Ann Lab Med.
2018 Jul;38(4):291-295. 10.3343/alm.2018.38.4.291.
Principles of Genetic Counseling in the Era of Next-Generation Sequencing
- Affiliations
-
- 1Department of Laboratory Medicine and Genetics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. kimjw@skku.edu
- KMID: 2408067
- DOI: http://doi.org/10.3343/alm.2018.38.4.291
Abstract
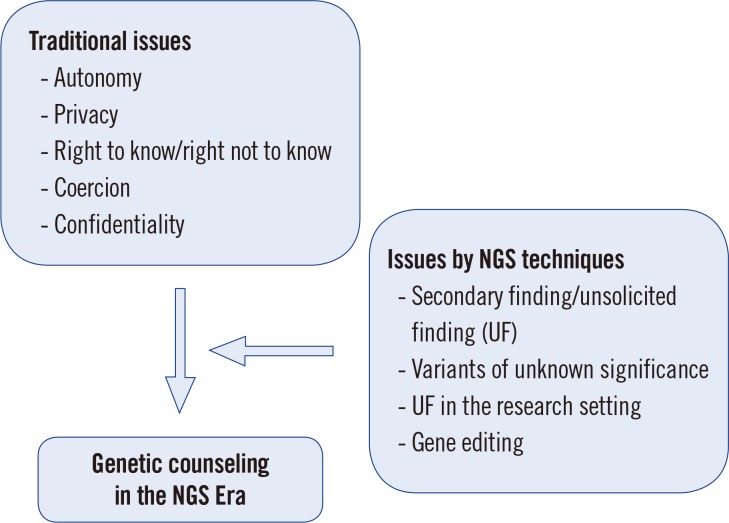
- Traditional genetic counseling has focused on the target gene and its natural progress with respect to disease risk. Next-generation sequencing (NGS) can produce information on several genetic variants simultaneously, with different functions and consequences for each. Accordingly, determining the status of the patient or consultant and interpreting sequencing results from many genes can largely increase the complexity of genetic counseling. Moreover, the current environment of big data that can be readily shared via the internet and a ubiquitous network provides many different avenues for which a consultant must handle the traditional principle of genetic counseling in different ways. Thus, further consideration and rethinking of genetic counseling principles are necessary in the era of NGS. In this review, we discuss several aspects of genetic counseling that one can encounter when faced with NGS data.
Figure
Cited by 2 articles
-
A Case of Next-generation Sequencing Gene Testing: Points to be Considered in Testing and Reporting
Na-Kyoung Kim, Jong-Won Kim
Ann Lab Med. 2022;42(2):296-297. doi: 10.3343/alm.2022.42.2.296.Current Issues, Challenges, and Future Perspectives of Genetic Counseling in Korea
Namhee Kim, Sun-Young Kong, Jongha Yoo, Do-Hoon Kim, Soo Hyun Seo, Jieun Kim
Ann Lab Med. 2022;42(3):314-320. doi: 10.3343/alm.2022.42.3.314.
Reference
-
1. Harper P. Practical genetic counselling. 5th ed. Woburn, MA: Butterworth-Heinemann;1998. p. 3–4.2. Vigorito E, Kuchenbaecker KB, Beesley J, Adlard J, Agnarsson BA, Andrulis IL, et al. Fine-scale mapping at 9p22.2 identifies candidate causal variants that modify ovarian cancer risk in BRCA1 and BRCA2 mutation carriers. PLoS One. 2016; 11:e0158801. PMID: 27463617.3. Kalia SS, Adelman K, Bale SJ, Chung WK, Eng C, Evans JP, et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017; 19:249–255. PMID: 27854360.4. van El CG, Cornel MC, Borry P, Hastings RJ, Fellmann F, Hodgson SV, et al. Whole-genome sequencing in health care: recommendations of the European Society of Human Genetics. Eur J Hum Genet. 2013; 21:580–584. PMID: 23676617.5. Park KS, Cho EY, Nam SJ, Ki CS, Kim JW. Comparative analysis of BRCA1 and BRCA2 variants of uncertain significance in patients with breast cancer: a multifactorial probability-based model versus ACMG standards and guidelines for interpreting sequence variants. Genet Med. 2016; 18:1250–1257. PMID: 27124784.6. Ryu JM, Kang G, Nam SJ, Kim SW, Yu J, Lee SK, et al. Suggestion of BRCA1 c.5339T>C (p.L1780P) variant confer from ‘unknown significance’ to ‘Likely pathogenic’ based on clinical evidence in Korea. Breast. 2017; 33:109–116. PMID: 28364669.7. Schneider K. Counseling about cancer: strategies for genetic counseling. 3rd ed. New Jersey: Wiley-Blackwell;2012. p. 409–443.8. Resta R. Complicated shadows: a critique of autonomy in genetic counseling. In : Leroy B, Veach P, Bartels DM, editors. Genetic counseling practice: advanced concepts and skills. New Jersey: Wiley-Blackwell;2010. p. 22.9. Wilson J. To know or not to know? Genetic ignorance, autonomy and paternalism. Bioethics. 2005; 19:492–504. PMID: 16425486.10. Andorno R. The right not to know: an autonomy based approach. J Med Ethics. 2004; 30:435–439. discussion 439-40. PMID: 15467071.11. Ndinya-Achola J, Ambani J, Temmerman M, Piot P. The right not to know HIV-test results. Lancet. 1995; 345:969–970. PMID: 7619122.12. Malpas P. The right to remain in ignorance about genetic information--can such a right be defended in the name of autonomy? N Z Med J. 2005; 118:U1611. PMID: 16132072.13. Hofmann B. Incidental findings of uncertain significance: To know or not to know-that is not the question. BMC Med Ethics. 2016; 17:13. PMID: 26873084.14. Robins Wahlin TB. To know or not to know: a review of behaviour and suicidal ideation in preclinical Huntington's disease. Patient Educ Couns. 2007; 65:279–287. PMID: 17000074.15. Shahmirzadi L, Chao EC, Palmaer E, Parra MC, Tang S, Gonzalez KD. Patient decisions for disclosure of secondary findings among the first 200 individuals undergoing clinical diagnostic exome sequencing. Genet Med. 2014; 16:395–399. PMID: 24113345.16. Husted J. Autonomy and a right not to know. In : Chadwick R, Levitt M, Shickle D, editors. The right to know and the right not to know. 2nd ed. Cambridge: Cambridge University Press;2014. p. 24–37.17. Pergament D, Ilijic K. The legal past, present and future of prenatal genetic testing: professional liability and other legal challenges affecting patient access to services. J Clin Med. 2014; 3:1437–1465. PMID: 26237611.18. Sparrow R. Imposing genetic diversity. Am J Bioeth. 2015; 15:2–10. PMID: 26030484.19. Wertz DC, Fletcher JC, Berg K. Review of ethical issues in medical genetics. World Health Organization Human Genetics Programme. 2003. p. 62.20. Pichini A, Shuman C, Sappleton K, Kaufman M, Chitayat D, Babul-Hirji R. Experience with genetic counseling: the adolescent perspective. J Genet Couns. 2016; 25:583–595. PMID: 26573304.21. Hehir-Kwa JY, Claustres M, Hastings RJ, van Ravenswaaij-Arts C, Christenhusz G, Genuardi M, et al. Towards a European consensus for reporting incidental findings during clinical NGS testing. Eur J Hum Genet. 2015; 23:1601–1606. PMID: 26036857.22. Green RC, Berg JS, Grody WW, Kalia SS, Korf BR, Martin CL, et al. ACMG recommendations for reporting of incidental findings in clinical exome and genome sequencing. Genet Med. 2013; 15:565–574. PMID: 23788249.23. Hallowell N, Hall A, Alberg C, Zimmern R. Revealing the results of wholegenome sequencing and whole-exome sequencing in research and clinical investigations: some ethical issues. J Med Ethics. 2015; 41:317–321. PMID: 25038088.24. Laurino MY, Leppig KA, Abad PJ, Cham B, Chu YWY, Kejriwal S, et al. A report on ten Asia Pacific countries on current status and future directions of the genetic counseling profession: the establishment of the Professional Society of Genetic Counselors in Asia. J Genet Couns. 2017; 1–12.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Guidelines for Genetic Counseling and Reporting of Cancer Genetic Test Results: Genetic Test for Hereditary Cancer-predisposing Syndrome Using Next-generation Sequencing
- Challenge of Personalized Medicine in the Genomic Era
- Clinical applications of next-generation sequencing in the diagnosis of genetic disorders in Korea: a narrative review
- Recent Advances in the Clinical Application of Next-Generation Sequencing
- The Role of Urologist in the Era of Assisted Reproductive Technology (ART)