst measuring 7.6 cm in size. Magnetic resonance imaging confirmed the presence of a right retroperitoneal cystic lesion which was hyperintense on T2 sequencing. An attempted single incision transumbilical laparoscopic surgery (SILS) was performed to excise the right adrenal pseudocyst. However, due to the retro-hepatic nature of the lesion and as the medial wall of the cyst was adherent to the inferior vena cava, an additional 5 mm port was inserted to facilitate retraction of the liver. The post-operative period was uneventful. She was successfully discharged from the hospital as a day surgery patient. The final pathology showed an adrenal pseudocyst.
Keyword
MeSH Terms
Figure
Reference
-
1. Tagge DU, Baron PL. Giant adrenal cyst: management and review of the literature. Am Surg. 1997; 63:744–746.2. Kim BS, Joo SH, Choi SI, Song JY. Laparoscopic resection of an adrenal pseudocyst mimicking a retroperitoneal mucinous cystic neoplasm. World J Gastroenterol. 2009; 15:2923–2926.
Article3. Gaffey MJ, Mills SE, Fechner RE, Bertholf MF, Allen MS Jr. Vascular adrenal cysts. A clinicopathologic and immunohistochemical study of endothelial and hemorrhagic (pseudocystic) variants. Am J Surg Pathol. 1989; 13:740–747.4. Medeiros LJ, Lewandrowski KB, Vickery AL Jr. Adrenal pseudocyst: a clinical and pathologic study of eight cases. Hum Pathol. 1989; 20:660–665.
Article5. AsalZare M, Shakiba B, Asadpour AA, Ghoreifi A. Laparoscopic management of symptomatic giant adrenal pseudocyst: a case report. Urol J. 2014; 11:1517–1520.6. Habra MA, Feig BW, Waguespack SG. Image in endocrinology: adrenal pseudocyst. J Clin Endocrinol Metab. 2005; 90:3067–3068.7. Khilnani GC, Kumar A, Bammigatti C, Sharma R, Gupta SD. Hemorrhagic pseudocyst of the adrenal gland causing acute abdominal pain. J Assoc Physicians India. 2008; 56:379–380.8. Hasson HM. A modified instrument and method for laparoscopy. Am J Obstet Gynecol. 1971; 110:886–887.
Article9. Davenport M, Pollard K, Smith SE, MacMahon MJ. Adrenal cysts--report, review and classification. Postgrad Med J. 1988; 64:71–73.
Article10. Ghandur-Mnaymneh L, Slim M, Muakassa K. Adrenal cysts: pathogenesis and histological identification with a report of 6 cases. J Urol. 1979; 122:87–91.
Article11. Khoda J, Hertzanu Y, Sebbag G, Lantsberg L, Barky Y. Adrenal cysts: diagnosis and therapeutic approach. Int Surg. 1993; 78:239–242.12. Gagner M, Lacroix A, Bolté E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. N Engl J Med. 1992; 327:1033.
Article13. Haveran LA, Novitsky YW, Czerniach DR, Kaban GK, Kelly JJ, Litwin DE. Benefits of laparoscopic adrenalectomy: a 10-year single institution experience. Surg Laparosc Endosc Percutan Tech. 2006; 16:217–221.
Article14. Wang HS, Li CC, Chou YH, Wang CJ, Wu WJ, Huang CH. Comparison of laparoscopic adrenalectomy with open surgery for adrenal tumors. Kaohsiung J Med Sci. 2009; 25:438–444.
Article15. Maccabee DL, Jones A, Domreis J, Deveney CW, Sheppard BC. Transition from open to laparoscopic adrenalectomy: the need for advanced training. Surg Endosc. 2003; 17:1566–1569.16. Shi TP, Zhang X, Ma X, Li HZ, Zhu J, Wang BJ, et al. Laparoendoscopic single-site retroperitoneoscopic adrenalectomy: a matched-pair comparison with the gold standard. Surg Endosc. 2011; 25:2117–2124.
Article17. Hora M, Ürge T, Stránský P, Trávníček I, Pitra T, Kalusová K, et al. Laparoendoscopic single-site surgery adrenalectomy - own experience and matched case-control study with standard laparoscopic adrenalectomy. Wideochir Inne Tech Maloinwazyjne. 2014; 9:596–602.
Article18. Hirano D, Hasegawa R, Igarashi T, Satoh K, Mochida J, Takahashi S, et al. Laparoscopic adrenalectomy for adrenal tumors: a 21-year single-institution experience. Asian J Surg. 2015; 38:79–84.
Article19. Kwak HN, Kim JH, Yun JS, Son BH, Chung WY, Park YL, et al. Conventional laparoscopic adrenalectomy versus laparoscopic adrenalectomy through mono port. Surg Laparosc Endosc Percutan Tech. 2011; 21:439–442.
Article20. Ishida M, Miyajima A, Takeda T, Hasegawa M, Kikuchi E, Oya M. Technical difficulties of transumbilical laparoendoscopic single-site adrenalectomy: comparison with conventional laparoscopic adrenalectomy. World J Urol. 2013; 31:199–203.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pyogenic Adrenal Cyst in Newborn
- Repeat Single Incision Laparoscopic Surgery after Primary Single Incision Laparoscopic Surgery for Colorectal Disease
- A case of infected adrenal pseudocyst
- Endothelial Cyst of the Adrenal Gland: Report of a case
- Postoperative Pain Relief Using Wound Infiltration With 0.5% Bupivacaine in Single-Incision Laparoscopic Surgery for an Appendectomy