Yonsei Med J.
2018 May;59(3):376-382. 10.3349/ymj.2018.59.3.376.
Effect of Central Line Bundle Compliance on Central Line-Associated Bloodstream Infections
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. imfell@yuhs.ac
- 2Department of Infection Control, Gangnam Severance Hospital, Seoul, Korea.
- KMID: 2407860
- DOI: http://doi.org/10.3349/ymj.2018.59.3.376
Abstract
- PURPOSE
The present study aimed to evaluate the effect of central line (CL) bundle compliance on central line-associated bloodstream infections (CLABSIs) in different departments of the same hospital, including the intensive care unit (ICU) and other departments.
MATERIALS AND METHODS
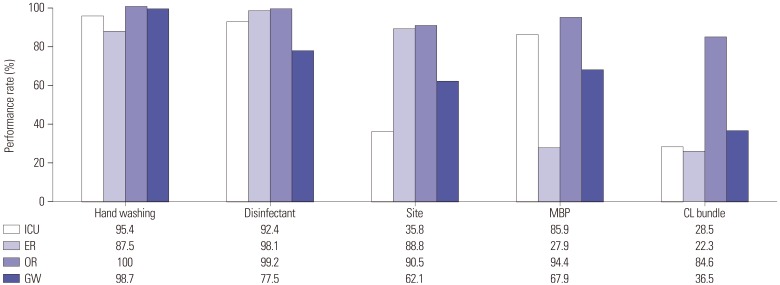
The four components of the CL bundle were hand hygiene, use of maximal sterile barrier precautions, chlorhexidine use, and selection of an appropriate site for venous access. Compliance of the CL bundle and CLABSIs were measured for every department [emergency room (ER), ICU, general ward (GW), and operating room (OR)]. A total of 1672 patients were included over 3 years (August 2013 through July 2016).
RESULTS
A total of 29 CLABSI episodes (1.73%) were identified, and only 53.7% of the patients completed CL bundles. The performance rates of all components of the CL bundle were 22.3%, 28.5%, 36.5%, and 84.6% for the ER, ICU, GW, and OR, respectively. The highest CLABSI rate was observed in patients of the ICU, for whom all components were not performed perfectly. Conversely, the lowest CLABSI rate was observed for patients of GWs, for whom all components were performed. Among individual components, femoral insertion site [relative risk (RR), 2.26; 95% confidence interval (CI), 1.09-4.68], not using a full body drape (RR, 3.55; 95% CI, 1.44-8.71), and not performing all CL bundle components (RR, 2.79; 95% CI, 1.19-6.54) were significant variables associated with CLABSIs.
CONCLUSION
This study provides direct evidence that completing all CL bundle components perfectly is essential for preventing CLABSIs. Customized education should be provided, according to specific weaknesses of bundle performance.
MeSH Terms
Figure
Cited by 1 articles
-
Korean National Healthcare-associated Infections Surveillance System, Intensive Care Unit Module Report: Summary of Data from July 2019 through June 2020
Eun Jin Kim, Yee Gyung Kwak, Sun Hee Kwak, Su Hui Ko, Oh Mee Kweon, Eu Suk Kim, Jin Hwa Kim, Tae Hyong Kim, Taek Soo Kim, Hee-Won Moon, Sun Hee Park, Jin Young Ahn, So-Yeon Yoo, Hyeon Mi Yoo, Sang-Oh Lee, Nan-Hyoung Cho, Pyoeng Gyun Choe, Ki Ho Hong, Yu-Mi Lee, Mi Suk Lee
Korean J Healthc Assoc Infect Control Prev. 2021;26(2):115-128. doi: 10.14192/kjicp.2021.26.2.115.
Reference
-
1. Stevens V, Geiger K, Concannon C, Nelson RE, Brown J, Dumyati G. Inpatient costs, mortality and 30-day re-admission in patients with central-line-associated bloodstream infections. Clin Microbiol Infect. 2014; 20:O318–O324. PMID: 24112305.
Article2. Ziegler MJ, Pellegrini DC, Safdar N. Attributable mortality of central line associated bloodstream infection: systematic review and meta-analysis. Infection. 2015; 43:29–36. PMID: 25331552.
Article3. Al-Rawajfah OM, Hewitt JB, Stetzer F, Cheema J. Length of stay and charges associated with health care-acquired bloodstream infections. Am J Infect Control. 2012; 40:227–232. PMID: 21621875.
Article4. Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011; 32:101–114. PMID: 21460463.
Article5. Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O'Grady NP, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014; 35(Suppl 2):S89–S107. PMID: 25376071.
Article6. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003; 348:1123–1133. PMID: 12646670.
Article7. Blot K, Bergs J, Vogelaers D, Blot S, Vandijck D. Prevention of central line-associated bloodstream infections through quality improvement interventions: a systematic review and meta-analysis. Clin Infect Dis. 2014; 59:96–105. PMID: 24723276.
Article8. Martínez-Morel HR, Sánchez-Payá J, Molina-Gómez MJ, García-Shimizu P, García Román V, Villanueva-Ruiz C, et al. Catheter-related bloodstream infection: burden of disease in a tertiary hospital. J Hosp Infect. 2014; 87:165–170. PMID: 24928788.
Article9. Choi JY, Kwak YG, Yoo H, Lee SO, Kim HB, Han SH, et al. Trends in the incidence rate of device-associated infections in intensive care units after the establishment of the Korean Nosocomial Infections Surveillance System. J Hosp Infect. 2015; 91:28–34. PMID: 26149593.
Article10. O'Grady NP, Alexander M, Burns LA, Dellinger EP, Garland J, Heard SO, et al. Healthcare Infection Control Practices Advisory Committee (HICPAC). Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011; 52:e162–e193. PMID: 21460264.11. Maki DG, Stolz SM, Wheeler S, Mermel LA. Prevention of central venous catheter-related bloodstream infection by use of an antiseptic-impregnated catheter. A randomized, controlled trial. Ann Intern Med. 1997; 127:257–266. PMID: 9265424.12. Wang H, Huang T, Jing J, Jin J, Wang P, Yang M, et al. Effectiveness of different central venous catheters for catheter-related infections: a network meta-analysis. J Hosp Infect. 2010; 76:1–11. PMID: 20638155.
Article13. Pronovost P, Needham D, Berenholtz S, Sinopoli D, Chu H, Cosgrove S, et al. An intervention to decrease catheter-related bloodstream infections in the ICU. N Engl J Med. 2006; 355:2725–2732. PMID: 17192537.
Article14. Jeong IS, Park SM, Lee JM, Song JY, Lee SJ. Effect of central line bundle on central line-associated bloodstream infections in intensive care units. Am J Infect Control. 2013; 41:710–716. PMID: 23394886.
Article15. Furuya EY, Dick A, Perencevich EN, Pogorzelska M, Goldmann D, Stone PW. Central line bundle implementation in US intensive care units and impact on bloodstream infections. PLoS One. 2011; 6:e15452. PMID: 21267440.
Article16. Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJ, Lloyd SM, et al. Elimination of central-venous-catheter-related bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011; 20:174–180.
Article17. Ong A, Dysert K, Herbert C, Laux L, Granato J, Crawford J, et al. Trends in central line-associated bloodstream infections in a trauma-surgical intensive care unit. Arch Surg. 2011; 146:302–307. PMID: 21422361.
Article18. McLaws ML, Burrell AR. Zero risk for central line-associated bloodstream infection: are we there yet? Crit Care Med. 2012; 40:388–393. PMID: 22020239.19. Furuya EY, Dick AW, Herzig CT, Pogorzelska-Maziarz M, Larson EL, Stone PW. Central line-associated bloodstream infection reduction and bundle compliance in intensive care units: a national study. Infect Control Hosp Epidemiol. 2016; 37:805–810. PMID: 27052993.
Article20. Conrick-Martin I, Foley M, Roche FM, Fraher MH, Burns KM, Morrison P, et al. Catheter-related infection in Irish intensive care units diagnosed with HELICS criteria: a multi-centre surveillance study. J Hosp Infect. 2013; 83:238–243. PMID: 23394814.
Article21. Apisarnthanarak A, Thongphubeth K, Yuekyen C, Warren DK, Fraser VJ. Effectiveness of a catheter-associated bloodstream infection bundle in a Thai tertiary care center: a 3-year study. Am J Infect Control. 2010; 38:449–455. PMID: 20006409.
Article22. Lee DH, Jung KY, Choi YH. Use of maximal sterile barrier precautions and/or antimicrobial-coated catheters to reduce the risk of central venous catheter-related bloodstream infection. Infect Control Hosp Epidemiol. 2008; 29:947–950. PMID: 18754735.
Article23. Kocazeybek B, Tokman HB. Prevalence of primary antimicrobial resistance of H. pylori in Turkey: a systematic review. Helicobacter. 2016; 21:251–260. PMID: 26395982.24. Comer A, Harris AD, Shardell M, Braun B, Belton BM, Wolfsthal SD, et al. Attaining Safety for Patients through Interdisciplinary Risk Reduction Efforts (ASPIRRE) Subgroup. Web-based training improves knowledge about central line bloodstream infections. Infect Control Hosp Epidemiol. 2011; 32:1219–1222. PMID: 22080663.
Article25. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008; 36:309–332. PMID: 18538699.
Article26. Choi JY, Kwak YG, Yoo H, Lee SO, Kim HB, Han SH, et al. Trends in the distribution and antimicrobial susceptibility of causative pathogens of device-associated infection in Korean intensive care units from 2006 to 2013: results from the Korean Nosocomial Infections Surveillance System (KONIS). J Hosp Infect. 2016; 92:363–371. PMID: 26876746.
Article27. Kwak YG, Lee SO, Kim HY, Kim YK, Park ES, Jin HY, et al. Risk factors for device-associated infection related to organisational characteristics of intensive care units: findings from the Korean Nosocomial Infections Surveillance System. J Hosp Infect. 2010; 75:195–199. PMID: 20434798.
Article28. Osorio J, álvarez D, Pacheco R, Gómez CA, Lozano A. [Implementation of an insertion bundle for preventing central line-associated bloodstream infections in an Intensive Care Unit in Colombia]. Rev Chilena Infectol. 2013; 30:465–473. PMID: 24248159.29. Leung PO, Lin HL, Lin YH, Lai CC. Different compliance with central line insertion bundle between intensivist and nonintensivist staff in intensive care units. Infect Control Hosp Epidemiol. 2014; 35:601–603.
Article30. Liang HW, Lin HL. Compliance with central line insertion bundles in an intensive care unit. Am J Infect Control. 2014; 42:581–582. PMID: 24773803.
Article31. Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. 3SITES Study Group. Intravascular complications of central venous catheterization by insertion site. N Engl J Med. 2015; 373:1220–1229. PMID: 26398070.
Article32. Arvaniti K, Lathyris D, Blot S, Apostolidou-Kiouti F, Koulenti D, Haidich AB. Cumulative evidence of randomized controlled and observational studies on catheter-related infection risk of central venous catheter insertion site in ICU patients: a pairwise and network meta-analysis. Crit Care Med. 2017; 45:e437–e448. PMID: 27632678.33. Ling ML, Apisarnthanarak A, Jaggi N, Harrington G, Morikane K, Thu le TA, et al. APSIC guide for prevention of Central Line Associated Bloodstream Infections (CLABSI). Antimicrob Resist Infect Control. 2016; 5:16. PMID: 27152193.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Incidences of Catheter Colonization and Central Line-Associated Bloodstream Infection According to Tegaderm vs. Chlorhexidine Gluconate (CHG)-Tegaderm Dressing
- Impact of Central Line Insertion Bundle on the Adherence of Bundle and Central Line-Associated Bloodstream Infections in the Operating Room
- Catheter care bundle and feedback to prevent central line-associated bloodstream infections in pediatric patients
- Comprehensive Approach to Prevention of Central Line-Associated Bloodstream Infection
- Central line-associated bloodstream infections in neonates