J Korean Soc Radiol.
2018 Apr;78(4):265-278. 10.3348/jksr.2018.78.4.265.
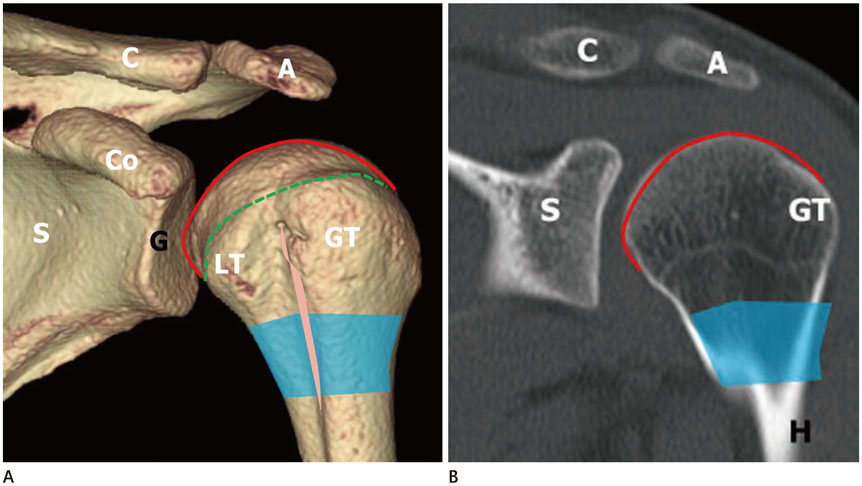
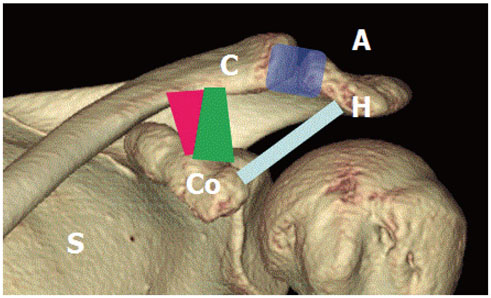
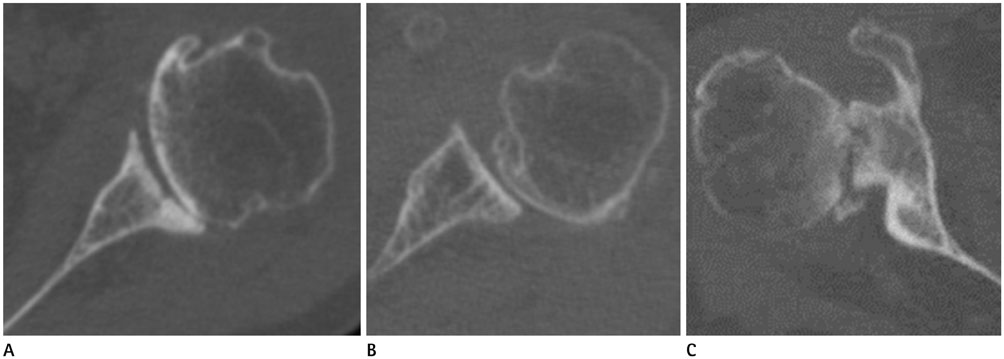
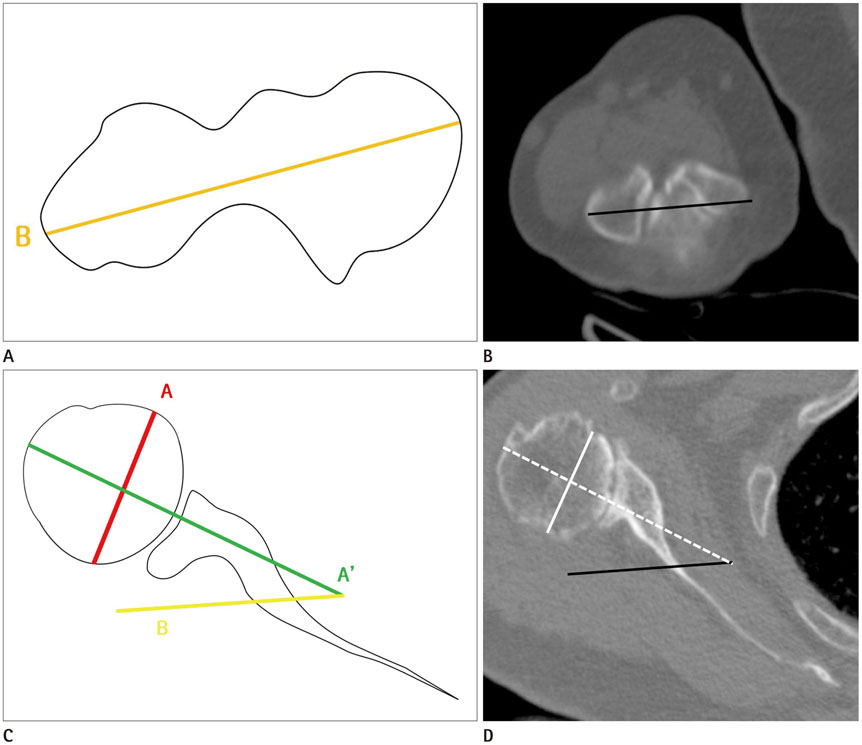
A Comprehensive Review of Shoulder CT Morphometry: What Surgeons Wants to Know
- Affiliations
-
- 1Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea. joongmoahn@gmail.com
- 2Department of Orthopaedic Surgery, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2407932
- DOI: http://doi.org/10.3348/jksr.2018.78.4.265
Abstract
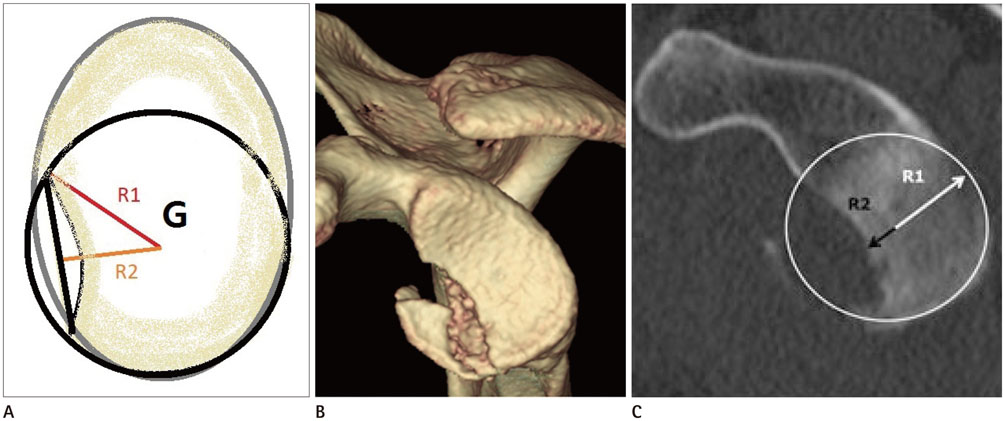
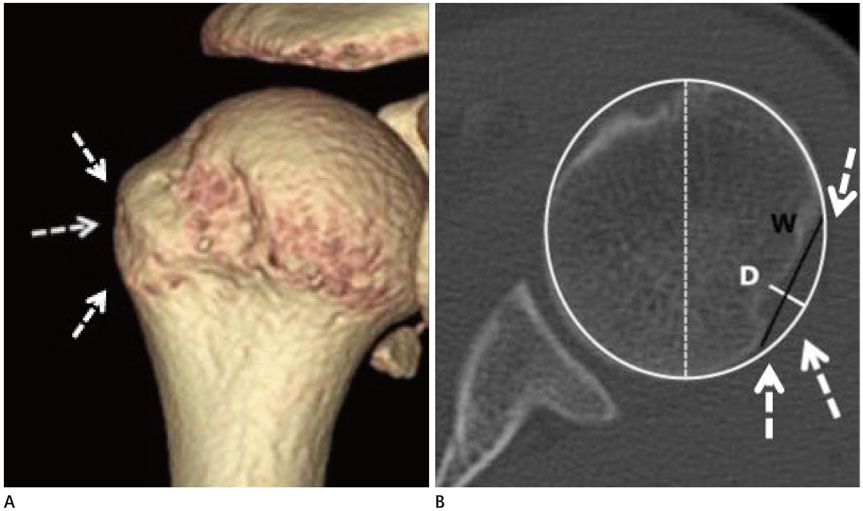
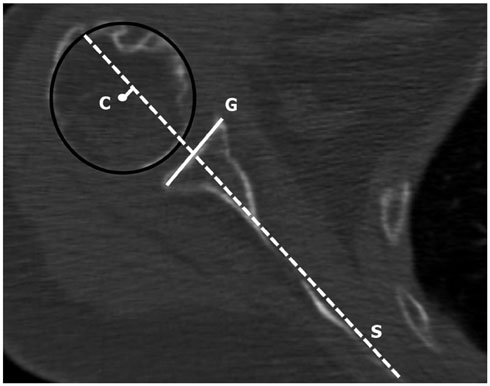
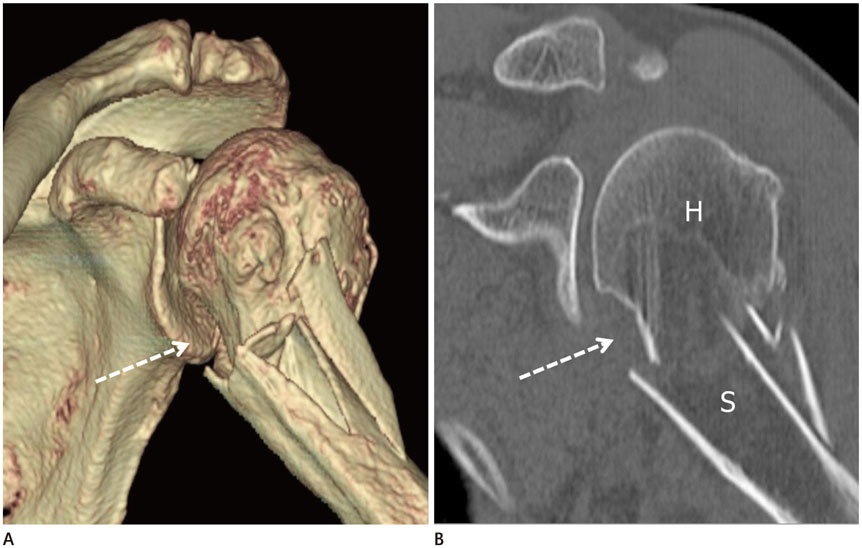
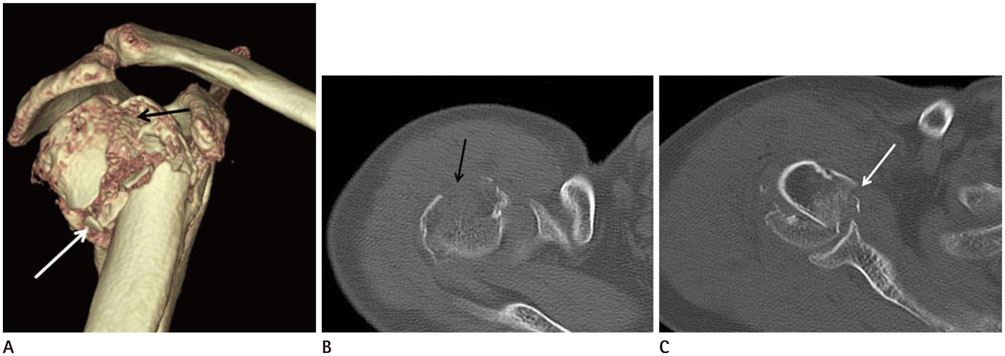
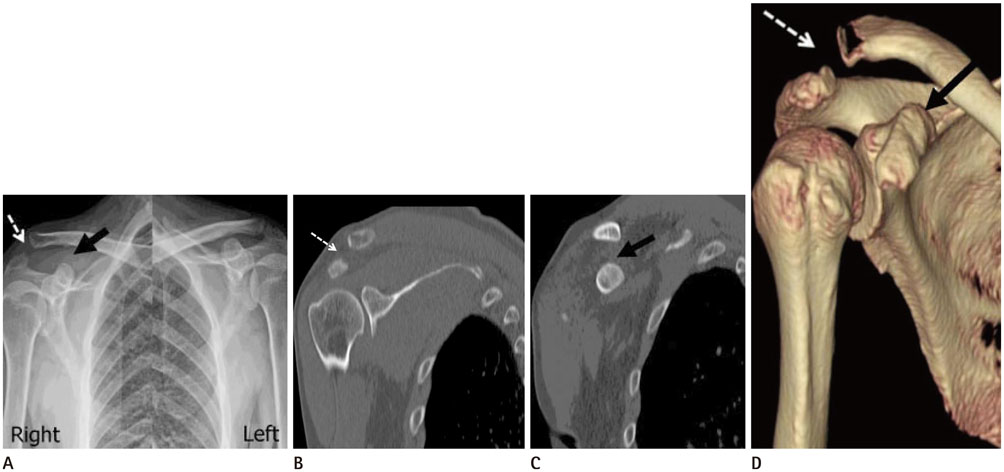
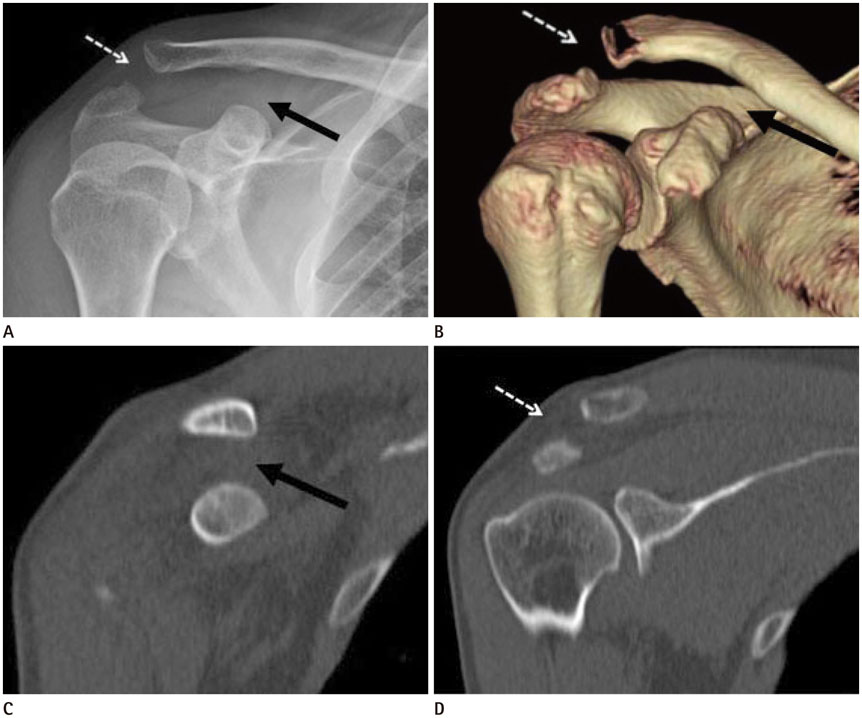
- A variety of surgical techniques have been employed for shoulder problems, i.e., arthroplasty, arthroscopy, and fracture fixation, etc. A thorough understanding and knowledge of the normal anatomy, physiology, biomechanics, and pathomechanics of the glenohumeral joint can help facilitate a successful pre-operative evaluation of the shoulder. The authors reviewed practical measurement methods of a shoulder computed tomography (CT) with three-dimensional volume-rendered images, from the orthopedic surgeon's viewpoint, to aid radiologists make structured reports. It is important that the radiologist be familiar with the normal and abnormal imaging appearances of the shoulder CT before and after the surgical procedures.
MeSH Terms
Figure
Reference
-
1. Pearl ML. Proximal humeral anatomy in shoulder arthroplasty: implications for prosthetic design and surgical technique. J Shoulder Elbow Surg. 2005; 14:1 Suppl S. 99S–104S.
Article2. Whiston TB. Fractures of the surgical neck of the humerus. J Bone Joint Surg Br. 1954; 36-B:423–427.
Article3. Sandstrom CK, Kennedy SA, Gross JA. Acute shoulder trauma: what the surgeon wants to know. Radiographics. 2015; 35:475–492.
Article4. Fukuda K, Craig EV, An KN, Cofield RH, Chao EY. Biomechanical study of the ligamentous system of the acromioclavicular joint. J Bone Joint Surg Am. 1986; 68:434–440.
Article5. Hoenecke HR Jr, Hermida JC, Flores-Hernandez C, D'Lima DD. Accuracy of CT-based measurements of glenoid version for total shoulder arthroplasty. J Shoulder Elbow Surg. 2010; 19:166–171.
Article6. Shapiro TA, McGarry MH, Gupta R, Lee YS, Lee TQ. Biomechanical effects of glenoid retroversion in total shoulder arthroplasty. J Shoulder Elbow Surg. 2007; 16:3 Suppl. S90–S95.
Article7. Friedman RJ, Hawthorne KB, Genez BM. The use of computerized tomography in the measurement of glenoid version. J Bone Joint Surg Am. 1992; 74:1032–1037.
Article8. Iannotti JP, Norris TR. Influence of preoperative factors on outcome of shoulder arthroplasty for glenohumeral osteoarthritis. J Bone Joint Surg Am. 2003; 85-A:251–258.
Article9. Inui H, Sugamoto K, Miyamoto T, Machida A, Hashimoto J, Nobuhara K. Evaluation of three-dimensional glenoid structure using MRI. J Anat. 2001; 199(Pt 3):323–328.
Article10. Matsumura N, Ogawa K, Ikegami H, Collin P, Walch G, Toyama Y. Computed tomography measurement of glenoid vault version as an alternative measuring method for glenoid version. J Orthop Surg Res. 2014; 9:17.
Article11. Farron A, Terrier A, Büchler P. Risks of loosening of a prosthetic glenoid implanted in retroversion. J Shoulder Elbow Surg. 2006; 15:521–526.
Article12. Walch G, Badet R, Boulahia A, Khoury A. Morphologic study of the glenoid in primary glenohumeral osteoarthritis. J Arthroplasty. 1999; 14:756–760.
Article13. Boileau P, Bicknell RT, Mazzoleni N, Walch G, Urien JP. CT scan method accurately assesses humeral head retroversion. Clin Orthop Relat Res. 2008; 466:661–669.
Article14. Kronberg M, Broström LA. Humeral head retroversion in patients with unstable humeroscapular joints. Clin Orthop Relat Res. 1990; (260):207–211.
Article15. Boileau P, Walch G, Liotard JP. [Radio-cinematographic study of active elevation of the prosthetic shoulder]. Rev Chir Orthop Reparatrice Appar Mot. 1992; 78:355–364.16. Robertson DD, Yuan J, Bigliani LU, Flatow EL, Yamaguchi K. Three-dimensional analysis of the proximal part of the humerus: relevance to arthroplasty. J Bone Joint Surg Am. 2000; 82-A:1594–1602.
Article17. Hempfing A, Leunig M, Ballmer FT, Hertel R. Surgical landmarks to determine humeral head retrotorsion for hemiarthroplasty in fractures. J Shoulder Elbow Surg. 2001; 10:460–463.
Article18. Kummer FJ, Perkins R, Zuckerman JD. The use of the bicipital groove for alignment of the humeral stem in shoulder arthroplasty. J Shoulder Elbow Surg. 1998; 7:144–146.
Article19. Hertel R, Knothe U, Ballmer FT. Geometry of the proximal humerus and implications for prosthetic design. J Shoulder Elbow Surg. 2002; 11:331–338.
Article20. McPherson EJ, Friedman RJ, An YH, Chokesi R, Dooley RL. Anthropometric study of normal glenohumeral relationships. J Shoulder Elbow Surg. 1997; 6:105–112.
Article21. Krahl VE. The phylogeny and ontogeny of humeral torsion. Am J Phys Anthropol. 1976; 45(3 pt. 2):595–599.
Article22. Saka M, Yamauchi H, Yoshioka T, Hamada H, Gamada K. Conventional humeral retroversion measurements using computed tomography slices or ultrasound images are not correlated with the 3-dimensional humeral retroversion angle. Orthop J Sports Med. 2015; 3:2325967115573701.
Article23. Saka M, Yamauchi H, Hoshi K, Yoshioka T, Hamada H, Gamada K. Reliability and validity in measurement of true humeral retroversion by a three-dimensional cylinder fitting method. J Shoulder Elbow Surg. 2015; 24:809–813.
Article24. Boileau P, Villalba M, Héry JY, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006; 88:1755–1763.
Article25. Taylor DC, Arciero RA. Pathologic changes associated with shoulder dislocations. Arthroscopic and physical examination findings in first-time, traumatic anterior dislocations. Am J Sports Med. 1997; 25:306–331.26. Stevens KJ, Preston BJ, Wallace WA, Kerslake RW. CT imaging and three-dimensional reconstructions of shoulders with anterior glenohumeral instability. Clin Anat. 1999; 12:326–336.
Article27. Itoi E, Lee SB, Amrami KK, Wenger DE, An KN. Quantitative assessment of classic anteroinferior bony Bankart lesions by radiography and computed tomography. Am J Sports Med. 2003; 31:112–118.
Article28. Itoi E, Lee SB, Berglund LJ, Berge LL, An KN. The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Joint Surg Am. 2000; 82:35–46.
Article29. Saliken DJ, Bornes TD, Bouliane MJ, Sheps DM, Beaupre LA. Imaging methods for quantifying glenoid and Hill-Sachs bone loss in traumatic instability of the shoulder: a scoping review. BMC Musculoskelet Disord. 2015; 16:164.
Article30. Burkhart SS, Debeer JF, Tehrany AM, Parten PM. Quantifying glenoid bone loss arthroscopically in shoulder instability. Arthroscopy. 2002; 18:488–491.
Article31. Chuang TY, Adams CR, Burkhart SS. Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy. 2008; 24:376–382.
Article32. Sugaya H. Techniques to evaluate glenoid bone loss. Curr Rev Musculoskelet Med. 2014; 7:1–5.
Article33. Bois AJ, Fening SD, Polster J, Jones MH, Miniaci A. Quantifying glenoid bone loss in anterior shoulder instability: reliability and accuracy of 2-dimensional and 3-dimensional computed tomography measurement techniques. Am J Sports Med. 2012; 40:2569–2577.34. Nofsinger C, Browning B, Burkhart SS, Pedowitz RA. Objective preoperative measurement of anterior glenoid bone loss: a pilot study of a computer-based method using unilateral 3-dimensional computed tomography. Arthroscopy. 2011; 27:322–329.
Article35. Assunção JH, Gracitelli ME, Borgo GD, Malavolta EA, Bordalo-Rodrigues M, Ferreira Neto AA. Tomographic evaluation of Hill-Sachs lesions: is there a correlation between different methods of measurement. Acta Radiol. 2017; 58:77–83.
Article36. Richards RD, Sartoris DJ, Pathria MN, Resnick D. Hill-Sachs lesion and normal humeral groove: MR imaging features allowing their differentiation. Radiology. 1994; 190:665–668.
Article37. Kodali P, Jones MH, Polster J, Miniaci A, Fening SD. Accuracy of measurement of Hill-Sachs lesions with computed tomography. J Shoulder Elbow Surg. 2011; 20:1328–1334.
Article38. Cho SH, Cho NS, Rhee YG. Preoperative analysis of the Hill-Sachs lesion in anterior shoulder instability: how to predict engagement of the lesion. Am J Sports Med. 2011; 39:2389–2395.39. Kaar SG, Fening SD, Jones MH, Colbrunn RW, Miniaci A. Effect of humeral head defect size on glenohumeral stability: a cadaveric study of simulated Hill-Sachs defects. Am J Sports Med. 2010; 38:594–599.40. Provencher MT, Frank RM, Leclere LE, Metzger PD, Ryu JJ, Bernhardson A, et al. The Hill-Sachs lesion: diagnosis, classification, and management. J Am Acad Orthop Surg. 2012; 20:242–252.
Article41. Yun G, Kang Y, Ahn JM, Lee E, Lee JW, Oh JH, et al. Posterior decentering of the humeral head on shoulder MR arthrography: significant association with posterior synovial proliferation. AJR Am J Roentgenol. 2017; 208:1297–1303.
Article42. Shah N, Tung GA. Imaging signs of posterior glenohumeral instability. AJR Am J Roentgenol. 2009; 192:730–735.
Article43. Tung GA, Hou DD. MR arthrography of the posterior labrocapsular complex: relationship with glenohumeral joint alignment and clinical posterior instability. AJR Am J Roentgenol. 2003; 180:369–375.
Article44. Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury. 2006; 37:691–697.
Article45. Neer CS 2nd. Displaced proximal humeral fractures. II. Treatment of three-part and four-part displacement. J Bone Joint Surg Am. 1970; 52:1090–1103.46. Murray IR, Amin AK, White TO, Robinson CM. Proximal humeral fractures. J Bone Joint Surg Br. 2011; 93-B:1–11.
Article47. Sidor ML, Zuckerman JD, Lyon T, Koval K, Cuomo F, Schoenberg N. The Neer classification system for proximal humeral fractures. An assessment of interobserver reliability and intraobserver reproducibility. J Bone Joint Surg Am. 1993; 75:1745–1150.
Article48. Siebenrock KA, Gerber C. The reproducibility of classification of fractures of the proximal end of the humerus. J Bone Joint Surg Am. 1993; 75:1751–1755.
Article49. Berkes MB, Dines JS, Little MT, Garner MR, Shifflett GD, Lazaro LE, et al. The impact of three-dimensional CT imaging on intraobserver and interobserver reliability of proximal humeral fracture classifications and treatment recommendations. J Bone Joint Surg Am. 2014; 96:1281–1286.
Article50. Cho CH, Oh JH, Jung GH, Moon GH, Rhyou IH, Yoon JP, et al. The interrater and intrarater agreement of a modified neer classification system and associated treatment choice for lateral clavicle fractures. Am J Sports Med. 2015; 43:2431–2436.
Article51. Hertel R, Hempfing A, Stiehler M, Leunig M. Predictors of humeral head ischemia after intracapsular fracture of the proximal humerus. J Shoulder Elbow Surg. 2004; 13:427–433.
Article52. Min W, Davidovitch RI, Tejwani NC. Three-and four-part proximal humerus fractures: evolution to operative care. Bull NYU Hosp Jt Dis. 2012; 70:25–34.53. Mazzocca AD, Arciero RA, Bicos J. Evaluation and treatment of acromioclavicular joint injuries. Am J Sports Med. 2007; 35:316–329.
Article54. Williams GR, Nguyen VD, Rockwood CA. Classification and radiographic analysis of acromioclavicular dislocations. Appl Radiol. 1989; 18:29–34.55. Senna LF, Pires E. Modified axillary radiograph of the shoulder: a new position. Rev Bras Ortop. 2016; 52:115–118.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dynamic ultrasonography of the shoulder
- Current Concepts and Recent Trends in Arthroscopic Treatment of Large to Massive Rotator Cuff Tears: A Review
- Rate of incidental findings on routine preoperative computed tomography for shoulder arthroplasty
- Ultrasound Guidance for Intra-Articular Shoulder Injections for Frozen Shoulder
- Extravasation of Joint Fluid into the Mediastinum and the Deep Neck during Arthroscopic Shoulder Surgery