Korean Circ J.
2018 Mar;48(3):179-190. 10.4070/kcj.2017.0393.
Functional Approach for Coronary Artery Disease: Filling the Gap Between Evidence and Practice
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Heart Vascular Stroke Institute, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Medicine, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 3Department of Medicine, Keimyung University Dongsan Medical Center, Daegu, Korea.
- 4Department of Cardiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 5Division of Cardiology, Dietrich Bonhoeffer Hospital, Academic Teaching Hospital of University of Greifswald, Greifswald, Germany.
- 6Department of Internal Medicine and Cardiovascular Center, Seoul National University Hospital, Seoul, Korea. bkkoo@snu.ac.kr
- 7Institute on Aging, Seoul National University, Seoul, Korea.
- KMID: 2406921
- DOI: http://doi.org/10.4070/kcj.2017.0393
Abstract
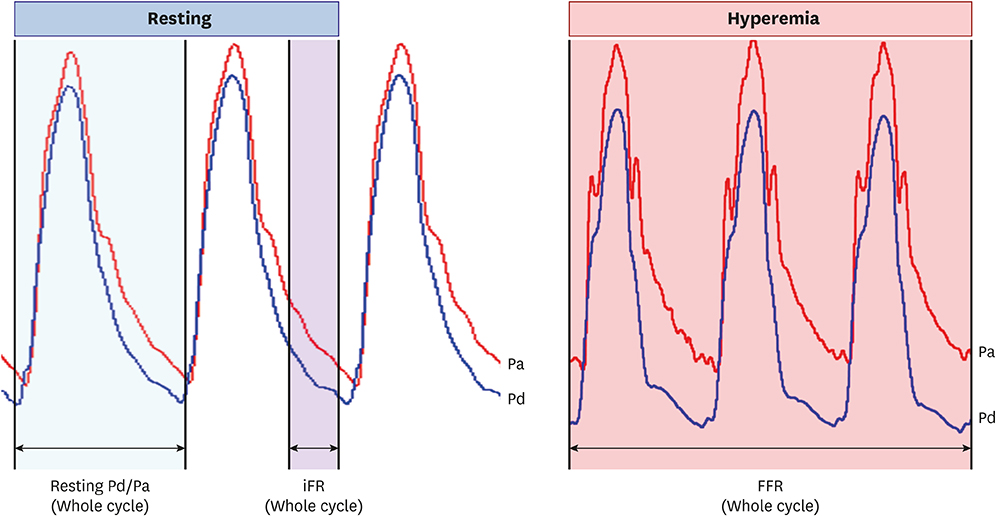
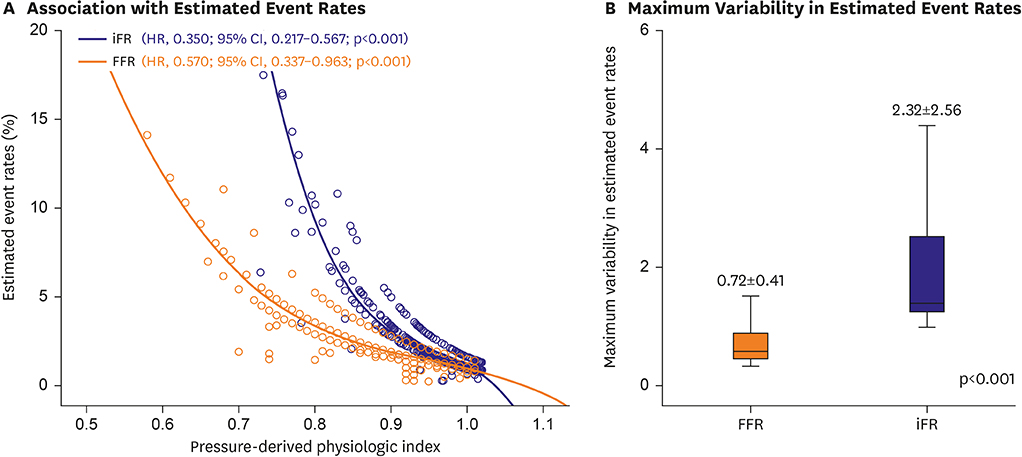
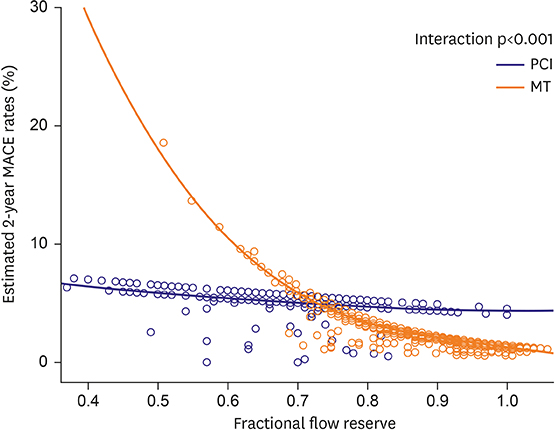
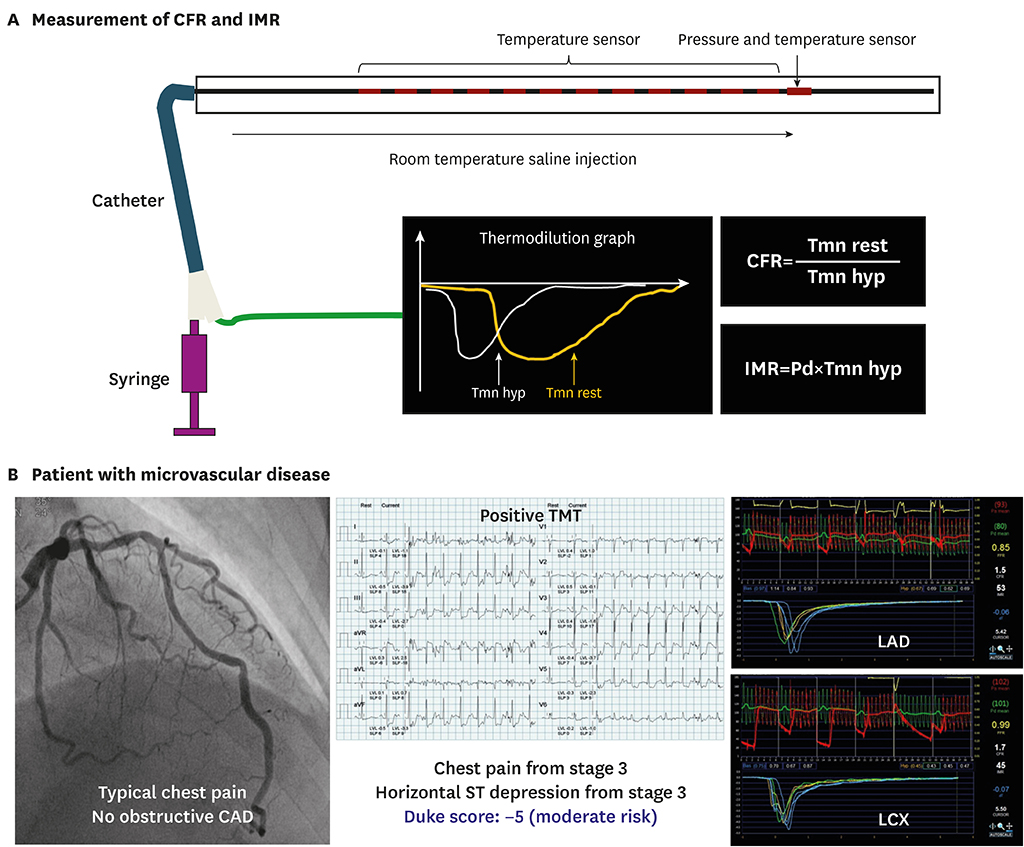
- The presence of myocardial ischemia is the most important prognostic factor in patients with coronary artery disease, and ischemia-directed revascularization has been a standard of care. Fractional flow reserve (FFR) is an invasive method used to detect the functionally significant epicardial coronary stenosis, and FFR-guided revascularization strategy has been proven to be superior to angiography-guided strategy. Recently, a hyperemia-free index, instantaneous wave free ratio (iFR), was developed and showed its non-inferiority for clinical outcomes compared with FFR-guided strategy. While evidence supporting the benefit of pressure wire assessment exists, there remain several unresolved issues, such as the mechanism of discordance between resting and hyperemic physiologic indices, clinical outcomes of patient/lesions with discordant results among the physiologic indices, role of physiologic indices beyond per-vessel decision tool, and the role of microvascular dysfunction in patient prognosis. The current article will review the recent studies performed to address these questions.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Coronary Physiology-Based Approaches for Plaque Vulnerability: Implications for Risk Prediction and Treatment Strategies
Seokhun Yang, Bon-Kwon Koo
Korean Circ J. 2023;53(9):581-593. doi: 10.4070/kcj.2023.0117.Diagnostic Performance of On-Site Automatic Coronary Computed Tomography Angiography-Derived Fractional Flow Reserve
Doyeon Hwang, Sang-Hyeon Park, Chang-Wook Nam, Joon-Hyung Doh, Hyun Kuk Kim, Yongcheol Kim, Eun Ju Chun, Bon-Kwon Koo
Korean Circ J. 2024;54(7):382-394. doi: 10.4070/kcj.2023.0288.
Reference
-
1. Iskandrian AS, Chae SC, Heo J, Stanberry CD, Wasserleben V, Cave V. Independent and incremental prognostic value of exercise single-photon emission computed tomographic (SPECT) thallium imaging in coronary artery disease. J Am Coll Cardiol. 1993; 22:665–670.
Article2. Hachamovitch R, Berman DS, Kiat H, Cohen I, Friedman JD, Shaw LJ. Value of stress myocardial perfusion single photon emission computed tomography in patients with normal resting electrocardiograms: an evaluation of incremental prognostic value and cost-effectiveness. Circulation. 2002; 105:823–829.
Article3. Iskander S, Iskandrian AE. Risk assessment using single-photon emission computed tomographic technetium-99m sestamibi imaging. J Am Coll Cardiol. 1998; 32:57–62.
Article4. Lin GA, Dudley RA, Lucas FL, Malenka DJ, Vittinghoff E, Redberg RF. Frequency of stress testing to document ischemia prior to elective percutaneous coronary intervention. JAMA. 2008; 300:1765–1773.
Article5. Patel MR, Peterson ED, Dai D, et al. Low diagnostic yield of elective coronary angiography. N Engl J Med. 2010; 362:886–895.
Article6. Levine GN, Bates ER, Blankenship JC, et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention. A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011; 58:e44–e122.7. Kolh P, Windecker S, Alfonso F, et al. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS). Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur J Cardiothorac Surg. 2014; 46:517–592.8. Zimmermann FM, Ferrara A, Johnson NP, et al. Deferral vs. performance of percutaneous coronary intervention of functionally non-significant coronary stenosis: 15-year follow-up of the DEFER trial. Eur Heart J. 2015; 36:3182–3188.
Article9. Park SH, Jeon KH, Lee JM, et al. Long-term clinical outcomes of fractional flow reserve-guided versus routine drug-eluting stent implantation in patients with intermediate coronary stenosis: five-year clinical outcomes of DEFER-DES Trial. Circ Cardiovasc Interv. 2015; 8:e002442.
Article10. Tonino PA, De Bruyne B, Pijls NH, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009; 360:213–224.
Article11. van Nunen LX, Zimmermann FM, Tonino PA, et al. Fractional flow reserve versus angiography for guidance of PCI in patients with multivessel coronary artery disease (FAME): 5-year follow-up of a randomised controlled trial. Lancet. 2015; 386:1853–1860.
Article12. Patel MR, Calhoon JH, Dehmer GJ, et al. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 appropriate use criteria for coronary revascularization in patients with stable ischemic heart disease: a report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol. 2017; 69:2212–2241.13. Davies JE, Whinnett ZI, Francis DP, et al. Evidence of a dominant backward-propagating “suction” wave responsible for diastolic coronary filling in humans, attenuated in left ventricular hypertrophy. Circulation. 2006; 113:1768–1778.
Article14. Siebes M, Kolyva C, Verhoeff BJ, Piek JJ, Spaan JA. Potential and limitations of wave intensity analysis in coronary arteries. Med Biol Eng Comput. 2009; 47:233–239.
Article15. Götberg M, Christiansen EH, Gudmundsdottir IJ, et al. Instantaneous wave-free ratio versus fractional flow reserve to guide PCI. N Engl J Med. 2017; 376:1813–1823.16. Davies JE, Sen S, Dehbi HM, et al. Use of the instantaneous wave-free ratio or fractional flow reserve in PCI. N Engl J Med. 2017; 376:1824–1834.17. Berry C, van't Veer M, Witt N, et al. VERIFY (VERification of Instantaneous Wave-Free Ratio and Fractional Flow Reserve for the Assessment of Coronary Artery Stenosis Severity in EverydaY Practice): a multicenter study in consecutive patients. J Am Coll Cardiol. 2013; 61:1421–1427.18. Park JJ, Petraco R, Nam CW, et al. Clinical validation of the resting pressure parameters in the assessment of functionally significant coronary stenosis; results of an independent, blinded comparison with fractional flow reserve. Int J Cardiol. 2013; 168:4070–4075.
Article19. Sen S, Asrress KN, Nijjer S, et al. Diagnostic classification of the instantaneous wave-free ratio is equivalent to fractional flow reserve and is not improved with adenosine administration. Results of CLARIFY (Classification Accuracy of Pressure-Only Ratios Against Indices Using Flow Study). J Am Coll Cardiol. 2013; 61:1409–1420.20. Jeremias A, Maehara A, Généreux P, et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: the RESOLVE study. J Am Coll Cardiol. 2014; 63:1253–1261.21. Lee JM, Hwang D, Park J, et al. Exploring coronary circulatory response to stenosis and its association with invasive physiologic indexes using absolute myocardial blood flow and coronary pressure. Circulation. 2017; 136:1798–1808.
Article22. Lee JM, Hwang D, Park J, Tong Y, Koo BK. Physiologic mechanism of discordance between instantaneous wave-free ratio and fractional flow reserve: insight from 13N-ammonium positron emission tomography. Int J Cardiol. 2017; 243:91–94.23. Cook CM, Jeremias A, Petraco R, et al. Fractional flow reserve/instantaneous wave-free ratio discordance in angiographically intermediate coronary stenoses: an analysis using doppler-derived coronary flow measurements. JACC Cardiovasc Interv. 2017; 10:2514–2524.24. Lee JM, Shin ES, Nam CW, et al. Discrepancy between fractional flow reserve and instantaneous wave-free ratio: clinical and angiographic characteristics. Int J Cardiol. 2017; 245:63–68.
Article25. Lee JM, Shin ES, Nam CW, et al. Clinical outcomes according to fractional flow reserve or instantaneous wave-free ratio in deferred lesions. JACC Cardiovasc Interv. 2017; 10:2502–2510.26. Lee JM, Park J, Hwang D, et al. Similarity and difference of resting distal to aortic coronary pressure and instantaneous wave-free ratio. J Am Coll Cardiol. 2017; 70:2114–2123.27. Curzen N, Rana O, Nicholas Z, et al. Does routine pressure wire assessment influence management strategy at coronary angiography for diagnosis of chest pain?: the RIPCORD study. Circ Cardiovasc Interv. 2014; 7:248–255.28. Van Belle E, Rioufol G, Pouillot C, et al. Outcome impact of coronary revascularization strategy reclassification with fractional flow reserve at time of diagnostic angiography: insights from a large French multicenter fractional flow reserve registry. Circulation. 2014; 129:173–185.29. Van Belle E, Baptista SB, Raposo L, et al. Impact of routine fractional flow reserve on management decision and 1-year clinical outcome of patients with acute coronary syndromes: PRIME-FFR (insights from the POST-IT [Portuguese Study on the Evaluation of FFR-Guided Treatment of Coronary Disease] and R3F [French FFR Registry] integrated multicenter registries - implementation of FFR [Fractional Flow Reserve] in routine practice). Circ Cardiovasc Interv. 2017; 10:e004296.
Article30. Ahn JM, Yoon SH, Roh JH, et al. Trends in outcomes of revascularization for left main coronary disease or three-vessel disease with the routine incorporation of fractional flow reserve in real practice. Am J Cardiol. 2015; 116:1163–1171.
Article31. Johnson NP, Tóth GG, Lai D, et al. Prognostic value of fractional flow reserve: linking physiologic severity to clinical outcomes. J Am Coll Cardiol. 2014; 64:1641–1654.32. Lee JM, Koo BK, Shin ES, et al. Clinical implications of three-vessel fractional flow reserve measurement in patients with coronary artery disease. [Epub ahead of print]. Eur Heart J. 2017.
Article33. Lee JM, Koo BK, Shin ES, et al. Clinical outcomes of deferred lesions with angiographically insignificant stenosis but low fractional flow reserve. J Am Heart Assoc. 2017; 6:e006071.
Article34. Park J, Lee JM, Koo BK, et al. TCT-67 clinical relevance of functionally insignificant moderate coronary artery stenosis assessed by 3-vessel fractional flow reserve measurement. J Am Coll Cardiol. 2017; 70:B29.
Article35. Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med. 2007; 356:830–840.
Article36. Toth G, Hamilos M, Pyxaras S, et al. Evolving concepts of angiogram: fractional flow reserve discordances in 4000 coronary stenoses. Eur Heart J. 2014; 35:2831–2838.
Article37. Lee JM, Layland J, Jung JH, et al. Integrated physiologic assessment of ischemic heart disease in real-world practice using index of microcirculatory resistance and fractional flow reserve: insights from the International Index of Microcirculatory Resistance Registry. Circ Cardiovasc Interv. 2015; 8:e002857.
Article38. Kobayashi Y, Lee JM, Fearon WF, et al. Three-vessel assessment of coronary microvascular dysfunction in patients with clinical suspicion of ischemia: prospective observational study with the index of microcirculatory resistance. Circ Cardiovasc Interv. 2017; 10:e005445.
Article39. Wessel TR, Arant CB, McGorray SP, et al. Coronary microvascular reactivity is only partially predicted by atherosclerosis risk factors or coronary artery disease in women evaluated for suspected ischemia: results from the NHLBI Women's Ischemia Syndrome Evaluation (WISE). Clin Cardiol. 2007; 30:69–74.
Article40. Yong AS, Ho M, Shah MG, Ng MK, Fearon WF. Coronary microcirculatory resistance is independent of epicardial stenosis. Circ Cardiovasc Interv. 2012; 5:103–108. S1–S2.
Article41. Lanza GA, Crea F. Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation. 2010; 121:2317–2325.42. Meuwissen M, Chamuleau SA, Siebes M, et al. The prognostic value of combined intracoronary pressure and blood flow velocity measurements after deferral of percutaneous coronary intervention. Catheter Cardiovasc Interv. 2008; 71:291–297.
Article43. van de Hoef TP, van Lavieren MA, Damman P, et al. Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv. 2014; 7:301–311.
Article44. Lee JM, Jung JH, Hwang D, et al. Coronary flow reserve and microcirculatory resistance in patients with intermediate coronary stenosis. J Am Coll Cardiol. 2016; 67:1158–1169.
Article45. Sen S, Escaned J, Malik IS, et al. Development and validation of a new adenosine-independent index of stenosis severity from coronary wave-intensity analysis: results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) study. J Am Coll Cardiol. 2012; 59:1392–1402.46. Petraco R, Escaned J, Sen S, et al. Classification performance of instantaneous wave-free ratio (iFR) and fractional flow reserve in a clinical population of intermediate coronary stenoses: results of the ADVISE registry. EuroIntervention. 2013; 9:91–101.
Article47. Petraco R, Al-Lamee R, Gotberg M, et al. Real-time use of instantaneous wave-free ratio: results of the ADVISE in-practice: an international, multicenter evaluation of instantaneous wave-free ratio in clinical practice. Am Heart J. 2014; 168:739–748.
Article48. Escaned J, Echavarría-Pinto M, Garcia-Garcia HM, et al. Prospective assessment of the diagnostic accuracy of instantaneous wave-free ratio to assess coronary stenosis relevance: results of ADVISE II International, Multicenter Study (ADenosine Vasodilator Independent Stenosis Evaluation II). JACC Cardiovasc Interv. 2015; 8:824–833.49. Hennigan B, Oldroyd KG, Berry C, et al. Discordance between resting and hyperemic indices of coronary stenosis severity: the VERIFY 2 Study (a comparative study of resting coronary pressure gradient, instantaneous wave-free ratio and fractional flow reserve in an unselected population referred for invasive angiography). Circ Cardiovasc Interv. 2016; 9:e004016.
Article50. Johnson NP, Jeremias A, Zimmermann FM, et al. Continuum of vasodilator stress from rest to contrast medium to adenosine hyperemia for fractional flow reserve assessment. JACC Cardiovasc Interv. 2016; 9:757–767.51. Nijjer SS, de Waard GA, Sen S, et al. Coronary pressure and flow relationships in humans: phasic analysis of normal and pathological vessels and the implications for stenosis assessment: a report from the Iberian-Dutch-English (IDEAL) collaborators. Eur Heart J. 2016; 37:2069–2080.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fractional Flow Reserve: The Past, Present and Future
- Functional Assessment of Coronary Artery Disease With Fractional Flow Reserve
- Direct Visualization of Coronary Artery and Flow using Transthoracic Doppler Echocardiography
- Ischemia-based Coronary Revascularization: Beyond Anatomy and Fractional Flow Reserve
- Ischemia-guided Revascularization for Stable Ischemic Heart Disease