J Korean Ophthalmol Soc.
2018 Mar;59(3):295-300. 10.3341/jkos.2018.59.3.295.
A Case of Orbital Apex Syndrome with Central Retinal Artery and Vein Occlusion Following Trauma
- Affiliations
-
- 1Department of Ophthalmology, Jeju National University School of Medicine, Jeju, Korea. righthanded8282@gmail.com
- KMID: 2406966
- DOI: http://doi.org/10.3341/jkos.2018.59.3.295
Abstract
- PURPOSE
To report a case of orbital apex syndrome (OAS) combined with central retinal artery occlusion (CRAO) and central retinal vein occlusion (CRVO) following blunt trauma.
CASE SUMMARY
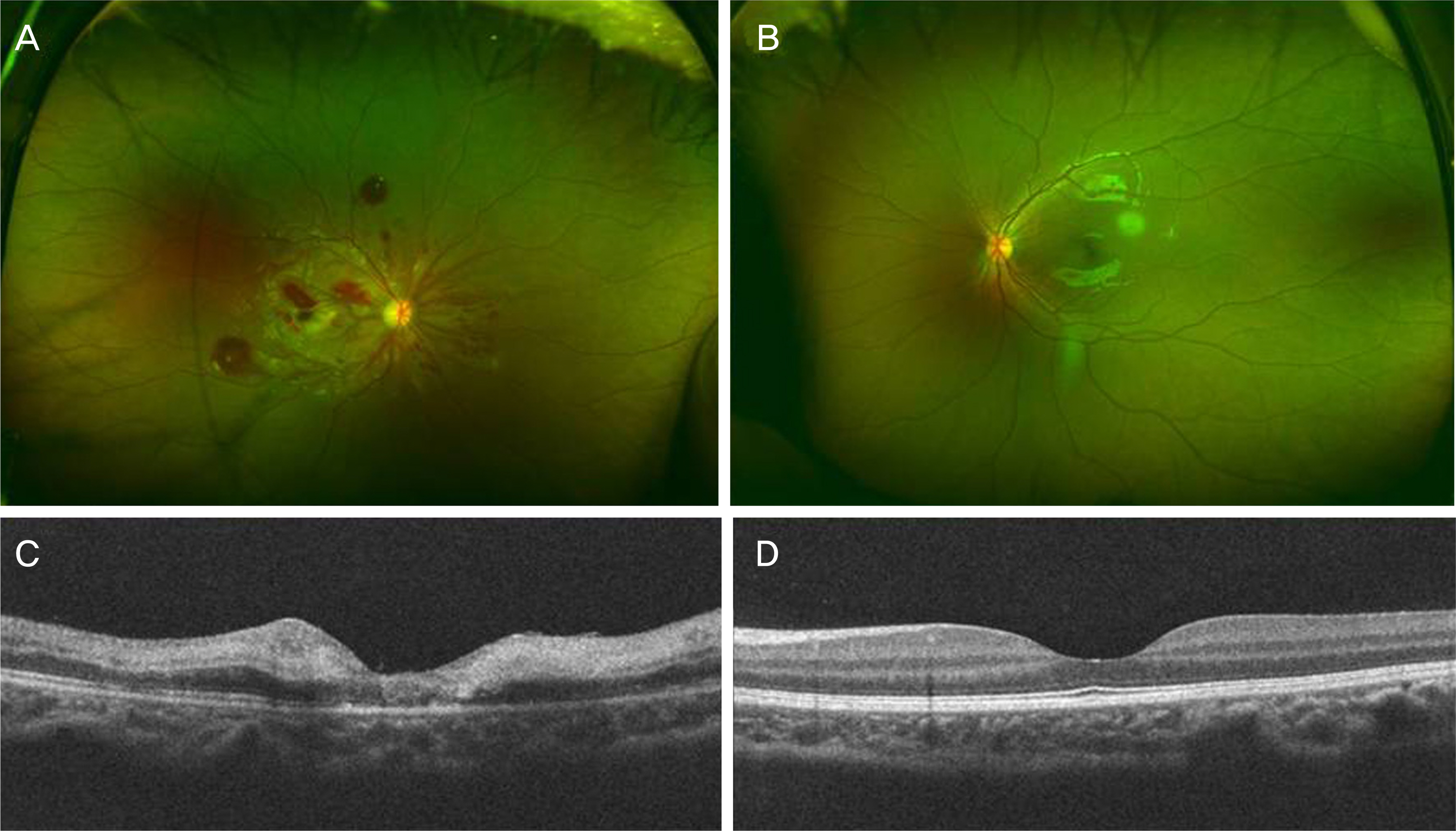
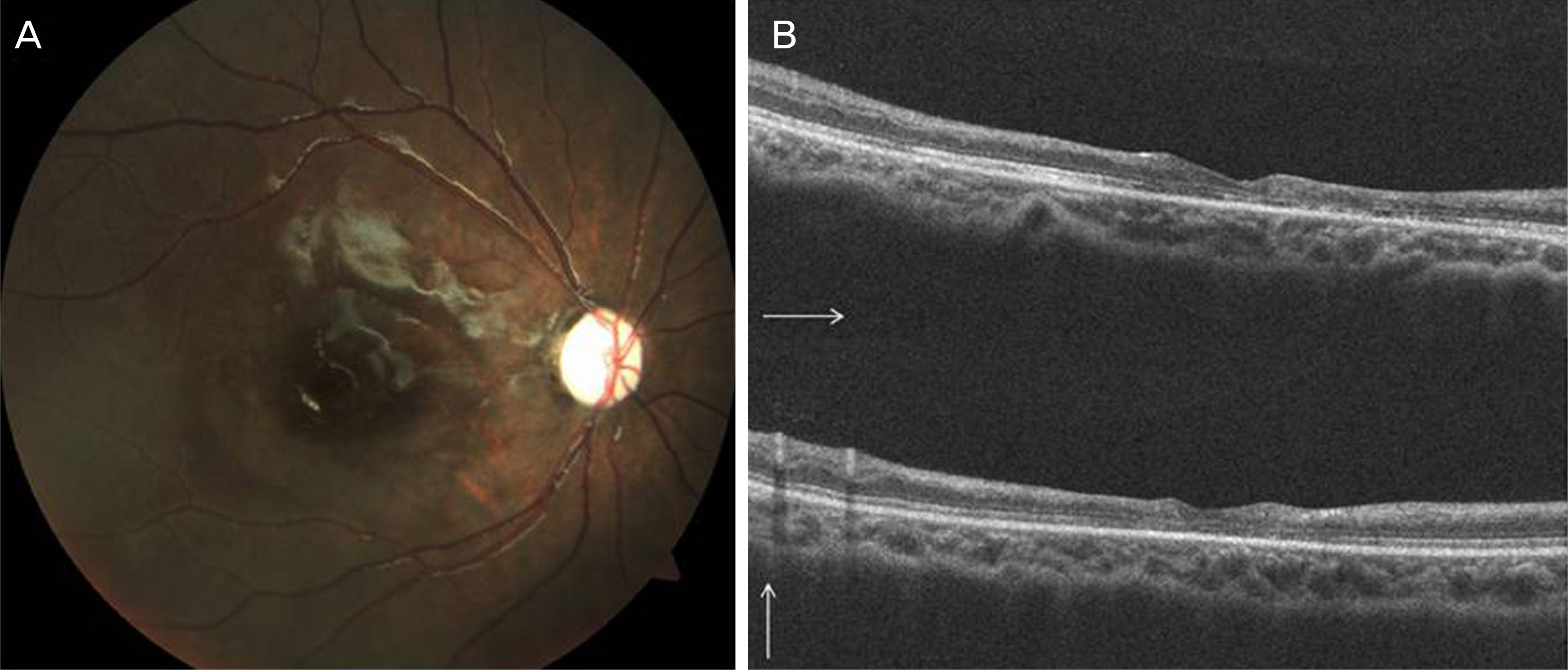
A 4-year-old female visited the hospital following a traffic accident. She was admitted because of multiple fractures of the skull and pneumocephalus. On day 5, she was referred to us with decreased visual acuity in her right eye. Her initial visual acuity was hand motions in the right eye and 0.8 in the left eye. The right eye showed a dilated pupil, ptosis, and total ophthalmoplegia, and the left eye showed limited abduction. A fundus examination revealed multiple retinal hemorrhages, tortuous veins, and an edematous white retina with a cherry-red spot in the right eye. Brain magnetic resonance imaging revealed an entrapped right optic nerve because of bony fragments in the orbital apex. The patient was diagnosed with OAS accompanied by CRAO and CRVO in the right eye, and with traumatic abducens nerve palsy in the left eye. After 6 months, the visual acuity was hand motions, and the fundus examination showed absorbed retinal hemorrhages, pale discs, and general retinal thinning of the right eye. Ptosis of the right eye and extraocular muscle movement of both eyes were improved.
CONCLUSIONS
Combined CRAO and CRVO following trauma is very rare and is even more rarely associated with OAS. It is important for clinicians to be aware of the potential for central retinal vessel occlusions and OAS in cases of blunt ocular trauma.
Keyword
MeSH Terms
-
Abducens Nerve Diseases
Accidents, Traffic
Brain
Child, Preschool
Female
Fractures, Multiple
Hand
Humans
Magnetic Resonance Imaging
Ophthalmoplegia
Optic Nerve
Orbit*
Pneumocephalus
Pupil
Retina
Retinal Artery Occlusion
Retinal Artery*
Retinal Hemorrhage
Retinal Vein
Retinal Vessels
Retinaldehyde
Skull
Veins*
Visual Acuity
Retinaldehyde
Figure
Reference
-
1). Park SJ, Choi NK, Seo KH, et al. Nationwide incidence of clinically diagnosed central retinal artery occlusion in Korea, 2008 to 2011. Ophthalmology. 2014; 121:1933–8.
Article2). Varma DD, Cugati S, Lee AW, Chen CS. A review of central retinal artery occlusion: clinical presentation and management. Eye (Lond). 2013; 27:688–97.
Article3). Lee WS, Yoon WT, Choi YJ, Park SP. Multiple cerebral infarctions with neurological symptoms and ophthalmic artery occlusion after filler injection. J Korean Ophthalmol Soc. 2015; 56:285–90.
Article4). Kim BO, Jin KH, Kwak HW. Retinal vessel obstruction caused by orbital compression after paranasal sinus surgery. J Korean Ophtalmol Soc. 1995; 36:130–4.5). Lim HW, Ko BW, Song Y, et al. Combined central retinal vein and artery occlusion after retrobulbar anesthesia: A case report. J Korean Ophtalmol Soc. 2008; 49:1013–7.
Article6). Koh JS, Woo SJ. Central retinal artery occlusion after trauma: Report of two cases. J Korean Ophthalmol Soc. 2016; 57:324–9.
Article7). Risk factors for central retinal vein occlusion. The Eye Disease Case-Control Study Group. Arch Ophthalmol. 1996; 114:545–54.8). Richards RD. Simultaneous occlusion of the central retinal artery and vein. Trans Am Ophthalmol Soc. 1979; 77:191.9). Durukan AH, Akar Y, Bayraktar MZ, et al. Combined retinal artery and vein occlusion in a patient with systemic lupus erythematosus and antiphospholipid syndrome. Can J Ophthalmol. 2005; 40:87–9.
Article10). Hamann S, Johansen S. Combined central retinal artery and vein occlusion in Churg-Strauss syndrome: case report. Acta Ophthalmol Scand. 2006; 84:703–6.
Article11). Schaible ER, Golnik KC. Combined obstruction of the central retinal artery and vein associated with meningeal carcinomatosis. Arch Ophthalmol. 1993; 111:1467–8.
Article12). Smith JL. Acute blindness in early syphilis. Arch Ophthalmol. 1973; 90:256–8.
Article13). Stowe GC 3rd, Zakov ZN, Albert DM. Central retinal vascular occlusion associated with oral contraceptives. Am J Ophthalmol. 1978; 86:798–801.
Article14). Singh NKK, Bhattacharya UK, Kamai GL, Fanai VR. Traumatic optic neuropathy with combined central retinal artery occlusion (CRAO) and central retinal vein occlusion (CRVO) following blunt ocular trauma. J Med Soc. 2014; 28:128.
Article15). Noble MJ, Alvarez EV. Combined occlusion of the central retinal artery and central retinal vein following blunt ocular trauma: a case report. Br J Ophtalmol. 1987; 71:834–6.
Article16). Cumurcu T, Doganay S, Demirel S, Cankaya C. Traumatic optic neuropathy and central retinal artery occlusion following blunt ocular trauma. J Clin Med Res. 2011; 3:55–7.
Article17). Scheerlinck TA, Van den Brande P. Post-traumatic intima dissection and thrombosis of the external iliac artery in sportsman. Eur J Vasc Surg. 1994; 8:645–7.18). Hayreh SS. Occlusion of the central retinal vessels. Br J Ophthalmol. 1965; 49:626.
Article19). Keane JR. Cavernous sinus syndrome. Analysis of 151 cases. Arch Neurol. 1996; 53:967–71.
Article20). Lenzi GL, Fieschi C. Superior orbital fissure syndrome. Review of 130 cases. Eur Neurol. 1977; 16:23–30.21). Garland SD, Maloney PL, Doku HC. Carotid-cavernous sinus fistula after trauma to the head. J Oral Surg. 1977; 35:832–5.22). Lew H, Lee SY, Jang JW, et al. The effects of high-dose corticosteroid therapy on optic nerve head blood flow in experimental traumatic optic neuropathy. Ophthalmic Res. 1999; 31:463–70.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Orbital Apex Syndrome and Central Retinal Vein Occlusion after Blow-out Fracture Repair
- A Case of Cilioretinal Artery Occlusion Associated with Central Retinal Vein Occlusion
- Incomplete Central Retinal Artery Occlusion
- Retinal Changes in a Patient with a Traumatic Orbital Subperiosteal Hematoma and Superior Ophthalmic Vein Compression
- The Successful Treatment of a Case of Central Retinal Artery Occlusion