J Clin Neurol.
2018 Apr;14(2):206-211. 10.3988/jcn.2018.14.2.206.
Demographic and Clinical Correlates of Seizure Frequency: Findings from the Managing Epilepsy Well Network Database
- Affiliations
-
- 1Geisel School of Medicine at Dartmouth, Hanover, NH, USA. Barbara.C.Jobst@hitchcock.org
- 2Department of Neurology, Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA.
- 3Neurological and Behavioral Outcomes Center, University Hospitals Cleveland Medical Center, Cleveland, OH, USA.
- 4Case Western Reserve University, School of Medicine, Cleveland, OH, USA.
- 5Rollins School of Public Health, Emory University, Atlanta, GA, USA.
- 6Center for Managing Chronic Disease, University of Michigan, Ann Arbor, MI, USA.
- 7Department of Population Health, NYU School of Medicine, New York, NY, USA.
- 8Department of Neurology, NYU School of Medicine, New York, NY, USA.
- 9School of Public Health, The University of Texas Health Science Center, Houston, TX, USA.
- 10Center for Health Promotion and Prevention Research, School of Public Health, The University of Texas, Houston, TX, USA.
- 11Departments of Neurology, Neurological Surgery, and Rehabilitation Medicine, Harborview Medical Center, Seattle, WA, USA.
- 12Department of Health Services, Health Promotion Research Center, University of Washington School of Public Health, Seattle, WA, USA.
- KMID: 2407948
- DOI: http://doi.org/10.3988/jcn.2018.14.2.206
Abstract
- BACKGROUND AND PURPOSE
Epilepsy is a chronic neurological disease that represents a tremendous burden on both patients and society in general. Studies have addressed how demographic variables, socioeconomic variables, and psychological comorbidity are related to the quality of life (QOL) of people with epilepsy (PWE). However, there has been less focus on how these factors may differ between patients who exhibit varying degrees of seizure control. This study utilized data from the Managing Epilepsy Well (MEW) Network of the Centers for Disease Control and Prevention with the aim of elucidating differences in demographic variables, depression, and QOL between adult PWE.
METHODS
Demographic variables, depression, and QOL were compared between PWE who experience clinically relevant differences in seizure occurrence.
RESULTS
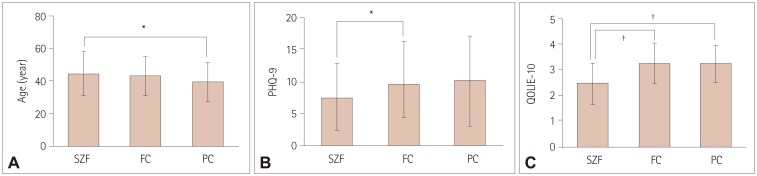
Gender, ethnicity, race, education, income, and relationship status did not differ significantly between the seizure-frequency categories (p>0.05). People with worse seizure control were significantly younger (p=0.039), more depressed (as assessed using the Patient Health Questionnaire) (p=0.036), and had lower QOL (as determined using the 10-item Quality of Life in Epilepsy for Adults scale) (p < 0.001).
CONCLUSIONS
The present results underscore the importance of early screening, detection, and treatment of depression, since these factors relate to both seizure occurrence and QOL in PWE.
MeSH Terms
Figure
Reference
-
1. Kobau R, Luo Y, Zack MM, Helmers S, Thurman DJ. Centers for Disease Control and Prevention (CDC). Epilepsy in adults and access to care–United States, 2010. MMWR Morb Mortal Wkly Rep. 2012; 61:909–913. PMID: 23151949.2. Yoon D, Frick KD, Carr DA, Austin JK. Economic impact of epilepsy in the United States. Epilepsia. 2009; 50:2186–2191. PMID: 19508694.
Article3. Dieleman JL, Baral R, Birger M, Bui AL, Bulchis A, Chapin A, et al. US spending on personal health care and public health, 1996-2013. JAMA. 2016; 316:2627–2646. PMID: 28027366.
Article4. Kleen JK, Scott RC, Lenck-Santini PP, Holmes GL. Cognitive and behavioral comorbidities of epilepsy. In : Noebels JL, Avoli M, Rogawski MA, Delgado-Escueta AV, editors. Jasper's Basic Mechanisms of the Epilepsies. 4th ed. Bethesda: National Center for Biotechnology Information (US);2012. p. 915–929.5. Lehrner J, Kalchmayr R, Serles W, Olbrich A, Pataraia E, Aull S, et al. Health-related quality of life (HRQOL), activity of daily living (ADL) and depressive mood disorder in temporal lobe epilepsy patients. Seizure. 1999; 8:88–92. PMID: 10222299.
Article6. Loring DW, Meador KJ, Lee GP. Determinants of quality of life in epilepsy. Epilepsy Behav. 2004; 5:976–980. PMID: 15582847.
Article7. Baker GA, Brooks J, Buck D, Jacoby A. The stigma of epilepsy: a European perspective. Epilepsia. 2000; 41:98–104. PMID: 10643931.
Article8. Johnson EK, Jones JE, Seidenberg M, Hermann BP. The relative impact of anxiety, depression, and clinical seizure features on health-related quality of life in epilepsy. Epilepsia. 2004; 45:544–550. PMID: 15101836.
Article9. Djibuti M, Shakarishvili R. Influence of clinical, demographic, and socioeconomic variables on quality of life in patients with epilepsy: findings from Georgian study. J Neurol Neurosurg Psychiatry. 2003; 74:570–573. PMID: 12700294.
Article10. Vickrey BG, Berg AT, Sperling MR, Shinnar S, Langfitt JT, Bazil CW, et al. Relationships between seizure severity and health-related quality of life in refractory localization-related epilepsy. Epilepsia. 2000; 41:760–764. PMID: 10840410.
Article11. Gilliam F, Hecimovic H, Sheline Y. Psychiatric comorbidity, health, and function in epilepsy. Epilepsy Behav. 2003; 4(Suppl 4):S26–S30. PMID: 14654425.
Article12. Azuma H, Akechi T. Effects of psychosocial functioning, depression, seizure frequency, and employment on quality of life in patients with epilepsy. Epilepsy Behav. 2014; 41:18–20. PMID: 25269689.
Article13. van Hout B, Gagnon D, Souêtre E, Ried S, Remy C, Baker G, et al. Relationship between seizure frequency and costs and quality of life of outpatients with partial epilepsy in France, Germany, and the United Kingdom. Epilepsia. 1997; 38:1221–1226. PMID: 9579924.
Article14. McLachlan RS, Rose KJ, Derry PA, Bonnar C, Blume WT, Girvin JP. Health-related quality of life and seizure control in temporal lobe epilepsy. Ann Neurol. 1997; 41:482–489. PMID: 9124805.
Article15. Lortie A, Chiron C, Mumford J, Dulac O. The potential for increasing seizure frequency, relapse, and appearance of new seizure types with vigabatrin. Neurology. 1993; 43(11 Suppl 5):S24–S27. PMID: 8232984.16. Wiebe S, Blume WT, Girvin JP, Eliasziw M. Effectiveness and Efficiency of Surgery for Temporal Lobe Epilepsy Study Group. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001; 345:311–318. PMID: 11484687.
Article17. Sajatovic M, Jobst BC, Shegog R, Bamps YA, Begley CE, Fraser RT, et al. The managing epilepsy well network: advancing epilepsy self-management. Am J Prev Med. 2017; 52(3S3):S241–S245. PMID: 28215372.18. Sahoo SS, Zhang GQ, Bamps Y, Fraser R, Stoll S, Lhatoo SD, et al. Managing information well: toward an ontology-driven informatics platform for data sharing and secondary use in epilepsy self-management research centers. Health Informatics J. 2016; 22:548–561. PMID: 25769938.
Article19. Caller TA, Ferguson RJ, Roth RM, Secore KL, Alexandre FP, Zhao W, et al. A cognitive behavioral intervention (HOBSCOTCH) improves quality of life and attention in epilepsy. Epilepsy Behav. 2016; 57:111–117. PMID: 26943948.
Article20. DiIorio C, Bamps Y, Walker ER, Escoffery C. Results of a research study evaluating WebEase, an online epilepsy self-management program. Epilepsy Behav. 2011; 22:469–474. PMID: 21889413.
Article21. Cramer JA, Perrine K, Devinsky O, Meador K. A brief questionnaire to screen for quality of life in epilepsy: the QOLIE-10. Epilepsia. 1996; 37:577–582. PMID: 8641236.
Article22. Bautista RE, Glen ET, Wludyka PS, Shetty NK. Factors associated with utilization of healthcare resources among epilepsy patients. Epilepsy Res. 2008; 79:120–129. PMID: 18339521.
Article23. Bautista RE, Glen ET, Shetty NK. Factors associated with satisfaction with care among patients with epilepsy. Epilepsy Behav. 2007; 11:518–524. PMID: 17936688.
Article24. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16:606–613. PMID: 11556941.25. Rathore JS, Jehi LE, Fan Y, Patel SI, Foldvary-Schaefer N, Ramirez MJ, et al. Validation of the Patient Health Questionnaire-9 (PHQ-9) for depression screening in adults with epilepsy. Epilepsy Behav. 2014; 37:215–220. PMID: 25064739.
Article26. Seminario NA, Farias ST, Jorgensen J, Bourgeois JA, Seyal M. Determination of prevalence of depression in an epilepsy clinic using a brief DSM-IV-based self-report questionnaire. Epilepsy Behav. 2009; 15:362–366. PMID: 19525150.
Article27. Fiest KM, Patten SB, Altura KC, Bulloch AG, Maxwell CJ, Wiebe S, et al. Patterns and frequency of the treatment of depression in persons with epilepsy. Epilepsy Behav. 2014; 39:59–64. PMID: 25203325.
Article28. Shcherbakova N, Rascati K, Brown C, Lawson K, Novak S, Richards KM, et al. Factors associated with seizure recurrence in epilepsy patients treated with antiepileptic monotherapy: a retrospective observational cohort study using US administrative insurance claims. CNS Drugs. 2014; 28:1047–1058. PMID: 25086640.
Article29. Escoffery C, McGee RE, Bamps Y, Helmers SL. Differences in epilepsy self-management behaviors among young and older adults. Austin J Neurol Disord Epilepsy. 2016; 3:1015.30. Jokeit H, Ebner A. Long term effects of refractory temporal lobe epilepsy on cognitive abilities: a cross sectional study. J Neurol Neurosurg Psychiatry. 1999; 67:44–50. PMID: 10369821.
Article31. Eatock J, Baker GA. Managing patient adherence and quality of life in epilepsy. Neuropsychiatr Dis Treat. 2007; 3:117–131. PMID: 19300542.
Article32. Kerr MP, Mensah S, Besag F, de Toffol B, Ettinger A, Kanemoto K, et al. International consensus clinical practice statements for the treatment of neuropsychiatric conditions associated with epilepsy. Epilepsia. 2011; 52:2133–2138. PMID: 21955156.
Article33. LaFrance WC Jr, Kanner AM, Hermann B. Psychiatric comorbidities in epilepsy. Int Rev Neurobiol. 2008; 83:347–383. PMID: 18929092.34. Li J, Wang X, Meng H, Zeng K, Quan F, Liu F. Systemic family therapy of comorbidity of anxiety and depression with epilepsy in adolescents. Psychiatry EInvestig. 2016; 13:305–310.
Article35. DiIorio CK, Bamps YA, Edwards AL, Escoffery C, Thompson NJ, Begley CE, et al. The prevention research centers’ managing epilepsy well network. Epilepsy Behav. 2010; 19:218–224. PMID: 20869323.
Article36. Thompson NJ, Patel AH, Selwa LM, Stoll SC, Begley CE, Johnson EK, et al. Expanding the efficacy of Project UPLIFT: distance delivery of mindfulness-based depression prevention to people with epilepsy. J Consult Clin Psychol. 2015; 83:304–313. PMID: 25495361.
Article37. Thompson NJ, Walker ER, Obolensky N, Winning A, Barmon C, Diiorio C, et al. Distance delivery of mindfulness-based cognitive therapy for depression: project UPLIFT. Epilepsy Behav. 2010; 19:247–254. PMID: 20851055.
Article38. Ciechanowski P, Chaytor N, Miller J, Fraser R, Russo J, Unutzer J, et al. PEARLS depression treatment for individuals with epilepsy: a randomized controlled trial. Epilepsy Behav. 2010; 19:225–231. PMID: 20609631.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Influencing on Fatigue in Patients with Epilepsy
- Efficacy of levetiracetam in refractory childhood epilepsy
- Driving in Patients with Epilepsy: Doctor's Perspective
- The Latest Classification of Epilepsy and Clinical Significance of Electroencephalography
- Changes in frequency of seizure after acute antiepileptic drugs withdrawal