Trends, Characteristics, and Clinical Outcomes of Patients Undergoing Percutaneous Coronary Intervention in Korea between 2011 and 2015
- Affiliations
-
- 1Department of Applied Statistics, Gachon University, Seongnam, Korea.
- 2Department of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. min8684@hanmail.net
- 3Department of Cardiology, Daejeon St. Mary's Hospital, The Catholic University of Korea, Daejeon, Korea.
- 4Department of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- KMID: 2407900
- DOI: http://doi.org/10.4070/kcj.2017.0359
Abstract
- BACKGROUND AND OBJECTIVES
We sought to evaluate nationwide trends, characteristics, and clinical outcomes in patients undergoing percutaneous coronary intervention (PCI) in Korea.
METHODS
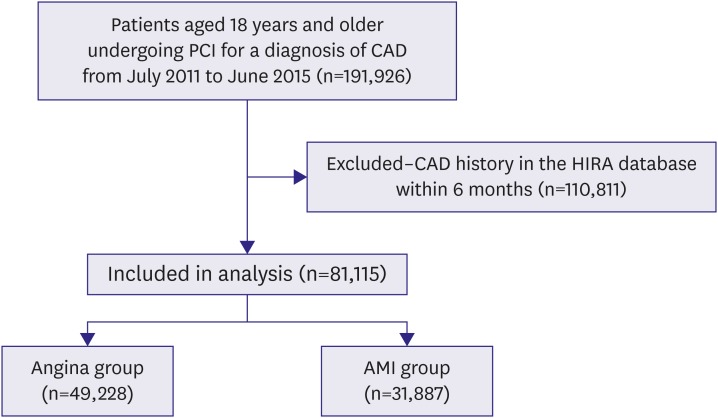
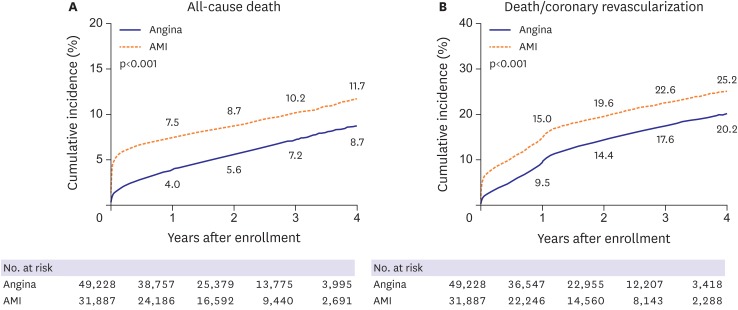
From National Health Insurance claims data in Korea, 81,115 patients, who underwent PCI for the first episode of coronary artery disease between 2011 and 2015, were enrolled. Patients were categorized into angina (n=49,288) or acute myocardial infarction (AMI, n=31,887) groups and analyzed.
RESULTS
The mean age of patients was 64.4±12.2 years and 56,576 (69.7%) were men. Diabetes, hyperlipidemia, and hypertension were observed in 27,086 (33.4%), 30,675 (37.8%), and 45,389 (56.0%) patients, respectively. There was a 10% increase in the number of patients undergoing PCI for angina between 2011-2012 and 2014-2015 (11,105 vs. 13,261; p=0.021). However, the number of patients undergoing PCI for AMI marginally decreased between 2011-2012 and 2014-2015 (8,068 vs. 7,823; p=0.052). In procedures, drug-eluting stent was the most frequently used device (93.2%), followed by balloon angioplasty (5.5%) and bare metal stents (1.3%). The mean number of stents per patient was 1.39±0.64. At discharge, dual-anti platelet therapy, statin, beta-blockers, and angiotensin converting enzyme inhibitor or angiotensin receptor blocker were provided to 76,292 (94.1%), 71,411 (88.0%), 57,429 (70.8%), and 54,418 (67.1%) patients, respectively. The mean in-hospital and 1-year total medical costs were 8,628,768±4,832,075 and 13,128,158±9,758,753 Korean Won, respectively. In-hospital mortality occurred in 2,094 patients (2.6%).
CONCLUSIONS
Appropriate healthcare strategies reflecting trends, characteristics, and clinical outcomes of PCI are needed in Korea.
Keyword
MeSH Terms
-
Angina Pectoris
Angioplasty, Balloon
Angiotensins
Blood Platelets
Coronary Artery Disease
Delivery of Health Care
Drug-Eluting Stents
Hospital Mortality
Humans
Hydroxymethylglutaryl-CoA Reductase Inhibitors
Hyperlipidemias
Hypertension
Korea*
Male
Myocardial Infarction
National Health Programs
Peptidyl-Dipeptidase A
Percutaneous Coronary Intervention*
Stents
Angiotensins
Peptidyl-Dipeptidase A
Figure
Cited by 3 articles
-
Current Practices of Percutaneous Coronary Intervention in Korea between 2011 and 2015
Han Saem Jeong, Soon Jun Hong
Korean Circ J. 2018;48(4):322-324. doi: 10.4070/kcj.2018.0058.The Current Status of Percutaneous Coronary Intervention in Korea: Based on Year 2014 & 2016 Cohort of Korean Percutaneous Coronary Intervention (K-PCI) Registry
Dong-Ho Shin, Hyun-Jae Kang, Jae-Sik Jang, Keon-Woong Moon, Young Bin Song, Duk-Woo Park, Jang-Whan Bae, Juhan Kim, Seung-Ho Hur, Byung Ok Kim, Dong Woon Jeon, Donghoon Choi, Kyoo-Rok Han
Korean Circ J. 2019;49(12):1136-1151. doi: 10.4070/kcj.2018.0413.Does Hospital Volume of Coronary Artery Bypass Graft Matter on Mid-Term Mortality?: from the Data of National Health Insurance Service in Korea
Jang-Whan Bae
Korean Circ J. 2021;51(6):530-532. doi: 10.4070/kcj.2021.0122.
Reference
-
1. Epstein AJ, Polsky D, Yang F, Yang L, Groeneveld PW. Coronary revascularization trends in the United States, 2001–2008. JAMA. 2011; 305:1769–1776. PMID: 21540420.2. Authors/Task Force members. 2014 ESC/EACTS Guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014; 35:2541–2619. PMID: 25173339.3. Jang JS, Han KR, Moon KW, et al. The current status of percutaneous coronary intervention in Korea: based on year 2014 cohort of Korean Percutaneous Coronary Intervention (K-PCI) Registry. Korean Circ J. 2017; 47:328–340. PMID: 28567083.4. Gwon HC, Jeon DW, Kang HJ, et al. The practice pattern of percutaneous coronary intervention in Korea: based on year 2014 cohort of Korean Percutaneous Coronary Intervention (K-PCI) Registry. Korean Circ J. 2017; 47:320–327. PMID: 28567082.5. Park GM, Han S, Kim SH, et al. Model for assessing cardiovascular risk in a Korean population. Circ Cardiovasc Qual Outcomes. 2014; 7:944–951. PMID: 25351481.6. Lee PH, Park GM, Kim YH, et al. Effect of beta blockers and renin-angiotensin system inhibitors on survival in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Medicine (Baltimore). 2016; 95:e2971. PMID: 26962802.7. Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43:1130–1139. PMID: 16224307.8. Shreibati JB, Baker LC, Hlatky MA. Association of coronary CT angiography or stress testing with subsequent utilization and spending among Medicare beneficiaries. JAMA. 2011; 306:2128–2136. PMID: 22089720.9. Park GM, Kim YH, Yun SC, et al. Anatomic or functional evaluation as an initial test for stable coronary artery disease: a propensity score analysis. J Nucl Med. 2016; 57:1364–1369. PMID: 27127224.10. Park GM, Kim SH, Jo MW, et al. Clinical impact and cost-effectiveness of coronary computed tomography angiography or exercise electrocardiogram in individuals without known cardiovascular disease. Medicine (Baltimore). 2015; 94:e917. PMID: 26020405.11. Wilson PW, D’Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998; 97:1837–1847. PMID: 9603539.12. Conroy RM, Pyörälä K, Fitzgerald AP, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003; 24:987–1003. PMID: 12788299.13. McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009; 150:505–515. PMID: 19380852.14. Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012; 366:54–63. PMID: 22216842.15. Kook HY, Jeong MH, Oh S, et al. Current trend of acute myocardial infarction in Korea (from the Korea Acute Myocardial Infarction Registry from 2006 to 2013). Am J Cardiol. 2014; 114:1817–1822. PMID: 25438907.16. Ueshima H, Sekikawa A, Miura K, et al. Cardiovascular disease and risk factors in Asia: a selected review. Circulation. 2008; 118:2702–2709. PMID: 19106393.17. Lagerqvist B, James SK, Stenestrand U, et al. Long-term outcomes with drug-eluting stents versus bare-metal stents in Sweden. N Engl J Med. 2007; 356:1009–1019. PMID: 17296822.18. Camenzind E, Steg PG, Wijns W. Stent thrombosis late after implantation of first-generation drug-eluting stents: a cause for concern. Circulation. 2007; 115:1440–1455. PMID: 17344324.19. Levine GN, Bates ER, Bittl JA, et al. 2016 ACC/AHA guideline focused update on duration of dual antiplatelet therapy in patients with coronary artery disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. 2016; 68:1082–1115. PMID: 27036918.20. Palmerini T, Biondi-Zoccai G, Della Riva D, et al. Stent thrombosis with drug-eluting and bare-metal stents: evidence from a comprehensive network meta-analysis. Lancet. 2012; 379:1393–1402. PMID: 22445239.21. Harnek J, Nilsson J, Friberg O, et al. The 2011 outcome from the Swedish Health Care Registry on Heart Disease (SWEDEHEART). Scand Cardiovasc J. 2013; 47(Suppl 62):1–10. PMID: 23941732.22. Bangalore S, Amoroso N, Fusaro M, Kumar S, Feit F. Outcomes with various drug-eluting or bare metal stents in patients with ST-segment-elevation myocardial infarction: a mixed treatment comparison analysis of trial level data from 34 068 patient-years of follow-up from randomized trials. Circ Cardiovasc Interv. 2013; 6:378–390. PMID: 23922145.23. Boden WE, O'Rourke RA, Teo KK, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med. 2007; 356:1503–1516. PMID: 17387127.24. Iqbal J, Zhang YJ, Holmes DR, et al. Optimal medical therapy improves clinical outcomes in patients undergoing revascularization with percutaneous coronary intervention or coronary artery bypass grafting: insights from the Synergy Between Percutaneous Coronary Intervention with TAXUS and Cardiac Surgery (SYNTAX) trial at the 5-year follow-up. Circulation. 2015; 131:1269–1277. PMID: 25847979.25. Goyal A, Alexander JH, Hafley GE, et al. Outcomes associated with the use of secondary prevention medications after coronary artery bypass graft surgery. Ann Thorac Surg. 2007; 83:993–1001. PMID: 17307447.26. Lin GA, Dudley RA, Lucas FL, Malenka DJ, Vittinghoff E, Redberg RF. Frequency of stress testing to document ischemia prior to elective percutaneous coronary intervention. JAMA. 2008; 300:1765–1773. PMID: 18854538.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Practices of Percutaneous Coronary Intervention in Korea between 2011 and 2015
- Literature Review of Nursing Intervention Studies for Patients Undergoing Percutaneous Coronary Intervention
- Gender Differences in Patients with Acute Myocardial Infarction Undergoing Percutaneous Coronary Intervention
- Recent Advances in Percutaneous Coronary Intervention in Coronary Artery Disease
- Perioperative management for patients undergoing noncardiac surgery after percutaneous coronary intervention