Hip Pelvis.
2018 Mar;30(1):29-36. 10.5371/hp.2018.30.1.29.
Effectiveness of Endoscopic Sciatic Nerve Decompression for the Treatment of Deep Gluteal Syndrome
- Affiliations
-
- 1Department of Orthopaedic Surgery, St. Carollo Hospital, Suncheon, Korea. wctoilets@hanmail.net
- KMID: 2408183
- DOI: http://doi.org/10.5371/hp.2018.30.1.29
Abstract
- PURPOSE
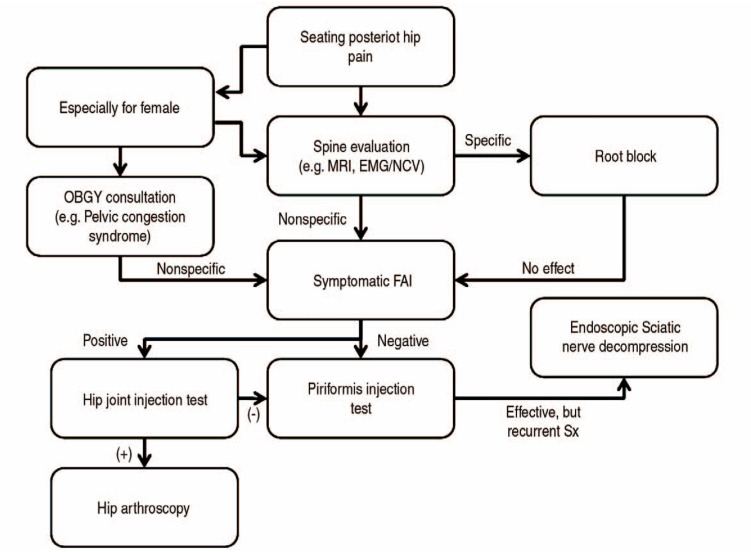
The purpose of this retrospective study was to evaluate clinical outcomes of endoscopic nerve decompression in patients with deep gluteal syndromes (DGS).
MATERIALS AND METHODS
Between October 2013 and March 2015, 24 patients who underwent surgical treatment of DGS were retrospectively included in this study. The mean age was 47 years (range, 35 to 76 years), and there were 11 males and 13 females. The mean duration of pain was 12 months (range, 5 to 35 months) and the mean follow-up period was 32 months (range, 26 to 45 months). Clinical evaluations included the visual analog scale (VAS) pain score, modified Harris hip score (mHHS), and the symptom-rating scale.
RESULTS
Significant improvement in symptoms following endoscopic decompression were achieved as measured using the VAS score (decrease in the mean from 7.1±0.9 to 2.5±1.5; P < 0.001) and mHHS (increase from 59.4±6.5 to 85.0±8.3; P < 0.001).
CONCLUSION
Endoscopic sciatic nerve decompression was satisfactory for treating recalcitrant DGS, making it an effective treatment option to improve symptoms of DGS.
MeSH Terms
Figure
Reference
-
1. Hernando MF, Cerezal L, Pérez-Carro L, Abascal F, Canga A. Deep gluteal syndrome: anatomy, imaging, and management of sciatic nerve entrapments in the subgluteal space. Skeletal Radiol. 2015; 44:919–934. PMID: 25739706.
Article2. Martin HD, Reddy M, Gómez-Hoyos J. Deep gluteal syndrome. J Hip Preserv Surg. 2015; 2:99–107. PMID: 27011826.
Article3. Hopayian K, Song F, Riera R, Sambandan S. The clinical features of the piriformis syndrome: a systematic review. Eur Spine J. 2010; 19:2095–2109. PMID: 20596735.
Article4. Park MS, Yoon SJ, Jung SY, Kim SH. Clinical results of endoscopic sciatic nerve decompression for deep gluteal syndrome: mean 2-year follow-up. BMC Musculoskelet Disord. 2016; 17:218. PMID: 27206482.
Article5. Martin HD, Kivlan BR, Palmer IJ, Martin RL. Diagnostic accuracy of clinical tests for sciatic nerve entrapment in the gluteal region. Knee Surg Sports Traumatol Arthrosc. 2014; 22:882–888. PMID: 24217716.
Article6. Filler AG, Haynes J, Jordan SE, et al. Sciatica of nondisc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine. 2005; 2:99–115. PMID: 15739520.
Article7. Boyajian-O'Neill LA, McClain RL, Coleman MK, Thomas PP. Diagnosis and management of piriformis syndrome: an osteopathic approach. J Am Osteopath Assoc. 2008; 108:657–664. PMID: 19011229.8. Benson ER, Schutzer SF. Posttraumatic piriformis syndrome: diagnosis and results of operative treatment. J Bone Joint Surg Am. 1999; 81:941–949. PMID: 10428125.9. Martin HD, Shears SA, Johnson JC, Smathers AM, Palmer IJ. The endoscopic treatment of sciatic nerve entrapment/deep gluteal syndrome. Arthroscopy. 2011; 27:172–181. PMID: 21071168.
Article10. Papadopoulos EC, Khan SN. Piriformis syndrome and low back pain: a new classification and review of the literature. Orthop Clin North Am. 2004; 35:65–71. PMID: 15062719.
Article11. Pace JB, Nagle D. Piriform syndrome. West J Med. 1976; 124:435–439. PMID: 132772.12. Freiberg AH. Sciatic pain and its relief by operations on muscle and fascia. Arch Surg. 1937; 34:337–350.
Article13. Coppieters MW, Alshami AM, Babri AS, Souvlis T, Kippers V, Hodges PW. Strain and excursion of the sciatic, tibial, and plantar nerves during a modified straight leg raising test. J Orthop Res. 2006; 24:1883–1889. PMID: 16838375.
Article14. Cox JM, Bakkum BW. Possible generators of retrotrochanteric gluteal and thigh pain: the gemelli-obturator internus complex. J Manipulative Physiol Ther. 2005; 28:534–538. PMID: 16182029.
Article15. Meknas K, Christensen A, Johansen O. The internal obturator muscle may cause sciatic pain. Pain. 2003; 104:375–380. PMID: 12855348.
Article16. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000; 16:578–587. PMID: 10976117.
Article17. Beaton LE, Anson BJ. The sciatic nerve and the piriformis muscle: their interrelation a possible cause of coccygodynia. J Bone Joint Surg Am. 1938; 20:686–688.18. Kitagawa Y, Yokoyama M, Tamai K, Takai S. Chronic expanding hematoma extending over multiple gluteal muscles associated with piriformis syndrome. J Nippon Med Sch. 2012; 79:478–483. PMID: 23291848.
Article19. Issack PS, Kreshak J, Klinger CE, Toro JB, Buly RL, Helfet DL. Sciatic nerve release following fracture or reconstructive surgery of the acetabulum. Surgical technique. J Bone Joint Surg Am. 2008; 90(Suppl 2):227–237. PMID: 18829936.20. Beauchesne RP, Schutzer SF. Myositis ossificans of the piriformis muscle: an unusual cause of piriformis syndrome. A case report. J Bone Joint Surg Am. 1997; 79:906–910. PMID: 9199390.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Transgluteal Approach for Decompression of Sciatic Nerve Entrapment (Piriformis Syndrome) with Intraoperative Neurophysiology: A Technical Note
- Complex Variations in the Course of the Sciatic Nerve and Origin of the Inferior Gluteal Nerve: A Case Report
- Sciatic Nerve Palsy Complicating Gluteal Compartment Syndrome due to Rhabdomyolysis: A Case Report
- Arthroscopic Treatment of Secondary Piriformis Syndrome by Perineural Cyst on the Sciatic Nerve: A Case Report
- Piriformis Syndrome (Sciatic Nerve Entrapment) Associated With Type C Sciatic Nerve Variation: A Report of Two Cases and Literature Review